Appendectomy - VCU Department of Surgery
advertisement

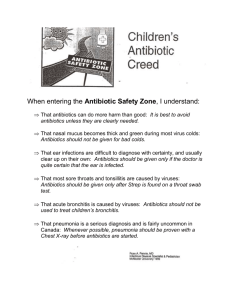
VCU Department of Surgery Death & Complications Conference Michelle Hamel, PGY-5 11/13/14 • Operation: Laparoscopic Appendectomy • Indication: Acute Appendicitis • Complication: Readmission, pelvic phlegmon formation, bacteremia Clavien-Dindo Classification Case Presentation • HPI: 44 y/o AA male presented to ED c/o 1 day h/o bilateral LQ abdominal pain, urinary urgency and tenesmus. Associated with nausea and emesis, which started at the same time as the pain. No fevers. Currently hungry. Normal BM yesterday and still passing flatus. Case Presentation • PMH: DM, HTN, CKD, Sleep apnea, obesity, gout, diabetic retinopathy • PSH: none • SH: Denies tob, EtOH or illicits. Married. Works as a restaurant manager. • FH: DM, HTN, kidney disease Case Presentation • Medications: Glipizide, ASA, atorvastatin, allopurinol, amlodipine, gabapentin • PE: – – – – – – Vitals: T 37.5; HR 79; BP 174/103; Sats 99%RA BMI 40 GEN: NAD, non-toxic RESP: CTAB CV:RRR ABD: soft, obese, tender in RLQ/suprapubic region, non-distended. +Rovsing’s sign, Voluntary guarding in RLQ Case Presentation • Labs: • WBC 8.4 / Hgb 11 / Plt 293 • Na 135 / K 4.7 / Cl 104 / Bicarb 22 / BUN 61 / Creat 3.93 / Glucose 109 • LFTs, Amylase, Lipase WNL CT Abd/Pelvis Case Presentation • CT abd/pelvis: Calcification within the base of the cecum with fat stranding distal to this and a non-visualized appendix; findings concerning for a ruptured appendix with associated appendicolith Case Presentation • Patient taken to OR and underwent laparoscopic appendectomy • Appendix gangrenous in midportion with tip scarred to the bladder, indicating possible longstanding inflammation • Midportion of appendix broke and appendix was removed piecemeal after stapling base of appendix • No associated abscess or gross spillage Case Presentation • On POD 1, WBC was 10.1, pt was afebrile and tolerating diet • Pt was d/c home • Pathology: Acute necrotizing appendicitis with serositis Case Presentation • Pt returned to ED on POD 7 c/o bilateral LQ abdominal pain and nausea. Subjective fevers at home. Normal BM that am. No emesis. • Febrile to 102, WBC 11.5 • Non-toxic appearing and abdomen tender in bilat LQ with no peritoneal signs. CT abdomen/pelvis Case Presentation • CT abd/pelvis: Developing pelvic abscess with fluid collections and locules of free air Case Presentation • Patient was admitted and started on IV zosyn. • No drainable fluid collections • Clinical improvement with antibiotics and WBC normalized, inpatient for additional 5 days • Blood cultures positive for bacteroides • Sensitivities demonstrated bacteria resistant to zosyn, sensitive to flagyl • Per ID recommendations, pt d/c home on 2 week course of cipro/flagyl • Our patient received antibiotics just prior to incision, and no post operative antibiotics • Should our patient have received postoperative antibiotics in setting of complicated appendicitis? • 45 randomized controlled trials including 9,576 adult & pediatric patients comparing effect of antibiotic treatment vs placebo for appendectomy, including wound infection and intraabdominal abscess • Preoperative or postoperative antibiotic treatment significantly decreased the wound infection and intraabdominal abscess formation Weaknesses of study • Many studies from 70s and 80s – Definition of intraabdominal abscess = persistent fever with no source, palpable mass in RLQ, purulent rectal drainage • No comparison of preoperative vs postoperative antibiotics • Included adults and children • No recommendations for type or length of course of antibiotics • Smaller number of patients with complicated appendicitis • *Has been standard of care to treat patients with complicated appendicitis with postoperative antibiotics • Retrospective review of 52 patients from 2007-2012 at EVMS • No significant difference in postoperative abscess formation in patients receiving <24H or >24H of antibiotics in complicated appendicitis • Small, retrospective study Conclusions • Current standard of care to give postoperative antibiotics for complicated (perforated, gangrenous appendicitis or with associated abscess) • Course and optimal regimen remain to be defined Analysis of Complication • Was the complication avoidable? – Yes, patient did not receive postoperative antibiotics • Would avoiding the complication change the outcome? – Yes, patient would avoid readmission and prolonged antibiotic course • What factors contributed to the complication? – Lack of postoperative antibiotic treatment in a patient at high risk for infectious complications (DM, CKD) • Questions?