Research
Original Investigation
Effect of a Clinical Practice Guideline for Pediatric
Complicated Appendicitis
Zachary I. Willis, MD; Eileen M. Duggan, MD, MPH; Brian T. Bucher, MD; John B. Pietsch, MD;
Monica Milovancev, MSN, CPNP; Whitney Wharton, MSN, CPNP; Jessica Gillon, PharmD, BCPS;
Harold N. Lovvorn III, MD; James A. O’Neill Jr, MD; M. Cecilia Di Pentima, MD, MPH; Martin L. Blakely, MD, MS
Invited Commentary
IMPORTANCE Complicated appendicitis is a common condition in children that causes
substantial morbidity. Significant variation in practice exists within and between centers. We
observed highly variable practices within our hospital and hypothesized that a clinical
practice guideline (CPG) would standardize care and be associated with improved patient
outcomes.
Supplemental content at
jamasurgery.com
OBJECTIVE To determine whether a CPG for complicated appendicitis could be associated
with improved clinical outcomes.
DESIGN, SETTING, AND PARTICIPANTS A comprehensive CPG was developed for all children
with complicated appendicitis at Monroe Carell Jr Children’s Hospital at Vanderbilt, a
freestanding children’s hospital in Nashville, Tennessee, and was implemented in July 2013.
All patients with complicated appendicitis who were treated with early appendectomy during
the study period were included in the study. Patients were divided into 2 cohorts, based on
whether they were treated before or after CPG implementation. Clinical characteristics and
outcomes were recorded for 30 months prior to and 16 months following CPG
implementation.
EXPOSURE Clinical practice guideline developed for all children with complicated appendicitis
at Monroe Carell Jr Children’s Hospital at Vanderbilt.
MAIN OUTCOMES AND MEASURES The primary outcome measure was the occurrence of any
adverse event such as readmission or surgical site infection. In addition, resource use,
practice variation, and CPG adherence were assessed.
RESULTS Of the 313 patients included in the study, 183 were boys (58.5%) and 234 were
white (74.8%). Complete CPG adherence occurred in 78.7% of cases (n = 96). The pre-CPG
group included 191 patients with a mean (SD) age of 8.8 (4.0) years, and the post-CPG group
included 122 patients with a mean (SD) age of 8.7 (4.1) years. Compared with the pre-CPG
group, patients in the post-CPG group were less likely to receive a peripherally inserted
central catheter (2.5%, n = 3 vs 30.4%, n = 58; P < .001) or require a postoperative computed
tomographic scan (13.1%, n = 16 vs 29.3%, n = 56; P = .001), and length of hospital stay was
significantly reduced (4.6 days post-CPG vs 5.1 days pre-CPG, P < .05). Patients in the
post-CPG group were less likely to have a surgical site infection (relative risk [RR], 0.41; 95%
CI, 0.27-0.74) or require a second operation (RR, 0.35; 95% CI, 0.12-1.00). In the pre-CPG
group, 30.9% of patients (n = 59) experienced any adverse event, while 22.1% of post-CPG
patients (n = 27) experienced any adverse event (RR, 0.72; 95% CI, 0.48-1.06).
CONCLUSIONS AND RELEVANCE Significant practice variation exists among surgeons in the
management of pediatric complicated appendicitis. In our institution, a CPG that
standardized practice patterns was associated with reduced resource use and improved
patient outcomes. Most surgeons had very high compliance with the CPG.
JAMA Surg. doi:10.1001/jamasurg.2016.0194
Published online March 30, 2016.
Author Affiliations: Department of
Pediatrics, Vanderbilt University
School of Medicine, Nashville,
Tennessee (Willis); Department of
Pediatric Surgery, Vanderbilt
University School of Medicine,
Nashville, Tennessee (Duggan,
Bucher, Pietsch, Milovancev,
Wharton, Lovvorn, O’Neill,
Di Pentima, Blakely); Division of
Pediatric Surgery, University of Utah,
Salt Lake City (Bucher); Monroe
Carell, Jr. Children’s Hospital at
Vanderbilt, Nashville, Tennessee
(Gillon).
Corresponding Author: Martin L.
