Neuro-CNS/PNS
advertisement

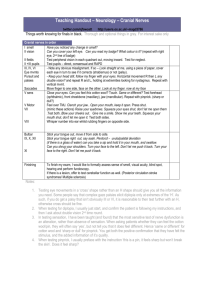
Teaching Handout – Neurology – Peripheral Nervious System twitter.com/njfawcett http://users.ox.ac.uk/~magd3786 Things worth knowing for finals in black. Thorough and optional things in grey. For interest sake only Examination of myotomes Shoulder abduction (deltoid) Elbow flexion (biceps/brachioradialis) Elbow extension (triceps) Wrist Extension (ECRL) Finger Extension (long/short extensors) Finger abduction (dorsal interossei) Hip flexion (iliopsoas) Knee Extension (quadriceps) Knee Flexion (hamstrings) Ankle DF (tibialis anterior) Ankle PF (gastrocnemius/soleus) C5 C6 C7 C7 C8 T1 L1/2 L3/4 L5/S1 L4/5 S1 Arms up, keep them up Pull me towards you / fist to your shoulder Push me away Arms out, cock your wrists back, keep them up Fingers out strong Push against my finger Lift your leg up, keep it up Kick your foot to the ceiling Knees bent, heel towards your bottom Toes up to the ceiling Push down on my hand This is a myotomal examination. Should your initial inspection/tone/myotomal power testing suggest a possible peripheral nerve lesion, only then it would be appropriate to go on to assess individual nerves ( median, ulnar, radial, common peroneal, tibial etc) otherwise move on. 1. Immobilise the joint your are testing 2. Compare same movement on both sides 3. Ideally test using a muscle group of similar power to that you are testing Muscle power should be tested as power at a static position, resisting movement (rather than range of movement). Instructions to the patient should focus on achieving this. Hence, ‘cock your wrists back, don’t let me push them down’ is a better test than ‘push your wrists back against my hand’ – for some reason, people are able to ‘resist’ more strongly and reliably than producing an active movement. (Though some movements are rather difficult to describe in this way). Try it yourself. In testing sensation, I have been taught (and found) that the most sensitive test of nerve dysfunction is an alteration, rather than absence of sensation. When asking patients whether they can feel the cotton wool/pin, they will often say ‘yes’, but not tell you that it does feel different. Hence ‘same or different’ for cotton wool and ‘sharp or dull’ for pinprick. You get both the positive confirmation that they have felt the stimulus, and the added information of it’s quality. When testing pinprick, I usually preface with the instruction ‘this is a pin, it feels sharp but won’t break the skin’. Does it feel sharp? Patterns of Neurological Compromise Descriptive LMN UMN Bilateral Unilateral Symmetrical Asymmetrical Distal Proximal Motor Sensory Mixed Deficit Level Myopathy NMJ Peripheral Neuropathy Peripheral Merve lesion (s) Plexopathy Radiculopathy Cauda equina Spinal cord lesion/Myelopathy Brainstem lesion Cortical lesion Patterns of deficit Corticospinal – UMN, pyramidal motor deficit Anterior Horn Cells – LMN motor deficit (eg. polio) Dorsal column – light touch, vibration, proprioception Spinothalamic – pain, temperature Peripheral nerves – sensorimotor deficit Peripheral Neuropathy Common Metabolic Paraneoplastic Infiltrative Drug-Induced Mononeuropathy External Compression Internal Compression Intrinsic lesion Diabetes, B12 Deficiency Diabetes, B12/folate, alcohol Lung, Ovarian, lymphoma, ENT/Adenocarcinoma Amyloid, Sarcoid Amiodarone, Chemotherapy- Vinca-Alkaloids(vincristine), Velcade (Bortezolemib) Trauma, prolonged compression (eg. Coma) Entrapment (eg. Carpal tunnel), tumors Inflammation (usually part of a polyneuropathy/ MNM Vasculitic (SLE, Rheumatoid, ANCA associated) infiltrative (Amyloid, Sarcoid) Failure to repair (metabolic) and minor compression - Diabetic microvascular disease, alcohol, B12 Common Peroneal