m5zn_2c3793c18b6e848
advertisement

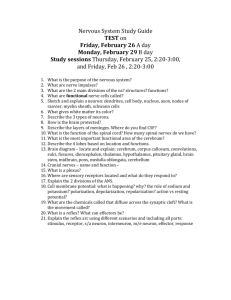
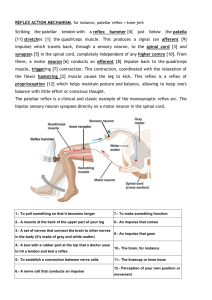
1-Anatomy,Histology and blood supply of the spinal cord. ( cover in lecture) 2-List Tracts (Sensory and motor) of the spinal cord and their functions.( cover in lecture) 3-Diffrentiate between an upper motor neuron lesion and a lower motor neuron lesion. 4-Examples of Spinal reflexes. 5-Describe spinal shock syndrome. 6-Describe various types of spinal cord injuries as regard to their etiologies,clinical features,pathogenesis,complications ,management and rehabilitation plans. 7-Explain the role of family and community in the management of rehabilitation of patient with spinal cord injury. 3) All the neurons contributing to the pyramidal and extrapyramidal systems should be called upper motor neurons (UMN). The anterior horn cells and the related neurons in the motor nuclei of some cranial nerves are called lower motor neurons (LMN). *Upper motor neuron lesions: Interruption of the corticospinal and corticonuclear tract along its course. *Clinical features of Upper motor neuron lesion: 1. Paralysis or weakness of movements of the affected side but gross movements may be produced. No muscle atrophy is seen initially but later on some disuse atrophy may occur. 2. Babinski sign is present: The great toe becomes dorsiflexed and the other toes fan outward in response to sensory stimulation along the lateral aspect of the sole of the foot. The normal response is plantar flexion of all the toes. 3. Loss of performance of fine-skilled voluntary movements especially at the distal end of the limbs. 4. Superficial abdominal reflexes and cremasteric reflex are absent. 5. Spasticity or hypertonicity of the muscles. 6. Clasp-knife reaction: initial higher resistance to movement is followed by a lesser resistance. 7. Exaggerated deep tendon reflexes and clonus may be present. lower motor neuron lesions: Degeneration of the motor neuron & peripheral nerves. Signs of Lower Motor Neuron Lesions (LMNL) 1. Flaccid paralysis of muscles supplied. 2. Atrophy of muscles supplied. 3. Loss of reflexes of muscles supplied. 4. Muscles fasciculation (contraction of a group of fibers) due to irritation of the motor neurons – seen with naked eye. 5. Muscle fibrillation (contraction of individual fibers) – detected only by EMG 6. Muscle contracture (shortening of paralyzed muscles) 7. Presence of muscle wasting 8. Reaction of degeneration: When the LMN is cut, a muscle will no longer respond to interrupted electrical stimulation 7 days after nerve section, although it will still respond to direct current. After 10 days, response to direct current also ceases. 4) Some examples of spinal reflexes: -stretch reflex: is a monosynaptic reflex that is a response to a muscle that has been stretched (the knee-jerk reflex is an example). When receptors in muscles, called muscle spindles, detect changes in muscle length, they stimulate, through a reflex arc, the contraction of a muscle. Stretch reflexes help maintain posture by stimulating muscles to regain normal body position. -flexor (withdrawal) reflex: is a polysynaptic reflex that causes a limb to be withdrawn when it encounters pain. -flexion and crossed extensor reflexes: a polysynaptic reflex step on sharp object cause a rapid lifting of affected foot while contralateral response activate the extensor. 5) *Spinal shock: A condition that can occur after spinal cord injury and involves a period of absent reflexes which may be permanent or last for hours to weeks. This period may be followed by a period of excessive reflexes. manifestation of spinal shock: 1)Loss of vasoconstrictor tone: if there is damage in descending fibres from vasoconstrictor centre to LHCs decreasing arterial blood pressure. 2)Bilateral Horner’s syndrome (e.g. ptosis, miosis, ..etc): if the lesion is in cervical region causes injury of descending fibres to LHCs of T1&2. 3)Loss of all reflexes below level of lesion: a. Superficial reflexes: are lost. b. Deep reflexes: loss of muscle tone (decreases body temperature) and loss of tendon jerks. c. Visceral reflexes: i. Micturition reflex: is lost and urination becomes by retention of u rine till overcomes internal uretheral sphincter’s resistance causing dribbling with overflow (retention with overflow) ii. Defecation reflex: is lost and defecation with retention with overfl ow. iii. Erection reflex: is lost with flaccid penis. 4) Bed sores and ulcers in the gluteal region and back due to: a. Sluggish circulation due to loss of vasoconstrictor tone with stagnan t hypoxia and skin becomes cold and cyanotic. b. Loss of the voluntary movement with prolonged pressure and worse circulation. c. Absent withdrawal protective reflex. Mechanism for Spinal Shock; The mechanism for spinal shock involves the sudden loss of conduction in the spinal cord as a result of the migration of potassium ions from the intracellular to extracellular spaces. This is associated with a transient loss of somatic and automatic reflex activity below the level of spinal cord segment damage. The spinal cord reflex arcs that are immediately above the injury may also be severely disrupted. Early Stages of Spinal Shock: Spinal shock following a spinal cord injury results in flaccid paralysis, areflexia and anaesthesia below the level of injury. The return of the reflexes indicates the end of spinal shock. Assessment of the end of spinal shock is based on the return of reflexes, with the bulbocavernosus reflex typically being the first to return. However, some clinicians may classify the end of spinal shock as the return of deep tendon reflexes or the return of reflexive detrusor function, which may be months after injury. Return of Reflexes Following Spinal Shock: Return of reflexes between 1-12 months post injury are characterised by hyper-reflexia, or abnormally strong reflexes usually produced with minimal stimulation. Inter neurons and lower motor neurons below the SCI begin sprouting, attempting to re-establish synapses. The first synapses to form are from shorter axons, usually from inter neurons - later changes are soma-mediated, and will take longer for the soma to transport various growth factors, including proteins, to the end of the axon.