Blakely, MD, MS, Monroe Carell Jr
Children's Hospital at Vanderbilt,
2200 Children's Way, Ste 7100,
Nashville, TN 37232 (martin.blakely
@vanderbilt.edu).
(Reprinted) E1
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a Vanderbilt University User on 04/01/2016
Research Original Investigation
A Clinical Guideline for Pediatric Complicated Appendicitis
A
ppendicitis is a common surgical condition, with a cumulative lifetime incidence of 9%.1 Children experience
the greatest risk of disease, and incidence among children is 4 times greater than the overall population. Appendicitis is often categorized as uncomplicated or complicated, with
the latter referring to a gangrenous or perforated appendix and
characterized by greater morbidity.2 Children, particularly those
younger than 15 years, are at very high risk of perforated appendicitis compared with young adults.1 The Healthcare Cost and
Utilization Project3 estimates that appendicitis with peritonitis accounted for 25 410 pediatric hospital admissions in 2012,
with a mean length of stay of 5.2 days and mean costs of $13 076.
Appendicitis is a common and costly condition,4 but the care
of children with appendicitis is highly variable.5 Complicated
appendicitis is associated with substantial postoperative morbidity. Nationwide, the readmission rate following appendectomy for complicated appendicitis is estimated at 12.8%.6 Clinical trials have consistently found a postoperative intra-abdominal
abscess rate of approximately 20% in cases of perforated appppendicitis.7,8 Other adverse events, such as superficial surgical
site infections (SSIs)and small-bowel obstruction, occur less frequently. These adverse events result in substantially increased
costs,6,9 additional exposure to ionizing radiation, additional operative interventions, prolonged antibiotic exposure, and delay
in return to premorbid function.
The appropriate management of children with complicated appendicitis has been the subject of substantial research, focusing on aspects including diagnosis, timing of surgery, surgical approach, preoperative and postoperative
antibiotic management, and discharge criteria. Still, many questions remain about optimal management in all phases.10-12 A
2004 survey of pediatric surgeons revealed considerable variation in the management of appendicitis.12
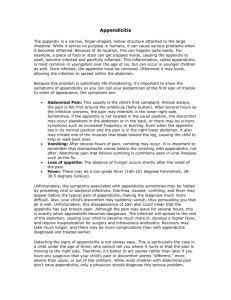
Medical conditions that are common, costly, and characterized by substantial variation in care are ideal targets for quality improvement via standardization of care. 4 Pediatric
appendicitis has been the subject of effective qualityimprovement initiatives that have reduced the use of computed tomographic (CT) scans for diagnosis13 and standardized the overall care of complicated appendicitis.14 In the
Monroe Carell Jr Children’s Hospital at Vanderbilt, we identified significant variability in the management of complicated
appendicitis along with high rates of intra-abdominal abscess formation and readmission. Therefore, we designed a
clinical practice guideline (CPG) with the goal of standardizing the operative and postoperative management of complicated appendicitis (Figure). The CPG was developed with multidisciplinary input from all services involved in these patients’
care as recommended by the Institute of Medicine.15 We hypothesized that CPG implementation would result in reduced health care use and fewer overall adverse events.
Methods
Question Can a clinical practice guideline for pediatric
complicated appendicitis achieve improvements in health care use
and patient outcomes?
Findings In this study comparing clinical outcomes before and
after implmentation of a clinical practice guideline for the
management of pediatric complicated appendicitis, there were
statistically significant declines in the incidence of postoperative
intra-abdominal abscess and the incidence of additional operative
procedures after guideline implementation. Resource use (eg,
hospital length of stay and peripherally inserted central catheter
use) also improved with clinical practice guideline–directed care.
Meaning The use of a clinical practice guideline for pediatric
complicated appendicitis can result in meaningful improvements
in patient outcomes.
nessee. Prior to guideline development, an internal review of
the management and outcomes of complicated appendicitis
revealed substantial practice variation and high rates of postoperative intra-abdominal abscess and readmission. Therefore, a CPG was proposed with the goals of standardizing practice and improving outcomes. The CPG was developed with
input from pediatric surgeons and pediatric surgery nurse practitioners, residents, and clinic nurses. The development team
also consulted with specialists from radiology; infectious
diseases; emergency medicine; and gastroenterology, hepatology, and nutrition. The final CPG was implemented on July
1, 2013.
