Body Tissues
advertisement

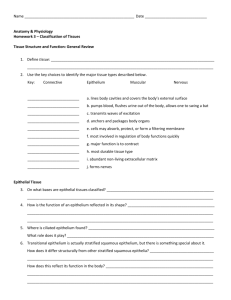
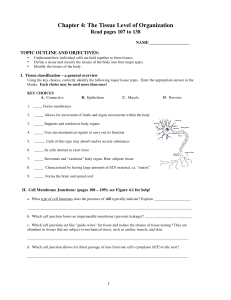
Body Tissues Chapter 3, Section 3 I. Tissues A. Definition: A group of cells that are similar in structure and function. B. Types 1. 2. 3. 4. Epithelium- Covering Connective Tissue- Support Nervous Tissue- Control Muscle- Movement 1. Epithelial Tissue (Epithelium)- Pg. 78, fig. 3.17 a. Definition: The lining, covering, and glandular tissue of the body. b. Functions: Protection, absorption, filtration, and secretion. c. Special Characteristics of Epithelium i. Epithelial cells fit closely together to form continuous sheets. Cells are bound together by cell junctions (desmosomes and tight junctions) i. The membranes always have one free surface or edge -This apical surface is exposed to the body’s exterior or toward a cavity. -Some apical surfaces are slick, while others have membrane modifications. iii. The lower surface of an epithelium rests on a basement membrane. -Basement membranes are structureless materials secreted by the cell. iv. Epithelial tissues are avascular (They have no blood supply) - They depend on diffusion from capillaries in underlying connective tissue. v. Epithelial cell regenerate easily when well-nourished. d. Classification of Epithelium i. Naming -Each epithelium is given 2 names – The first tells us the number of cell layers (simple= 1 layer, stratified= more than 1 layer) – The second tells us its shape (squamous= flattened, cuboidal= cubeshaped, and columnar= shaped like columns. ii. Types -Simple Epithelia are mostly concerned with absorption, secretion and filtration » Simple Squamous Epithelium is a single layer of flat cells that rest on a basement membrane. • Forms membranes where filtration occurs. (lungs) • Serous membranes are slick and line the ventral cavities. » Simple cuboidal epithelium is a single layer of cube-shaped epithelium that rests on a basement membrane. • Common in glands and their ducts. (Salivary glands, pancrea) » Simple Columnar Epithelium is made up of a single layer of tall cells. • Function: Absorption and secretion. • Goblet cells line the entire digestive tract and produce a lubricating mucous • Mucosae (Mucous Membranes) line body cavities that are open to the environment. » Pseudostratified Columnar Epithelium sit on a basement membrane, but due to varying length of the cells and location of the nuclei. They sometimes appear to be stratified. • Function: Absorption and secretion • Found in respiratory tract. -Stratified Epithelia consists of 2 or more cell layers and are mainly used for protection because of their durability. >>Stratified Squamous Epithelium is the most common stratified epithelium in the body. • Several layers. • Free edge made up of squamous cells and those close to the basement membrane are cuboidal or columnar. • Found in the esophagus, mouth, and outer integument where most friction/abuse occurs. » Stratified Cuboidal Epithelium usually has 2 cell layers with the surface cells being cuboidal. • Rare in the body, found mainly in ducts of large glands. » Stratified Columnar Epithelium have surface cells that are columnar, but basal cells vary in shape and size. • Rare in the body, found mainly in ducts of large glands. » Transitional Epithelium is highly modified, stratified squamous epithelium. • Forms lining of only a few organs. • All are part of the urinary system. • Subject to considerable amounts of stretching. • Cells at the basal layer are cuboidal or columnar. • Cells on the free surface vary. • When the organ is filled with urine, the tissue stretches and thins, making the cells appear to be squamous. – Glandular Epithelium » A gland is made of one or more cells that make and secrete certain products called secretions (proteins in water). • 2 types of glands *Endocrine Glands are ductless glands. They secrete hormones. -Secretions diffuse directly into blood vessels *Exocrine Glands retain ducts. Include sweat and oil glands. -Secretions empty through ducts to the epithelial surface 2. Connective Tissue-pg. 81, Fig. 3.18 a. Definition: Tissue that connects body parts. b. Where is it found? i. Everywhere! It is the most abundant and widespread tissue. c. Function: i. Protection, support, and binding other tissues together. d. Common Characteristics i. Variations in blood supply -Most connective tissue is vascularized. -Tendons and ligaments have a poor blood supply -Cartilage is avascular -Because of little or no blood supply, tendons, ligaments, and cartilages heal extremely slowly or don’t heal at all. ii. Extracellular Matrix -Connective tissues are made of many different types of cells plus varying amounts of extracellular matrix. >>Extracellular matrix is the nonliving substances outside the cells. >> Produced by connective tissue cells and secreted out. >>Extracellular matrix makes connective tissue durable enough to withstand stretching, abrasion, and other abuses. >>Fat tissue is mostly cells with a soft matrix, while cartilage has few cells and is strong with a hard matrix. -Fibers are also created and deposited in the matrix. >>Collagen (white), elastic (yellow), and reticular (fine) fibers. e. Types of Connective Tissue i. Bone (Osseous tissue) is made of bone cells. - These sit in cavities and secrete hard matrix made of calcium salts and large collagen fibers. Bone is great for protection and support. ii. Cartilage is less hard and more flexible than bone. -Not found in many places in the body. -The most abundant type is hyaline cartilage. >>Rubbery matrix with a glassy look • Larynx, ribs, joints. – Elastic Cartilage provides elasticity. » External Ear – Fibrocartilage is highly compressable » Cushionlike » Between vertebrae iii. Dense Connective Tissue (Dense Fibrous Tissue) has rows of fibroblasts surrounded by a collagen fiber matrix. -Forms strong, ropelike structures such as tendons and ligaments. >>Tendons attach skeletal muscle to bones. >>Ligaments attach bones