Nerve Palsy Causes Trauma/Compression at fibula (crossing legs!) Acute mononeuritis - Diabetes, Vasculitis Predisposition to pressure palsy/neuropathy - Diabetes, B12 deficiency, Alcohol, Hypothyroidism Inspector Morse with his foot drop - most common lower limb nerve mononeuropathy THINK PERONEAL COMPARTMENT (which is lateral calf) Motor – weakness of dorsiflexion, and eversion and toe extension but *sparing of inversion* Sensory changes – lateral calf and dorsum Ankle jerk preserved (S1 via tibial nerve) Differentials of foot drop L4L5 radiculopathy – but would involve medial sensory calf sensory change Sciatic Nerve (more extensive motor/sensory deficit) Peripheral neuropathy - glove/stocking sensory loss Mononeuritis Multiplex Common Diabetes Vasculitis Systematic Infection Infarction Inflammation Infiltration Iatrogenic Neoplastic Congenital Metabolic Hormonal Lyme, Hep B, Hep C, HIV -Vasculitic - SLE, Rhematoid, ANCA associated Amyloid, Sarcoid Amiodarone, Chemotherapy (vincristine, thalidomide), Ethambutol Lymphoma, myeloma Charcot Marie Tooth Diabetes, B12, CKD, liver disease Hypothyroidism Multifocal Motor Neuropathy Is Acquired inflammatory demyelinating polyneuropathy affecting the motor axons. Produces a LMN bilateral asymmetrical predominantly distal pure motor neuropathy, usually involving the upper limbs. Muscle wasting and fasciculation are often absent. (In finals if you (are unlucky enough to) get this, the only thing you will be expected to do is localise this to a LMN lesion affecting the motor system, and suggest a few semi-sensible LMN pathologies and initial investigations) Management Full Hx and Ex to establish diagnosis and effect of the condition. Investigations include looking for other causes, using nerve conduction studies, MR imaging of the cord and nerve roots, and blood tests for condition such as diabetes and the vasculitides. LP may show oligoclonal bands in the CSF and there is an association with anti-GM1 IgM Treatment is multidisciplinary. (OT, physio, social/community/group support) Medical treatment involves immunomodulation with regular IVIG infusions. Differentials: Amyotrophic Lateral Sclerosis (ALS/Motor Neurone Disease – but this has UMN signs) Plexopathy/Diabetic Amyotrophy Causes of Mixed UMN and LMN signs General Motor Neurone Disease Two pathologies Look for Bulbar signs (eg. Cord compression and peripheral nerve compression) Syringomelia (expanding central canal, usually cervical) Early spinothalamic tract pain/loss of pinprick. LMN wasting and weakness of small muscles from early ventral root compression. UMN spasticity from corticospinal tract involvement late in disease course Absent ankle jerks and upgoing plantars Caused by damage to corticospinal tracts (plantars) and peripheral nerve damage (loss of ankle jerks) Subacute Combined Degeneration of Cord 2 pathologies Taboparesis 2’ neurosyphilis Friedrichs ataxia Look for autoimmune disease, dementia Eg. Cord compression + diabetic neuropathy Charcot joints, Argyll Robertson pupils Skeletal deformity, cerebellar signs Causes of UMN signs General Cord / Myelopathy Intracranial Compression: Disc Trauma Tumor (primary or metastatic) Degeneration (spondylosis)/ (AA subluxation in Rheumatoid) Abscess Inflammation – multiple sclerosis Infarction - anterior spinal artery infarction Mass lesion Tumor - Primary (meningioma, astrocytoma, glioblastoma) Tumor - Secondary Infarction – stroke – haemorrhagic or ischaemic Inflammation – MS Infection – encephalitis, meningitis Autoimmune – autoimmune/paraneoplastic encephalopathies Degeneration – frontotemporal dementias, other Hydrocephalus Tumors that metastasise to bone 5 ‘B’s - most rubbish mnemonic ever Breast Bronchus Bidney (kidney) Byroid (thyroid) Brostate (prostate)