The CPG applies to all patients with complicated appendicitis, defined as the operative finding of a gangrenous or perforated appendix. The CPG encourages early rather than interval appendectomy (Figure).16,17 For patients in whom an
abscess is discovered at operation, placement of a closedsuction drain is encouraged. All patients are administered piperacillin-tazobactam before and after the operation,18 with
transition to a 7-day course of oral ciprofloxacin and metronidazole when tolerating a diet. A white blood cell (WBC) count
is not checked to determine the duration of antibiotic therapy
or hospitalization. A follow-up clinic visit is scheduled within
2 weeks. For patients with ongoing fever, diarrhea, or intolerance of oral intake, along with physical examination findings
suspicious for intra-abdominal abscess, a CT scan is obtained
on the seventh postoperative day. If an abscess is discovered,
the patient may undergo operative or percutaneous drainage
or ongoing medical management as clinically indicated at the
discretion of the treating surgeon.
To allow individual surgeons to assess their performance, all pediatric surgeons received monthly reports detailing overall and individual CPG adherence. Small incentives in the form of gift cards were awarded to the monthly top
performer.
Patients and Data Collection
CPG Development
Monroe Carell Jr Children’s Hospital at Vanderbilt is a 271bed, freestanding, tertiary referral center in Nashville, TenE2
Key Points
From July 1, 2013, the date of CPG implementation, until November 1, 2014, all patients treated for complicated appendicitis in Monroe Carell Jr Children’s Hospital at Vanderbilt were
JAMA Surgery Published online March 30, 2016 (Reprinted)
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a Vanderbilt University User on 04/01/2016
jamasurgery.com
A Clinical Guideline for Pediatric Complicated Appendicitis
Original Investigation Research
Figure. Clinical Practice Guideline (CPG) Used for Suspected and Confirmed Complicated Appendicitis
Patient characteristics
increasing likelihood of
gangrenous or perforated
appendicitis: young age,
>48 h of symptoms,
generalized tenderness on
abdominal examination,
white blood cell count
>19 400 μL, and abscess
identification by imaging
Not improving/responding
Continued fever, examination
not improving, diarrhea, or
otherwise worsening condition,
consider nutrition consult
No
Order
piperacillin-tazobactam.
If penicillin allergy:
ciprofloxacin/flagyl
Early laparoscopic appendectomy
• Local irrigation (500-1000 mL)
• Blake drain if abscess or
widespread contamination
Consider computed tomography of
abdomen/pelvis POD7 if concern for
intra-abdominal abscess
Responding
to treatment?
Interventional
radiology
request consult
Yes
Inclusion criteria
Children with gangrenous or perforated appendicitis
determined intraoperatively by the attending surgeon.
In children with very delayed presentation (>1 wk)
who are nontoxic and have a contained abscess
on imaging, consideration should be given to treatment
with interval appendectomy (with/without initial
drainage of the intra-abdominal abscess) rather than
using this CPG.
Yes
Intraabdominal
abscess?
No
Evaluate for
other infection
source
Interventional radiology
or operative drainage of
intra-abdominal abscess;
obtain culture
Consider oral
ciprofloxacin/flagyl
when taking regular diet
Meets discharge criteria
Discharge criteria
Afebrile (<38°C) >24 h
Tolerating diet
Adequate pain control with oral medications
Benign abdominal examination by attending surgeon
Ambulating without assistance
Discharge home with
ciprofloxacin/flagyl 7 d
Follow-up 1 wk,
if unable to follow up,
telephone call
POD7 indicates postoperative day 7. To convert white blood cell count to ×109/L, multiply by 0.001.
prospectively added to a study-specific REDCap database.19
To determine baseline patient outcomes, resource use, and
practice variation, a cohort of patients treated for complicated appendicitis in the 30 months prior to CPG implementation (January 1, 2011, to June 30, 3013) was created. All
records in that time with an International Classification of
Diseases, Ninth Edition diagnosis code of 540.0 (acute
appendicitis with generalized peritonitis) or 540.1 (acute
appendicitis with peritoneal abscess) were ascertained.
