CRYSTAL-INDUCED ARTHRITIS
advertisement

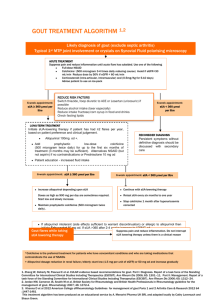
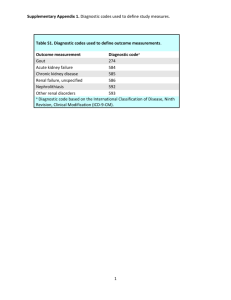
Arthritis in the Elderly “All the Pearls in 50 Minutes” Gerald F. Falasca, M.D. Johnson City, TN March 2013 GOALS • Practical advice • Up to date on mgt • Hone diagnostic skills DISEASES To Be Touched On • • • • • Sjogren’s PMR DJD RA Gout CASE 1 • A 70 year old woman presents with widespread pain, stiffness and fatigue. She recently started keeping a water bottle at her bedside. Physical exam is remarkable for slight synovitis of hands & wrists, and presence of all fibromyalgia tender points. CASE 1 – cont’d. • Sed rate is 30 mm/hr but CRP is normal CRP at 0.7 mg/dl (nl 0 - 1.0 mg/dl) • C4 ↑ at 36 mg/dl. • RF, CCP & ANA are negative. CASE 1 – cont’d. What is the most likely diagnosis? A. Polymyalgia rheumatica B. Rheumatoid arthritis C. Fibromyalgia D. Primary Sjogren syndrome E. Paraneoplastic syndrome Causes of Pain All Over in the Elderly • • • • • • • • Polymyalgia rheumatica Statins Fibromyalgia Depression Sjogren’s Rheumatoid Lupus Osteoarthritis Primary Sjogren’s • • • • • Dry eyes, dry mouth Fatigue Pain all over No idea what is wrong with them You probably have some in your practice Sjogren’s - History • Use of eye drops? • Can you eat crackers w/o water? • Keep water on night table? • Physical Exam: Nothing specific! – Sometimes small joint puffiness – Peripheral neuropathy Sjogren’s - Lab • SSA / SSB – insensitive • ESR often up • CRP high normal Sjogren’s - TX • • • • Hydroxychloroquine Low-dose prednisone Methotrexate Rituximab • Fibromyalgia treatments (for symptoms) Polymyalgia Rheumatica • 10-15% go on to GCA • Respond well to treatment • In other words, this is a potentially serious disease that is treatable. PMR • • • • Pain all over; sudden onset. Age > 50 (usually >70!) Weight loss Shoulder limitation of motion (periarthritis) • Proximal muscle tenderness • Sed rate > 50 mm/hr • Anemia PREDNISONE in ELDERLY • • • • • ↓K+, ↑glucose DEXA Calcium + Vit D T/C bisphosphonate Eye exams: cataracts & pressure Amer. College of Rheum. • Recommendations for the Prevention and Treatment of Glucocorticoid-Induced Osteoporosis 2010 • Arthritis Care & Research, Vol. 62, No. 11, November 2010, pp 1515– 1526 • DOI 10.1002/acr.20295 GOUT The risk factors for gout were known to the ancients. Risk Factors for Gout • • • • • Obesity, metabolic syndrome Ethanol Diuretics Fructose ingestion Excessive purine ingestion Ben Franklin (1706 -1790) "Be temperate in wine, in eating, girls, and sloth, or the Gout will seize you and plague you…" -- Franklin Drugs Associated with Hyperuricemia • Diuretics (loop and thiazide types) • Low-dose aspirin • Ethanol Hyperuricemia & Gout Serum Uric Acid (mg/dl) < 7.0 Annual Incidence of Gout (%) 0.1 7.0 – 8.9 0.5 > 9.0 4.9 This is chronic refractory gout! Amer. College of Rheum. • Guidelines for Management of Gout. Part 1 & 2 • Arthritis Care & Research, Vol. 64, No. 10, October 2012, pp 1431– 1461 • DOI 10.1002/acr.21773 The Three Phases of Gout Treatment • Treat acute attack • Prevent new attacks • Reduce uric acid level (sometimes) Phase 1 - Termination • • • • • NSAID Colchcine Intra-articular steroids Systemic steroids IL-1 inhibitor (off-label use) NSAIDs • Treatment of choice in otherwise healthy (elderly?) patient. • Avoid in renal insufficiency and in peptic ulcer disease. • Avoid salicylates (these cause swings in serum uric acid). Intra-Articular Steroids • One or a few joints. • Make sure infection not present. Oral Colchicine • 1.2 mg followed by 0.6 mg 2 hrs later. • Loading dose same in renal insufficiency. • Maintenance (preventive) dose 0.6 mg qd or bid. • 0.3 mg 2-3 times per week in dialysis patients (preventive). Systemic Steroids • • • • • Polyarticular attacks or fever. Longstanding