Neurology Block Integration Lecture
advertisement

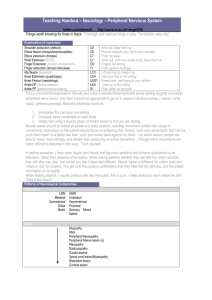
Neurology Block Integration Lecture Localization in Clinical Neurology Remember: The Goal of Neurology in Unit III To produce a medical student entering clerkship with a sufficient knowledge of neurology to identify and treat neurologic conditions that are Common Serious Dr. Heather MacLean Common, Serious or Both • • • • • • • • • • • Tumors Stroke Subarachnoid Hemorrhage Head and Spinal trauma Parkinson’s Disease Wilson’s Disease Huntington’s Disease ALS Sciatica Carpal Tunnel Syndrome Diabetic Polyneuropathy Guillain Barre Myasthenia Gravis Multiple Sclerosis Meningitis HSV Encephalitis Migraines Tension Headaches Cluster Headaches Epilepsy Sleep disorders What are the 3 Golden Questions in Neurology? 1. 2. 3. Is it neurological? Where is the lesion? What is the lesion? The tools we have given you to answer those questions… NeuroAnatomy NeuroPathology NeuroPhysiology Answers To Golden Trio NeuroRadiology Clinical Neurology NeuroAnatomy Probably more than any other specialty, Neurology REQUIRES a working knowledge of relevant anatomy It is the key to an accurate localization Know your NeuroAnatomy Organized by Regions… Dr. Heather MacLean And Organized by Systems Eg: the motor system Muscle NMJ Nerve Dr. Heather MacLean Elements of the Motor System UMN Pyramidal Tract (aka Direct Pathway) “Other” Tracts (aka Indirect Pathway) LMN NMJ Muscle Diseases at Each Level Where in the Motor System is the Lesion? (UMN,LMN,NMJ,Muscle) 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Myasthenia gravis (MG) Dermatomyositis (DM) Myotonic Dystrophy (MD) Spinomuscular Atrophy (SMA) Amyotrophic Lateral Sclerosis (ALS) Guillain Barre Syndrome (GBS) Multiple Sclerosis (MS) Left MCA stroke Left Occipital Lobe Tumor Benign Rolandic Epilepsy of Childhood L3/4 disc protrusion causing L4 distribution sciatica C6 vertebral fracture causing a complete traumatic myelopathy 1. 2. 3. 4. 5. NMJ Muscle Muscle LMN UMN & LMN 10. LMN UMN (if the motor is affected!) UMN Neither! UMN 11. LMN (L4 motor root) 12. UMN (CSTs) and LMN (Anterior Horn Cells at level of C6 only) 6. 7. 8. 9. The Pyramidal Tract – UMN Pathway For Voluntary Movement UMN Syndrome vs. LMN Syndrome UMN Syndome LMN Syndrome weakness yes muscle bulk fasciculations normal muscle tone stretch reflexes clonus plantar reflex none increased hyperactive present upgoing (Babinski) Dr. Heather MacLean yes wasting yes decreased hypoactive absent downgoing Regarding the motor system, very important to know spinal anatomy… Corticospinal tract location, decussation and ‘somatotopic organization’ Anterior horn cells Segmentation of spinal cord Spinal Cord Segmentation Spinal Myotomes Root innervation of muscles Important Myotomes: C5, C6, C7, C8/T1 Innervate most of the arms L4, L5, S1 Innervate most of the legs …AND need to know the very complicated Brainstem Where the CSTs run in the Midbrain Pons Medulla Which CN’s have motor functions/nuclei How to clinically differentiate between UMN and LMN facial weakness LMN Facial Weakness Regarding the Motor System, you must know the other 2 Circuits that modulate Movement… Dr. Heather MacLean Elements of the Somatosensory System Cutaneous Receptors Peripheral Nerves Dorsal Roots & Dorsal Root Ganglia 2 main sensory pathways Spinothalamic tract (STT) Dorsal Column Medial Lemniscal pathway Both synapse in the contralateral thalamus on the way to sensory cortex Cortical Sensation Aka corticosensory testing 2 point discrimination Graphesthesia Stereognosis Dermatomes Root innervation of skin Important Dermatomes: C5,C6, C7,C8 T4 (nipple line) T10 (umbiliculus) L4, L5, S1 The Visual System Normal Anatomy of Vision VF Defects Depending on Lesion Location Autonomic nervous system Control of unconscious, visceral functions Sympathetic system Pupils Tearing Salivary glands Breathing Heart rate Blood pressure Stomach, intestines, gall bladder Bladder, sex organs Sweat glands, piloerector muscles Adrenal glands Fight and flight responses Thoracolumbar levels Parasympathetic system Resting, vegetative functions Craniosacral levels Dr. Heather MacLean Higher Cognitive Functions Neglect Anosognosia Language Left (dominant) hemispheric control Analogue in the right (non-dominant) hemisphere affects emotional aspects of language Memory Declarative Semantic Episodic Non-declarative (procedural) Transient Global Amnesia A temporary, largely anterograde memory defect Clinical Neurology You must recognize patterns