Cases were excluded at this stage if there was no mention of
appendiceal perforation or gangrenous appendicitis in the
operative report or surgeon’s progress notes. For both the
pre- and post-CPG patients, medical records were reviewed,
and demographic and clinical data were extracted into
the database. Only patients who were treated by early
appendectomy (occurring during the index admission for
appendicitis) were included in this analysis. Because of the
subjective nature of the diagnosis of gangrenous appendicitis, these patients were also excluded from the primary
analysis (n = 34), leaving only patients with a grossly perforated appendix or gross peritoneal contamination. Because
the CPG did apply to patients with gangrenous appendicitis,
a secondary analysis was conducted that included these
patients. The study was approved by the institutional
review board of the Vanderbilt University School of Medijamasurgery.com
cine. The institutional review board determined it to be a
quality improvement project with no consent required.
Outcome Measures
The primary outcome measure was the occurrence of any adverse event within 30 days of appendectomy. Adverse events
assessed included SSIs, classified as superficial incisional, deep
incisional, or organ/space infection20; emergency department
visits; hospital readmissions; additional operative procedure;
any interventional radiology procedure; and adverse effects of
antibiotics requiring discontinuation and/or medical treatment.
Health care use measures included length of stay, proportion of
patients undergoing interval appendectomy, proportion undergoing open appendectomy, proportion receiving a postoperative CT scan, proportion receiving a peripherally inserted central catheter (PICC), proportion having a WBC count checked to
determine duration of antibiotic administration, and proportion
receiving parenteral nutrition. The CPG strongly discouraged use
of PICC unless indicated for parenteral nutrition. Initial diagnostic evaluation was not addressed by the CPG, but the proportion
of patients receiving a preoperative CT scan was gathered to assess baseline trends in CT use.
To assess CPG adherence, we calculated the adherence rate
for each individual surgeon and tabulated the most common
reasons for nonadherence. To be considered CPG-adherent, an
(Reprinted) JAMA Surgery Published online March 30, 2016
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a Vanderbilt University User on 04/01/2016
E3
Research Original Investigation
A Clinical Guideline for Pediatric Complicated Appendicitis
Table 1. Demographic Characteristics, Clinical Data at the Time of Presentation, Imaging Use and Findings,
and Operative Findingsa
Pre-CPG
(n = 191)
Characteristic
Age, mean (SD), y
Male, No. (%)
Post-CPG
(n = 122)
P Value
8.8 (4.0)
8.7 (4.1)
.79
111 (58.1)
72 (59.0)
.88
Race, No. (%)
American Indian or Alaska Native
1 (0.5)
1 (0.8)
Asian
3 (1.6)
4 (3.3)
Black or African American
23 (12.0)
8 (6.6)
141 (73.8)
93 (76.2)
23 (12.0)
16 (13.1)
44 (23.0)
28 (23.0)
.99
Duration of symptoms, h
76.6 (65.1)
67.6 (47.8)
.16
White blood cell count, /μL
17.2 (6.4)
17.8 (6.0)
.41
White
Unknown/not reported
.43
Ethnicity, No. (%)
Hispanic
Presenting characteristics, mean (SD)
No. of patients
183
117
Preoperative imaging, No. (%)
CT
128 (67.0)
63 (48.4)
.001
Ultrasonography
79 (41.4)
79 (64.8)
<.001
None
10 (5.2)
1 (0.8)
.04
11.3 (7.2)
.26
Operative management, mean (SD), h
Time from presentation to OR
10.2 (10.1)
No. of patients
190
119
167 (87.4)
105 (86.1)
Open
11 (5.8)
8 (6.6)
Laparoscopic converted to open, No. (%)
13 (6.8)
9 (7.4)
.92
79 (41.4)
53 (43.4)
.72
Laparoscopic, No. (%)
Abscess identified at operation
individual patient had to meet the following criteria: (1) received only appropriate inpatient antibiotics (piperacillintazobactam or ciprofloxacin plus metronidazole if allergic to
penicillin); (2) did not have a WBC count checked to determine duration of antibiotics or readiness for discharge; (3) prescribed ciprofloxacin plus metronidazole for 7 days at discharge; and (4) attended a follow-up surgery clinic appointment
within 30 days of discharge. Responsibility for nonadherence
was assigned to the medical team or family. For example, if no
follow-up appointment was scheduled, then responsibility for
nonadherence was assigned to the surgical team. If a patient
failed to attend a scheduled follow-up appointment, responsibility was assigned to the family. To determine the effect of
the CPG on practice variation, between-surgeon use of PICCs,
parenteral nutrition, and WBC count to determine discharge
eligibility was tabulated.