to bones at joints. -Makes up the lower layers of the skin (dermis) iv. Loose Connective Tissue is soft and has more cells and fewer fibers than any other connective tissue besides blood. -Areolar Tissue cushions and protects the body organs it wraps. >>Holds the internal organs in place. >>Most of the matrix appears to be empty space. >>Provides a reservoir of water and salts for surrounding tissues • Most body cells get nutrients from this matrix • Soaks up excess fluid from an enflamed region, causing it to swell (edema). – Adipose Tissue » Commonly called fat. • It is areolar tissue where fat cells predominate. • Function: *Insulation, protection, fuel – Reticular Connective Tissue » Network of interwoven reticular fibers. » Forms an internal support framework » Can support many free blood cells in lymphoid organs. v. Blood – – – – Also known as vascular tissue. Blood cells are surrounded by a matrix of plasma Fibers are seen only during clotting Main function: Transport 3. Muscle Tissue a. Definition: Highly specialized cells that contract, or shorten, to produce movement. i. Since they are elongated, they are called muscle fibers. b. Types of Muscle Tissue i. Skeletal Muscle -Packaged by connective tissue sheets into skeletal muscles. -Can be controlled voluntarily and form the flesh of the body. -Pull on bones or skin when they contract. -Cells are long, cylindrical, and multinucleate -Have obvious striations (stripes) ii. Cardiac Muscle -Found only in the heart -Contractions force the heart to pump. -Striated, uninucleated, branching cells. -Fit tightly together, like clasping fingers, at junctions called intercalated disks. -Gap junctions here allow ions to pass freely from cell to cell, resulting in rapid conduction of electrical impulses across the heart. -Operate under involuntary control. iii. Smooth Muscle -Also known as visceral muscle. » No striations are visible. – Have a single nucleus and are spindle-shaped. – Found in the walls of hollow organs. – When it contracts, the cavity of an organ gets small (constricts) or enlarges (dilates) so substances can be propelled in a specific direction. » Contraction here is slower than with the other two muscle types. » Ex: Peristalsis is the wavelike motion that keeps food moving through the small intestines. 4. Nervous Tissue a. Made of neurons. i. All neurons receive and conduct electrochemical impulses. ii. Major functions: irritability and conductivity. iii. The cytoplasm is drawn out into long extensions, which allows a single neuron to conduct an impulse over long distances in the body. b. Other nervous tissue participants: i. Supporting cells: Special cells that insulate, support, and protect the neurons. -Supporting cells and neurons together make up the structures of the nervous system. II. Tissue Repair A. Prevention: 1. Physical barriers help to prevent the tissues from being harmed a. Skin, mucous membranes, cilia, stomach acid B. Response to Damage: a. Injury to tissue stimulates inflammatory and immune responses. i. Inflammation is a generalized body response that attempts to prevent further injury. ii. Immune responses are specific and mount attacks on recognized invaders (bacteria, viruses, toxins). C. Tissue Repair (Wound healing) occurs in two major ways: 1. Regeneration a. Replacement of destroyed tissue by the same type of cells 2. Fibrosis a. Repair by dense (fibrous) connective tissue. i. This is scar tissue. 3. When does each occur? a. Which occurs depends on i. Type of tissue damaged. ii. Severity of the injury. 4. Events in tissue repair i. Phase I -Capillaries become permeable, allowing certain substances to seep into the injured region. -Clotting proteins form a clot (hardens and forms a scab) • Stops blood loss, holds wound edges together, and blocks off the injured area. ii. Phase II -Granulation Tissue forms. • This is a delicate pink tissue made mostly of capillaries from undamaged nearby blood vessels. • These bleed freely and are fragile. • Contains phagocytes that eventually dispose of the blood clot and connective tissue cells (fibroblasts) that make collagen fibers (scar tissue) • Scar tissue permanently bridges the gap. iii. Phase III -Surface epithelium regenerates and makes its way across the granulation tissue. -When complete, the scar detaches. -Final Result = Fully regenerated surface epithelium + underlying area of fibrosis (scar). -Depending on the severity of the wound, the scar may not be visible. 5. Tissue types and Repair a. b. c. Epithelial tissues, fibrous connective tissues, and bone heal well. Skeletal muscle regenerates poorly, if at all. Cardiac muscle and nervous tissue are only replaced by scar tissue. i. Scar tissue is strong, but not very flexible. -It is also unable to perform the function of the tissues that it replaces, which can severely hamper the functioning of an organ. III. Developmental Aspects of Cells and Tissues A. Cell specialization occurs from fertilization to maturity. 1. Aging begins once maturity is reached. a. Some believe aging begins at birth. 2. After puberty is reached, many cell types stop dividing a. Only certain cells continue dividing routinely. i. Those that are exposed to routine wear and tear. b. Some cells only divide when absolutely needed. i. Liver cells c. Some stop dividing once maturity is reached. (Amitotic) i. Heart muscle and nervous tissue. ii. These are severely hampered by damage. B. What causes aging? 1. It is thought to be a result of chemical insults that occur during life. a. Toxins, lack of nutrients, exposure to radiation, etc. 2. 3. 4. 5. Partially due to genetics Gravity Less active endocrine/exocrine systems. Deterioration of connective tissue due to age (collagen) C. Other cellular modifications 1. Neoplasm a. Benign vs. malignant 2. Hyperplasia a. Enlarging of body tissues/organs due to irritants or medical conditions. i. Anemia 3. Atrophy a. Decrease in size due to loss of normal stimulation i.Lack of muscle use.