attacks (>3-5 days). Need divided doses. Taper over 7-10 days. Start prophylactic agent (colchicine) as soon as possible. Adjunctive Measures • • • • • Rest Ice Elevation Analgesics Anti-motility agents (if using colchicine or indomethacin) • Continue hypouricemic agent if patient has been taking it. Phase 2 - Preventive Therapy • Colchicine or NSAID. • Always use when beginning a hypouricemic drug. • Continue several weeks to years (depending on tophi, serum uric acid). • Always use before surgery in previously gouty patient. Phase 3 - Hypouricemic Therapy • Not every patient needs it. • May not need it in: – Very elderly – Non-compliant – Infrequent attacks and no tophi • May exacerbate attacks early on Goals of Hypouricemic Treatment • Aim for serum uric acid under 6, preferably near 5 for some chronic gouty patients. • But remember: – allopurinol toxicity more likely with higher dose. – More likely with renal insufficiency. Hypouricemic Agents • • • • • • Allopurinol Febuxostat Probenecid Losartan (off-label) Vitamin C (off-label) Pegloticase Major Toxicities of Allopurinol • Increased gout attacks early on (use prophylaxis) • Rash (may be severe) • Stevens-Johnson syndrome • Vasculitis • Hepatitis • Renal failure (interstitial nephritis) • Bone marrow suppression Allopurinol Hypersensitivity Syndrome • Fever • Rash • Renal Failure • Hepatic injury • Leukocytosis • Eosinophilia (the tipoff!) • May be fatal. Hard to treat. • Serious reactions to allopurinol reported in 1 of 260 patients. Arthritis Rheum 29:82, 1986 Febuxostat • Non-xanthine inhibitor of XO and XD. • Better tolerated than allopurinol. • Lower uric acid levels than allopurinol (53% vs. 21% met target of 6.0 mg/dl). • Better dissolution of tophi. Tophus Reduction Mean Reduction in Tophus Area Group % Area Reduction P Value Feb 80 mg 83 P = .08 (NS) Feb 120 mg 66 P = 0.16 (NS) Allop 300mg 50 Becker MA. N Engl J Med. 2005 Dec 8;353(23):2450-61. Febuxostat compared with allopurinol in patients with hyperuricemia and gout. Febuxostat vs. Allopurinol Percentage of Patients Achieving Serum Uric Acid < 6 mg/dl Study 1: Allopurinol dosed at 300 mg/d for ClCr ≥ 60 ml/min or 200 mg/d for 30 ≤ ClCr ≤ 59 ml/min. Febuxostat: Best Use • Allopurinol failures • Renal insufficiency • Tophaceous gout Allopurinol & Febuxostat Drug Interactions • Life threatening interaction with azathioprine, 6-mercaptopurine. – Reduce dose of purine analogue by approximately 2/3. • Theophylline • Other interactions also Gout vs. Pseudogout • Gout – hallux, ankle, knee, hand – younger, male • Pseudogout – knee, wrist, ankle – older, female • Almost any joint can be affected by either disease! CPPD Deposition • Wrist: triangular ligament • Pelvis: symphysis pubis • Knee: menisci • Also: annulus fibrosis, articular capsules, bursae, ligaments, tendons Clinical Associations with Psuedogout • Aging • Previous joint surgery • Previous joint trauma • Familial types • Gout • Amyloidosis • • • • Hyperpara Hemochromatosis Hypomagnesemia Familial hypocalciuric hypercalcemia • Hypophosphatasia • Wilson’s disease • Ochronosis Pseudo-DJD Pattern of CPPD • 50% of CPPD patients. • Wrists, MCPs, elbows, shoulders, knees. Note difference from usual DJD pattern. • Heberden’s or Bouchard’s frequently found. • May be acute or chronic. Treatment of Acute Psuedogout • Aspiration (more important than in gout!) • Rest • Intra-articular steroids • NSAIDs • Systemic steroids • Colchicine? • IL-1 Inhibitors? Pseudogout Prevention • • • • Colchicine NSAID Magnesium? There’s no allopurinol for pseudogout (unfortunately). The Basic (Non-Acidic) Calcium Phosphates • • • • Hydroxyapatite Calcium carbonate Octacalcium phosphate Tricalcium phosphate (whitlockite) • Hydroxyapatite is nonbirefringent. Syndromes Associated with Hydroxyapatite • Acute monoarthritis (pseudopseudogout) • Acute calcific tendinitis, bursitis • Scleroderma, dermatomyositis • Heterotopic calcification • Milwaukee shoulder • Crowned Dens Synd. Acute Apatite Monoarthritis (Pseudopseudogout) • Is usually a peri-arthritis. • Intense inflammation (looks septic) • Synovial fluid often noninflammatory. • Often causes podagra (especially in younger women). • Look for the telltale calcifications on radiographs. CROWNED DENS SYNDROME Crowned Dens Synd • • • • Headache Pain with head rotation Shoulder myalgias Very elevated sed rate RHEUMATOID ARTHRITIS In the Elderly Rheumatoid • Even in the elderly, completely new paradigm of treatment. • Dual goals: – Symptom improvement – Prevention of structural damage Rheumatoid • “Small joint polyarthritis with morning stiffness” • MCPs, wrists, MTPs • ESR, CRP may or may not be up. • RF or anti-CCP pos 70% RA in the Elderly • M:F ratio more nearly equal • More shoulder involvement • May overlap with polymyalgia rheumatoica Initial Tx of RA • Low dose prednisone (actually a good DMARD!) • Methotrexate – safer than we expected in 1987! – Lung toxicity is possible – Follow liver enzymes – Added infection risk is relatively low (2-3%). What We Try to Prevent The New Paradigm • Is it likely that the patient will have destructive or debilitating disease in the long-term? • If so, begin one or more DMARDs (often MTX). • If inadequate response after 3 months, add or switch DMARDs, often includes a TNFI. Anti-CCP • CCP = cyclic citrullinated peptides • RA synovium overproduces CCP • RA patients THEN make ANTIBODIES to CCP • 70% sensitive, 90% specific • Anti-CCP is often present years before RA manifests itself. Goals of the New Criteria • Identify persons with “early arthritis” who are at high risk of erosive or debilitating disease. • Allow for earlier disease modifying treatment. • But…the criteria are not simple! 2010 ACR/EULAR CRITERIA FOR CLASSIFICATION OF RHEUMATOID ARTHRITIS Arthritis & Rheumatism 62(9): 2569–2581, 2010. Lab Eval of Polyarthritis • • • • • • • Rheum factor Anti-CCP ANA C4 Lyme CBC Chem-12 • SSA, SSB • Anti-RNP Methotrexate • • • • Standard of care for RA. dihydrofolate reductase inhibitor. Best initial treatment for most patients. Avoid in pre-existing liver disease, renal disease and in drinkers. • Main risk: pulmonary toxicity • Higher doses being used, espec. Sub Q. • 1/3 of patients will have little or no radiographic progression on MTX alone. Methotrexate (cont’d) • Always give only once a week, but dose may be split in two parts, and given 12 hours apart. • Most persons should receive supplemental folate 1 mg/d. • Follow liver enzymes (with albumin), CBC, creatinine monthly initially. Methotrexate - Side Effects • • • • • • Nausea, diarrhea Stomatitis Alopecia Rash Infections MTX pneumonitis • • • • • Hepatitis Cirrhosis Pulm. fibrosis Pancytopenia Lymphoma? • Don’t use if creatinine > 2.0! TNF Inhibitors • Potent inhibitors of inflammation • Have revolutionized the treatment of RA since 1998. • They retard erosions • Act quickly • Two approaches: monoclonal Ab vs. soluble receptor • $$$$ Side Effects of TNF Inhibitors • • • • Rashes, especially inject. site rxns. Infections. Reactivation of tuberculosis. Demyelinating disease, optic neuritis, seizures. • Pancytopenia. • Congestive heart failure (effect may last for months). • Malignancy (espec. lymphoma) Prednisone • Low dose prednisone: 7.5 mg/d • Reduces number of erosions at two years in early RA (22% vs. 46%). • N Engl J Med 1995 Jul 20;333(3):142-6. Remission: The New Standard? • Durable remissions are achievable with combination therapy. • Definition of remission important however! • Remission depends heavily on treating early (first year of disease) • New trials may report the remission rate as the