Data Analysis
Dichotomous measures were assessed with χ2 test and Fisher
exact test as appropriate. For dichotomous outcome measures, relative risk (RR) with 95% CI was calculated with the
pre-CPG group as the referent. For continuous measures and
outcomes, a t test was used when data were normally distributed. When data were not normally distributed, the Wilcoxon rank sum test was used. All tests were 2-tailed, with a P
value less than .05 considered statistically significant. Analyses were conducted using Stata/IC 13.1 (StataCorp).
E4
Abbreviations: CPG, clinical practice
guideline; CT, computed tomography;
OR, operating room.
SI conversion factor: to convert white
blood cell count to × 109 per liter,
multiply by .001.
a
Excluding patients diagnosed as
having appendicitis more than
48 hours after admission (n = 4).
Results
Demographic and Clinical Presenting Characteristics
Of 219 patients assessed for inclusion in the pre-CPG cohort,
19 were excluded because of interval appendectomy and 9 were
excluded for nonperforated appendicitis, for a final pre-CPG
cohort of 191 patients. One hundred fifty-two patients were assessed for inclusion in the post-CPG cohort, after excluding 5
because of interval appendectomy and 25 because of nonperforated appendicitis, for a final post-CPG group of 122
patients.
Data regarding patients’ demographic and clinical characteristics are presented in Table 1. There were no significant
differences in the age (P = .79), sex (P = .88), race (P = .43), or
Hispanic ethnicity (P = .99) between patients in the pre-CPG
and post-CPG groups. There were no significant differences in
preoperative duration of symptoms (P = .16) or WBC count
(P = .41) on admission. There was no difference in the proportion of patients diagnosed as having an intra-abdominal abscess at the time of appendectomy (P = .72).
Preoperative Imaging and Operative Management
Preoperative and operative management are summarized in
Table 1. There was no difference in operative approach between the 2 cohorts, with most patients in both groups undergoing laparoscopic appendectomy (P = .94). There was a sig-
JAMA Surgery Published online March 30, 2016 (Reprinted)
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a Vanderbilt University User on 04/01/2016
jamasurgery.com
A Clinical Guideline for Pediatric Complicated Appendicitis
Original Investigation Research
nificant difference in the use of preoperative imaging, with
67% of pre-CPG patients undergoing a CT scan vs 48% of postCPG patients (P = .001). Conversely, 41.4% of pre-CPG
patients had preoperative ultrasonography vs 64.8% of postCPG patients (P < .001).
A total of 10 individual surgeons operated in cases of
complicated appendicitis during the study. Three surgeons performed a total of 40 appendectomies for complicated appendicitis exclusively in the pre-CPG period, while 1 surgeon
performed 1 appendectomy for complicated appendicitis exclusively in the post-CPG period. The remaining 6 surgeons performed a minimum of 9 appendectomies for complicated
appendicitis in both the pre- and post-CPG periods.
CPG Adherence and Standardization of Practice
Of the 122 patients in the post-CPG group, complete CPG adherence occurred in 96 patients (78.7%). Twenty-nine deviations from protocol occurred in 26 patients, with the most common reason being failure to follow up in pediatric surgery clinic
(n = 12) and failure to prescribe 7 days of ciprofloxacin and metronidazole (n = 10). Thirteen of 29 deviations (45%) were attributed to the health care team; the remainder were attributed to the family, most commonly for failure to attend the
scheduled follow-up appointment. When considering only adherence failures attributed to health care teams, overall adherence was 87.5%. For the 6 surgeons treating patients after
CPG implementation, adherence ranged from 67% to 100%
(Table 2). There were no temporal trends in adherence during
the 16 months of observation.
