Childhood Leukemia
advertisement

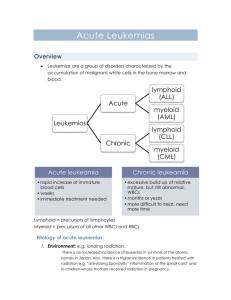
Childhood Leukemia Mary E. MacBlane MS, PNP-BC Goals Incidence Etiology Diagnosis Types/Classification Treatment Primary Care Pearls Incidence 30% of all cancers in childhood Peak incidence 2-5 years of age males > females Caucasian > African American Incidence of ALL (acute lymphoblastic leukemia) is 5 times higher than incidence than AML (acute myeloid leukemia) Etiology Exact cause is NOT known Genetics – – Identical twin with leukemia Chromosome abnormalities – Other Down Syndrome Severe Combined Immunodeficiency Neurofibromatosis Fanconi’s Anemia Bloom Syndrome Environmental – – – – Ionizing Radiation Chemotherapy Viruses Pesticides 5 – Year Survival 1960 – Less than 10% Today – – ALL: 80-85% AML: about 65% Why? – – Research Standardized treatment protocols COG Childrens Oncology Group International Organization Ongoing Studies – – – Chemo combinations & timing, radiation, etc… Quality of Life Epidemiology Standards of Care Treatment Protocols Nursing Discipline Shared Data Meetings Diagnosis: Symptoms Fatigue Pallor Anorexia Bruising/Bleeding Fever Bone/joint pain Belly pain H/A Diagnosis: Exam Findings Pallor Bruises Petechiae Lymphadenopathy Hepatosplenomegaly Cranial Nerve Palsies Testicular enlargement Chloromas Leukemia Cutis Mediastinal Mass Superior Vena Cava Syndrome Leukemia Cutis Petechiae Differential Diagnosis Viral Illness ITP Aplastic Anemia Arthritis Lupus Transient Erythroblastic Anemia of Childhood Other Malignancies Diagnostic Studies CBC Other – – – – – – Chemistries Uric Acid LFT’s LDH Viral Titers Chest x-ray CBC w/ Differential WBC’s – ↑ or ↓ Hgb ↓ Platelet Ct ↓ Diff – – Neutropenia Peripheral Blasts Types of Childhood Leukemia ALL – Acute Lymphoblastic Leukemia AML – Acute Myeloid Leukemia CML – Chronic Myeloid Leukemia Classification by Cell Lineage Acute Lymphocytic Leukemia (ALL) Most common cause of childhood leukemia Peak age: 2-5 years Males > females ALL – Best Prognosis Ages 1-9 Females Initial WBC < 10,000 Favorable cytogenetics Early response to treatment ALL –Poor Prognosis Ages < 1 year or > 10 years Initial WBC > 50,000 Extramedullary sites – – CNS Testes Steroid Pre-Treatment Unfavorable cytogenetics Lack of remission after induction treatment ALL - Cytogenetics Examples Favorable Unfavorable Hyperdiploid (extra chromosomes) Hypodiploid (fewer than 54 chromosomes) Trisomies 4, 10, 17 t(9;22) BCR/ABL translocation (Philadelphia chromosome) t (12;21) TEL-AML1 t(4;11) MLL rearrangement ALL - Risk Stratification Low Risk Average (Standard) Risk High Risk Very High Risk ALL Induction Therapy Lasts 35 Days Medications – – – – Intrathecal Medications weekly (Cytarabine or Methotrexate) Vincristine IV weekly Peg-Asparaginase on Day 4 28 days of steroids Examine peripheral blood for remission at Day 8 and Day 29 Bone marrow recheck at Day 29 Expect remission by the end of induction ALL - Phases of Treatment Induction (first month) Consolidation (1 month) Interim Maintenance I (2 months) Delayed Intensification (2 months) Interim Maintenance II (2 months) Maintenance – – 2 years for females 3 years for males Acute Myeloid Leukemia (AML) No Peak Age 20-25% of acute leukemia in children Overall prognosis about 65% AML – Favorable Prognosis Down syndrome Cytogenetics: t(8;21) t(15;17), inv 16 AML – Unfavorable Prognosis WBC > 100,000 at diagnosis Cytogenetics: t(9;11), 11q23 Therapy-related AML Lack of remission after induction AML – General Treatment Very Intensive Therapy – – Induction I and II Intensification I and II About 6 months Inpatient for most of therapy Bone Marrow Transplant High Risk ALL AML Complications of Leukemia Treatment Tumor Lysis Syndrome Infection/Sepsis Thrombosis Hemorrhage / DIC Leukostasis Infection Risk Central Lines Prolonged Neutropenia Immunocompromise after BMT Infection Risk Tidbits Alpha Strep Fungal PCP – – – Bactrim Dapsone Pentamidine Primary Care Diagnosis During Treatment Late Effects Monitoring for relapse Primary Care