Gout
advertisement

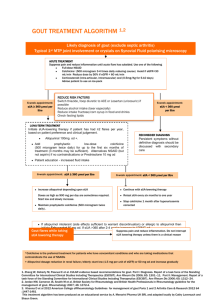
GOUT: DIAGNOSIS AND MANAGEMENT Gout Metabolic disorder due to excessive accumulation of uric acid in tissues leading to acute and chronic arthritis and soft tissue and bone deposition of uric acid (tophi). Acute Gouty Arthritis Abrupt 75% onset often at night of initial attacks in first MTP joint Usually monoarticular, may be polyarticular Attack Na+ subsides in 3-10 days urate crystals in synovial fluid Hyperuricemia present may or may not be The victim goes to bed and sleeps in good health. About 2 o’clock in the morning he is awakened by a severe pain in the great toe; more rarely in the heel, ankle or instep. The pain is like that of a dislocation, and yet the parts feel as if cold water were poured over them…Now it is a violent stretching and tearing of the ligaments – now it is a gnawing pain, and now a pressure and tightening. So exquisite and lively meanwhile is the feeling of the part affected, that it cannot bear the weight of the bedclothes nor the jar of person walking in the room. The night is spent in torture. - Thomas Sydenham (1624-1689) QUESTION: Who gets gout? ANSWER: Individuals with prolonged hyperuricemia So who gets hyperuricemia? Hyperuricemia Overproduction (10%) (80 % idiopathic) Ethanol HGPRT or G6PD deficiency PRPP synthetase overactivity Myeloproliferative disorders Hyperuricemia Underexcretion (90%) (80% idiopathic) Renal insufficiency Drugs and toxins –Diuretics –Ethanol –Cyclosporine A –Pyrazinamide –Lead nephropathy –Low dose aspirin Ketosis So who gets gout? Young and middle-aged men Individuals with hypertension, obesity,renal insufficiency, metabolic syndrome, organ transplants Patients on diuretics Beer drinkers Who doesn’t get gout? Women Unless Post-menopausal Renal insufficiency Chronic diuretic use Myeloproliferative disorder The prevalence of gout is increasing Patients with CHF and renal disease are surviving longer Obesity/metabolic syndrome epidemic More organ transplants Less estrogen used Low dose aspirin use GOUT: DIAGNOSIS Presentation Patient demographics Physical findings Differentiate from: Sepsis RA Spondyloarthropathy(psoriasis, reactive) Lyme GOUT: DIAGNOSIS Arthrocentesis and crystal identification Serum uric acid may be misleading and is not a good diagnostic test for acute gout. TREATMENT OF ACUTE GOUT NSAIDS Intra-articular steroids Prednisone Colchicine PO – no fun IV – be careful (limited availability) TREATMENT OF RECURRENT GOUT PO daily low-dose colchicine Colchicine neuromypathy Lower serum uric acid level TREATMENT OF HYPERURICEMIA: INDICATIONS Repeated or severe acute gout attacks Patient preference Tophaceous/erosive gout Chemotherapy of hematologic malignancies Nephrolithiasis Treatment of Hyperuricemia Decrease uric acid production Allopurinol Febuxostat (Uloric) Uricosuric agents Probenecid Sulfinpyrazone TREATMENT OF HYPERURICEMIA: ALLOPURINOL/FEBUXOSTAT Marked hyperuricemia Increased urinary uric acid excretion Tophaceous or erosive gout Renal insufficiency Nephrolithiasis TREATMENT OF HYPERURICEMIA: URICOSURICS Low urinary uric acid excretion Mild renal insufficiency (Probenecid, sulfinpyrazone) TREATMENT PEARLS Aspirin makes gout worse. Allopurinol/febuxostat is a treatment for hyperuricemia and not acute gout. Giving allopurinol or febuxostat during an acute attack will prolong the attack. Starting allopurinol/febuxostat may provoke attacks. Therefore add colchicine for 6-12 mos.




![06Gout_-_Copy[1].](http://s2.studylib.net/store/data/005758926_1-0d7c6513b0c82c14c18839741770ea53-300x300.png)