Substantial variation in practice was observed before CPG
implementation. Prior to CPG implementation, individual sur-
Table 2. Clinical Practice Guidelines Adherence by Operating Surgeon
Surgeon
19
18 (94.7)
2
18
12 (66.7)
3
17
13 (76.5)
4
23
22 (95.7)
5
22
21 (95.5)
6
1
1 (100)
7
9
9 (100)
109
96 (88.1)
Total
a
Adherence, No. (%)a
No. of Cases
1
Cases in which the family was nonadherent are excluded (n = 13).
geons’ use of PICCs ranged from 7% to 48%; after CPG implementation, no operating surgeon ordered placement of more
than 1 PICCs (range, 0%-5%). Parenteral nutrition use ranged
from 6% to 22% before implementation and from 0% to 5%
after implementation. Before the CPG, individual surgeons’ use
of the WBC count to determine eligibility for discharge ranged
from 7% to 100%; following implementation, the range was
0% to 11%. The intersurgeon distribution of surgical approach was similar between the cohorts: the use of an open
approach ranged from 0% to 17% for both cohorts.
Postoperative Resource Use
Inpatient use of hospital services and procedures was lower
in the post-CPG group (Table 3). Specifically, in the pre-CPG
group, 84 patients (44%) had a WBC count drawn prior to discharge compared with 5 (4.1%, P < .001) in the post-CPG group.
Fifty-eight patients (30.4%) in the pre-CPG group and 3 patients (2.5%) in the post-CPG group (P < .001) underwent PICC
placement. Twenty-three patients (12.0%) in the pre-CPG group
underwent an interventional radiology procedure compared
with 3 (2.5%) in the post-CPG group (P = .003). Parenteral nutrition was administered to 22 patients (11.5%) in the pre-CPG
group and to 2 patients (1.6%) in the post-CPG group (P = .001).
In the pre-CPG group, 56 patients (29.3%) underwent a postoperative CT scan, compared with 16 (13.1%) in the post-CPG
group (P = .001).
Patient Outcomes
The proportions of patients experiencing adverse events between the 2 groups are presented in Table 4. In the pre-CPG
group, 59 patients (30.9%) experienced any adverse event,
while 27 post-CPG patients (22.1%) experienced any adverse
event (RR, 0.72; 95% CI, 0.48-1.06). In the pre-CPG group, 27
patients (14.1%) returned to the emergency department within
30 days of appendectomy, while 14 post-CPG patients (11.5%)
returned to the emergency department (RR, 0.81; 95% CI, 0.441.49). The 30-day readmission rate was 16.2% in the pre-CPG
group and 11.5% in the post-CPG group (RR, 0.71; 95% CI, 0.391.27). Prior to CPG implementation, 9.4% of patients returned
to the operating room, while 3.3% of post-CPG patients required
a second surgical procedure (RR, 0.35; 95% CI, 0.12-1.00). There
was a significant decrease in the proportion of patients who had
an organ-space SSI, from 24.1% in the pre-CPG group to 9.8%
in the post-CPG group (RR, 0.41; 95% CI, 0.23-0.74). Superficial incisional and deep incisional SSIs were uncommon and no
Table 3. Resource Use by CPG Status
No. (%)
Resource
Pre-CPG
(n = 191)
Post-CPG
(n = 122)
WBC count prior to discharge
84 (44)
5 (4.1)
0.09 (0.05-0.17)
<.001
PICC at any time
58 (30.4)
3 (2.5)
0.08 (0.04-0.18)
<.001
Any IR procedure
23 (12.0)
3 (2.5)
0.20 (0.07-0.58)
.003
Receipt of parenteral nutrition
22 (11.5)
2 (1.6)
0.14 (0.04-0.47)
.001
56 (29.3)
16 (13.1)
0.45 (0.28-0.72)
.001
8 (4.2)
1 (0.8)
0.20 (0.02-1.54)
.10
P Value
RR (95% CI)
Postoperative
CT
Ultrasonography
jamasurgery.com
Abbreviations: CPG, clinical practice
guideline; CT, computed tomography;
IR, interventional radiology;
PICC, peripherally inserted central
catheter; RR, relative risk;
WBC, white blood cell.