Contralateral if hemispheric Hemibody (face=arm=leg) Optic nerves Medial Longitudnal fasciculus Basal ganglia Brainstem Dipoplia, dysarthria, vertigo Crossed sensory deficits Ipsilateral incoordination Dysarthria, vertigo, nystagmus Motor & Sensory areas affected depend on specific nerve involved if mononeuroapthy Symmetric length dependent glove & stocking sensory loss if polyneuropathy NMJ Hyper or hypokinetic sx/signs Cerebellum Symmetric Sensory level Motor level, UMN findings below this Impaired bladder & bowel Peripheral neuropathy White matter pathology Differential involvement of face&arm >leg or leg> arm&face Seizures Sometimes headache Sometimes dementia Spinal lesions Contralateral Cortical homunculus Gray matter pathology Fatiguable Face and Eye involvement Only motor Myopathy Symmetric Proximal muscles usually Only motor You need to systematically Create a Differential Diagnosis Congenital Traumatic Metabolic Infectious, Inflammatory, Iatrogenic Neoplastic Degenerative Stroke, seizure, sleep disorder Vascular Psychogenic Dr. Heather MacLean Let’s put our skills to the test… Case 1 Mr. Brown is a 60 year old right handed auto mechanic who has been referred for neck pain. He has had posterior neck pain intermittently for 10 years but for the past 6 months it has been nearly constant. 3 weeks ago after shovelling his driveway following a heavy snowfall the pain in his neck started radiating into his right shoulder and arm and his right lateral forearm and thumb have become numb and tingly. He also now finds his legs feel rubbery and weak when he walks and he has had new problems with urination. His stream is hesitant and he never seems to be able to completely empty his bladder. Localize this lesion by history Key symptoms: Is his pain and numbness due to a central (CNS) cause? Radiating pain from neck to right arm Strip of numbness/paresthesias involving right thumb Bilateral leg weakness Bladder hesitancy No. Although central lesions often produce numbness, they very less frequently cause pain. To have a “strip” of numbness would be unusual from a cortical source (think of the homunculus) and would be nearly impossible from a subcortical source (think how close the sensory fibres are in the internal capsule and how tiny that lesion would need to be!) In the PNS, does this fit with a root problem or a nerve problem? Let’s look at this further… Nerve Sensory Innervation of the Hand Median nerve First 3 ½ fingers (conting from thumb) SPLITS the ring finger He has mainly the thumb Involved, not first 3 ½ fingers And his numbness spreads Up higher than the wrist – Doesn’t fit with median nerve Dermatomes C5 C6 fits nicely Thumb C7 Anterior Shoulder Middle Finger C8 “Pinky” Radicular (root) Pain in the Arm C5 C7 C5 C6 C8 C6 C8 BLACK= Pain, STIPPLED= Numbness/tingling Radicular Pain in the Leg S1 S1 L5 L5 L4 L4 BLACK= Pain, STIPPLED= Numbness/tingling Dermatomes vs. Nerve Sensory Innervation in the Leg Comparison More Questions Case 1 Can his bilateral leg weakness and bladder symptoms be explained by a C6 radiculopathy? Where do these symptoms localize to? No Keys to a Spinal cord lesion are symmetric bilateral motor involvement of legs (paraparesis) and bladder dysfunction Let’s see if his physical exam confirms your suspicion... Case 1 continued On examination he appeared in moderate discomfort but was pleasant and able to give a concise history. Mental status, language and cranial nerve examinations were normal. Motor examination of the arms demonstrated atrophy and weakness of the right biceps (mild), brachioradialis and wrist extensors (more pronounce). Shoulder abduction and finger abduction and adduction were normal. Fasciculations were seen in the right brachioradialis muscles. Motor examination of the legs revealed spasticity and mild weakness of bilateral hip flexors, knee flexors and ankle dorsiflexors. The extensors of the legs seemed strong. Sensory exam of the left arm was normal. In the right arm, pin prick and fine touch were reduced in the lateral forearm & thumb. You test temperature sensation and he has a definite bilateral sensory level on the anterior trunk. Pulling out your dermatome chart, you think it is between the C5 & T1 levels. Simple as 1,2,3 Myotomes L4,5 S1,2 Biceps (mostly C5) Elbow flexion, semipronated (brachioradialis) Wrist extension L4 Elbow extension (triceps) C8/T1 Hand intrinsics Knee extension L5 C7 Shoulder abduction, biceps C6 L3,4 C5 L2,3 Ankle dorsiflexion, ankle inversion and ankle eversion S1 Ankle plantarflexion