primary outcome measure RA Take Home Messages • The treatment paradigm has changed in the past 10-15 years. • Aggressive treatment changes long-term outcome. • The earlier treatment is started, the better. • There are new tools to help us make an earlier diagnosis. Osteoarthritis • Everyone gets a little • Minor degenerative changes on xray often meaningless • Knee, 1st CMC, DIPs, hip, back • Usually localized – Exception: Erosive or inflammatory OA. Nonpharmacologic Therapy for Patients with OA Amer. Coll. Of Rheumatology • Patient education Self-management programs (e.g., Arthritis Foundation Self-Management Program) Personalized social support through telephone contact Weight loss (if overweight) Aerobic exercise programs Physical therapy Range-of-motion exercises Muscle-strengthening exercises Assistive devices for ambulation Patellar taping Appropriate footwear Lateral-wedged insoles (for genu varum) Bracing Occupational therapy Joint protection and energy conservation Assistive devices for activities of daily living http://www.rheumatology.org/practice/clinical/guidelines/oa-mgmt.asp Pharmacologic Therapy for Patients with OA Amer. Coll. Of Rheumatology • Acetaminophen • COX-2-specific inhibitor • Nonselective NSAID [plus misoprostol or a proton pump inhibitor if at ↑GI risk] • Non-acetylated salicylate • Other pure analgesics: Tramadol • Opioids • Intraarticular glucocorticoids, hyaluronan • Topical Capsaicin Methylsalicylate http://www.rheumatology.org/practice/clinical/guidelines/oa-mgmt.asp OA of the Knee • Most sensitive and specific finding on physical exam: • CREPITUS! • Sometimes knee pain is coming from the hip OA of Knee • • • • • • Glucosamine: mixed data Corticosteroid injection Viscosupplementation Quadriceps exercises Neoprene sleeve Hinged brace OA of the Hip Joint • Mimicked by low back pain! • Most common cause of trochanteric bursitis is low back pain too! • Hip pain usually radiates to groin, not to the “hip”. Hip OA • Injections don’t last long and are not practical. • Hip replacement is a good operation. 1st CMC Osteoarthritis • • • • Brace off-the-shelf Brace custom molded Surgery Liniment NSAIDs Toxicity in Elderly • Peptic ulcer disease • Hypertension • Congestive heart failure • CNS changes • Intestinal ulceration GI Less Toxic NSAIDs • • • • • Celecoxib Salsalate Meloxicam Nabumetone Etodolac Risk Factors for UGI Events Amer. Coll. Of Rheumatology • • • • • Age >=65 Comorbid medical conditions Oral glucocorticoids History of peptic ulcer disease History of upper gastrointestinal bleeding • Anticoagulants http://www.rheumatology.org/practice/clinical/guidelines/oa-mgmt.asp RISK FACTORS FOR ULCERS • • • • • • • NSAID Use Age > 64 Prior event CHF Ethanol Warfarin Concomitant corticosteroid, low dose aspirin, bisphosphonate, SSRI • H. pylori PREVALENCE OF NSAID ULCERS BY AGE Ann Rheum Dis. 2007 March; 66(3): 417–418. PREVENTION OF NSAID ULCERS Arch Intern Med. 2002 Jan 8;162(2):169-75 NSAID ULCER PROPHYLAXIS • H2 blockers NOT recommended for prophylaxis • PPI or misoprostol recommended • PPI doesn’t seem to reduce celecoxib ulcer complications further. • Low dose aspirin ELIMINATES any benefit of celecoxib. Amer. Coll. Of Gastro. 2009 • Patients with hx PUD should be tested for H. pylori prior to NSAID or ASA use. Amer. Coll. Gastro. Guide. 2009 GI RISK High CV RISK* Mod Low High No NSAID, no COX-2 Naproxen + (PPI or MIS) Naproxen + (PPI or MIS) Low COX-2 + (PPI or MIS) COX-2 or (NSAID NSAID alone + (PPI or MIS)) *High CV risk defined as those needing aspirin therapy. Prophylactic Regimens • Misoprostol 200 mcg QID • Lansoprazole 15 or 30 mg/d • Esomeprazole 20 or 40 mg/d CV Risk - Celecoxib • • • • 33 months Placebo 200 mg BID 400 mg BID Abs 6/676 18/683 23/669 % 0.9% 2.6% 3.4% N Engl J Med. 2006;355(9):873. RR 1.0 2.6 3.4