(Reprinted) JAMA Surgery Published online March 30, 2016
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a Vanderbilt University User on 04/01/2016
E5
Research Original Investigation
A Clinical Guideline for Pediatric Complicated Appendicitis
Table 4. Patient Outcomes
No. (%)
Outcome
Postoperative length of stay, median, d
Pre-CPG
(n = 191)
5.1
Post-CPG
(n = 122)
4.6
RR (95% CI)
NA
P Value
.03
Any adverse event
59 (30.9)
27 (22.1)
0.72 (0.48-1.06)
.09
ED visit
27 (14.1)
14 (11.5)
0.81 (0.44-1.49)
.50
Readmission
31 (16.2)
14 (11.5)
0.71 (0.39-1.27)
.24
Return to OR
18 (9.4)
4 (3.3)
0.35 (0.12-1.00)
.04
46 (24.1)
12 (9.8)
0.41 (0.23-0.74)
4 (2.1)
2 (1.6)
0.78 (0.15-4.21)
SSI
Organ-space (intra-abdominal abscess)
Incisional (superficial or deep)
different between the groups. Postoperative length of stay was
significantly shorter in the post-CPG cohort (median of 5.1 days
vs 4.6 days, P < .05). For patients with an intra-abdominal abscess at the time of appendectomy, the median postoperative
length of stay was 5.8 days in the pre-CPG cohort vs 4.9 days
in the post-CPG cohort (P < .05).
Results of a secondary analysis of patient outcomes, in
which patients with gangrenous appendicitis were included,
are displayed in the eTable in the Supplement. There were 9
such patients in the pre-CPG group and 25 such patients in the
post-CPG group (4.5% vs 17.0%, P < .001). Adverse events occurred in 2 of these patients, both in the post-CPG group.
Discussion
Implementation of a CPG for complicated appendicitis in our
institution was associated with greater standardization of
care; decreased postoperative use of CT scans, interventional
radiology procedures, and PICCs; shorter inpatient length of
stay; and lower rates of postoperative infectious complications. The high adherence rate suggests that the CPG was acceptable to pediatric surgeons, pediatric surgery nurse practitioners, residents, and clinic nurses, likely owing to the
collaborative process by which the guideline was developed.
Among the 122 patients treated after CPG implementation, there
were only 13 deviations attributed to the pediatric surgery service (10.7%).
We observed a 14.3% reduction in the absolute risk of an
organ-space SSI, translating to a number needed to treat of 7
patients to avoid one such complication. This improvement
is reflected in the observed reductions in the length of stay and
the risks of requiring an interventional radiology procedure or
a second operative procedure.
Since 2010, several research groups have reported successful efforts to reduce CT scan use in the diagnosis of pediatric appendicitis.13,21,22 In our study, the use of preoperative
CT scans was significantly lower in the post-CPG group because diagnosis relied increasingly on ultrasonography. Because diagnostic approach was not a target of the CPG, this
change is likely associated with a secular trend. More strikingly, patients treated after CPG implementation were 55% less
likely to undergo a postoperative CT scan than their predecessors, a reduction of 22 CT scans per 100 patients treated. PostE6
.002
>.99
Abbreviations: CPG, clinical practice
guideline; ED, emergency
department; NA, not applicable;
OR, operating room; RR, relative risk;
SSI, surgical site infection.
operative CT scans were not replaced by ultrasonographies as
in preoperative patients because the use of postoperative
ultrasonographies did not rise. Because the CPG specified triggers for a postoperative CT scan, the decline in CT use is
believed to be caused by improvements in patient outcomes.
Furthermore, the decrease in CT use was not accompanied by
an increase in length of stay or readmissions, suggesting that
this approach did not result in missed diagnoses of postoperative SSIs.
Similar benefit was seen with the reduction in PICC placements. Rice-Townsend et al5 found that PICC use by hospital
ranged from 1.7% to 81.8% for patients with complicated appendicitis, with a weighted average of 18.9%. Use of PICCs fell
from 30.4% to 2.5% in our cohort, a 92% reduction. While there
were no major complications related to PICCs in either group,
a 2012 study23 found that 31% of children who have a PICC
placed experience a medically attended complication. The CPG
recommends against PICC use except in unusually complicated cases such as when parenteral nutrition was required.