Pearls Diagnosis – – – – – – – History Exam CBC No Steroids Avoid Transfusion CXR Make the phone call Primary Care Pearls After Diagnosis – – General Care Immunizations – – Flu Shots No Live-Virus Vaccines Maintaining Normalcy and Hope Sibling Considerations Virus Varicella Flu Shots Primary Care Pearls Late Effects – – – – – Avascular necrosis Cardiotoxicity Neuro-cognitive Secondary malignancies Endocrine abnormalities Alert for Relapse Case Study 1 2 year old female brought to primary care provider Parents report a 1 week hx of fatique that has gotten worse; pain that began in her feet and progressed to legs; and a petechial rash over her arms and legs with some bruising. She had a brief episode of epistaxis on day prior to appointment. They also felt that her belly has seemed more prominent for the past 2 weeks. Primary provider obtained a CBC which revealed peripheral blasts Case Study 1 Initial labs at admission: CBC – WBC: 27,000 – – Blasts: 34% Neutrophils 1% Hgb: 4.9 (11.5-13.5) Platelets: 6,000 (150,000-400,000) Chemistries: – – – – – Uric Acid: 3.4 (2.4-5.7) Potassium: 3.9 (3.3-5.1) Creat: 0.2 (.2-.7) Bili: 0.2 (.1-1.0) LDH: 341 (120-300) Case Study 1 Treated following standard risk ALL protocol 2 unplanned admissions – – Both for fever and neutropenia On one admission found to have pneumonia Otherwise did well and completed therapy in 25 months Case Study 2 12 year old male with bulky lymphadenopathy, change in voice, difficulty breathing. Seen in local ED and prescribed 4 day course of prednisone Symptoms initially resolved but recurred and seemed much worse 3 days later (very hoarse voice, could not lay down flat to sleep) Again seen in ED and 5 day course of prednisone and then 4 day taper prescribed On last day of steroids there was a biopsy of a lymph node. 2 days later the primary care provider was notified that the results were consistent with T-cell leukemia. Case Study 2 Admitted to our facility with initial studies: CBC: – WBC: 58.6 Creatinine: 1.1 (0.5-1.2) Uric Acid: 8.3 (3.4-7.0) Chest x-ray reveals large mediastinal mass and tracheal deviation Case Study 2 High Risk T-Cell ALL Age – 12 years Initial WBC – 58,000 Pretreated with Steroids Already in tumor lysis Creatinine 1.1 Uric acid 8.3 Case Study 3 15 year male who moved to the US about 6 months earlier. He was seen in primary care office for routine well-child check. Only complaint was headache on and off for 2 weeks. Exam: nl except mild submandibular adenopathy CBC – WBC 6.8 – – 32% Blasts 9% Neutrophils Hgb 12.6 (13-17) Plt 308 Case Study 3 Admitted to the hospital and lumbar puncture and bone marrow completed Lumbar puncture: No evidence of malignancy Bone Marrow consistent with Acute Myeloid Leukemia with favorable cytogenetics: t(8,21) Case Study 3 Received 4 courses of chemotherapy over 4 admissions Admission #1 and #2 each lasted about 1 month. Received prophylactic antibiotics and antifungals. Occasional transfusions of packed cells and platelets Case Study 3 Admission 3: Lots of issues (1 month stay) – – – – Persistent fever despite prophylaxis. Had to change to treatment dose of meds. All cultures were negative throughout stay Ambisome for fungal coverage and then needed Amiloride to prevent potassium wasting Anorexia – Started periactin. Needed N-D tube for feeds Multiple transfusions of packed red blood cells and platelets Case Study 3 Admission 4: Over 6 weeks stay – – – – – – Persistent fever despite prophylaxis. Positive blood cultures for Staph hominis. Required Vanco and Zosyn for 10 days and then returned to prophylaxis. Ambisome again for fungal coverage. Required electrolyte supplementation (Magnesium, Potassium) in addition to Amiloride Anorexia – Periactin at first. Changed to Marinol. Tube feedings not tolerated. TPN required. C-diff infection. Treated with Flagyl Lip lesion positive for HSV-1 Multiple transfusions of packed red blood cells and platelets Case Study 3 Now doing GREAT! Returned to school Visits the clinic about every 6 weeks currently Thank You