Case 1 continued Tests of coordination/cerebellar function were done well. Left biceps and brachioradialis reflexes were normal. The right biceps reflex was present but reduced, the right brachioradialis reflex was absent. His triceps, knee jerks and ankle jerks were bilaterally brisk and he had bilaterally upgoing plantar responses. Root Innervation of Reflexes As simple as counting 1,2,3 Our case And even more questions Case 1 Does this support a myelopathic process? Yes How do you get a C6 radiculopathy and a myelopathy? What is the lesion? Degenerative Disc Disease (Mini)Case 2 You are on call for neurology and you hear a stroke code being called overhead. You rush to the ER where Mrs. White is being assessed by the ERP and is surrounded by nurses taking blood and getting an ECG. The ERP tells you she is an 80 year old woman with a past history of HTN who suddenly developed right-sided numbness 1 hour ago. There is no headache, neck pain or apparent sensory loss. You take over and examine her. She is alert and oriented and speaks normally. Vision is normal. There is dense numbness involving the right face, arm and leg to pinprick, temperature and fine touch but all strength testing seems normal. Coordination and reflexes are normal. She can walk without assistance. Pure sensory loss Where is the lesion? CNS or PNS? Brain or spinal cord? Definitely not cerebellum (motor control) No other brainstem sx or signs (diplopia, dysarthria, dysphagia, vertigo, crossed sensory findings) Probably cerebrum Which hemisphere? Brain, hemisensory not sensory level Cerebrum, brainstem or cerebellum? CNS Left Cortex, white matter, thalamus or basal ganglia? Not BG (motor control) Cortex less likely as would have to involve a HUGE cortical surface area to equally involve face, arm and leg, yet sparing any adjacent motor cortex or language area of the Left hemisphere??? IMPOSSIBLE! Likely thalamus which functions as a huge sensory relay or retrolenticular part of the the internal capsule which carries thalamic radiations to cortex. What is the lesion? Remember CT MIND SVP Sudden onset, no ‘march’ to suggest seizure (seconds) or migraine (minutes) No hx of trauma or infectious symptoms Negative symptoms (sensory loss) rather than positive (tingling) seen in seizure or migraine Older woman with HTN, stroke risk factor Lacunar infarction of the left thalamus Think lacune if stroke presents with Pure hemisensory or pure hemimotor signs, Especially if F=A=L distribution! Minicase 3 A 35 year old female nurse notes that, at the end of her shifts, she has difficulty enunciating her words, producing a smile, and even holding her head up. Her symptoms disappear with rest. On prolonged upgaze she develops ptosis of the left eyelid. While reading a long passage aloud, her speech gradually becomes dysarthric. The rest of neuro exam including sensory exam, strength, tone, bulk and reflexes are normal. There are no fasciculations. Based on this history, where is the lesion? Note: Brainstem Anterior horn cells Multiple cranial neuropathies Multifocal white matter (eg: MS) Neuromuscular junction 1. 2. 3. 4. 5. no UMN signs no atrophy/fasics/LMN signs no sensory abnormalities the fatiguability Dysarthria – can be UMN, cerebellar, LMN of CN 7, 9/10, 12 , NMJ or myopathy of face/tongue Facial weakness – can be UMN or LMN CN7, NMJ or myopathy of face/tongue Ptosis -- can be LMN CN3 lesion or Horner’s syndrome, NMJ or myopathy affecting eyes Neck weakness – UMN or LMN CN11, NMJ or myopathy Recall your patterns! Keys here are pure motor symptoms, fatiguability and eye and face involvement What is the lesion? MG is the most common NMJ disorder Fits clinically with her presentation Minicase 4 A 68 year old man was walking from his bathroom at 10am when he suddenly developed an explosive headache. It is the “worst headache of my life”. It began in the bifrontal area and over the next few minutes spread all over his head and down his neck. He denies nausea, vomiting, LOC or vision changes. He is a heavy smoker and has CAD. Minicase 4 continued What is the single most important diagnosis to rule out based on this history 1. 2. 3. 4. Meningitis Encephalitis Subarachnoid hemorrhage Intracerebral hemorrhage If SAH, what ‘extra’ neurologic sign do you need to look for on exam? 1. 2. 3. 4. Nuchal rigidity Straight leg raising Dix-Hallpike maneuvre Relative afferent pupillary defect What investigation(s) should be ordered next? CT head then LP if negative If a SAH is proven cerebral angiogram Dr. Heather MacLean