In the pre-CPG cohort, PICCs were placed frequently and with
highly variable frequency among attending surgeons. Following CPG implementation, PICCs were rarely placed. Similarly,
there was a broad range of practice prior to CPG implementation with regard to obtaining a WBC count to determine
duration of antibiotic therapy and/or eligibility for discharge.
In the post-CPG cohort, the WBC count was rarely checked by
any of the attending surgeons.
Our study had several limitations. There was a significantly greater proportion of patients with gangrenous appendicitis in the post-CPG era than the pre-CPG era. The reason
for this is unclear. Gangrenous appendicitis is a subjective diagnosis, and surgeons’ propensity to assign this diagnosis may
have been affected by the presence of the CPG. The diagnosis
of perforated appendicitis required gross perforation and/or
gross contamination of the peritoneal cavity with bowel contents; this diagnosis is far less subjective. To eliminate this difference in patient groups before and after the CPG implementation, gangrenous appendicitis cases were excluded from the
primary analysis. Consequently, the patient cohorts prior to
and after CPG implementation were very similar (ie, all had perforated appendicitis and were similar in other regards). There
was little difference between our primary results and the results of a secondary analysis in which patients with gangrenous appendicitis were included. Any assessment of a guide-
JAMA Surgery Published online March 30, 2016 (Reprinted)
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a Vanderbilt University User on 04/01/2016
jamasurgery.com
A Clinical Guideline for Pediatric Complicated Appendicitis
line implementation is biased by time: we do not know how
management and outcomes might have changed over time
without intervention. Establishing a contemporaneous control group with such a study design was not feasible because
all clinicians were necessarily aware of the CPG. Additionally,
the failure to find a statistically significant difference on several important outcome measures was likely a consequence of
inadequate power. Finally, because several interventions were
incorporated simultaneously, it is difficult to determine which
changes had the greatest benefit.
Despite these limitations, our results suggest that a concerted effort to standardize the care of children with complicated appendicitis may substantially improve patient outcomes. Our guideline was designed to not replace the surgeon’s
judgment with respect to any individual case. For a heteroge-
ARTICLE INFORMATION
Accepted for Publication: January 19, 2016.
Published Online: March 30, 2016.
doi:10.1001/jamasurg.2016.0194.
Author Contributions: Drs Willis and Blakely had
full access to all the data in the study and take
responsibility for the integrity of the data and the
accuracy of the data analysis.
Study concept and design: Duggan, Pietsch,
Milovancev, Wharton, O’Neill, Di Pentima, Blakely.
Acquisition, analysis, or interpretation of data:
Willis, Duggan, Bucher, Pietsch, Milovancev, Gillon,
Lovvorn, Di Pentima, Blakely.
Drafting of the manuscript: Willis, Milovancev,
Blakely.
Critical revision of the manuscript for important
intellectual content: Duggan, Bulcher, Pietsch,
Wharton, Gillon, Lovvorn, O’Neill, Di Pentima,
Blakely.
Statistical analysis: Willis, Duggan, Di Pentima.
Administrative, technical, or material support:
Bucher, Milovancev, Wharton, Gillon, Lovvorn,
Di Pentima.
Study supervision: Pietsch, O’Neill, Di Pentima,
Blakely.
Conflict of Interest Disclosures: None reported.
Funding/Support: Dr Willis was supported by
training grant T32 AI095202 from the National
Institutes of Health (principal investigator: Mark
Denison, MD).
Role of the Funder/Sponsor: The funding
organization had no role in the design and conduct
of the study; collection, management, analysis, and
interpretation of the data; preparation, review, or
approval of the manuscript; and decision to submit
the manuscript for publication.
REFERENCES
1. Anderson JE, Bickler SW, Chang DC, Talamini MA.
Examining a common disease with unknown
etiology: trends in epidemiology and surgical
management of appendicitis in California,
1995-2009. World J Surg. 2012;36(12):2787-2794.
2. Dunn J. Appendicitis. In: Coran A, ed. Pediatric
Surgery. Philadelphia, PA: Saunders; 2012:1255-1263.
3. Agency for Health Care Research and Quality.
HCUP Kids’ Inpatient Database. http://hcupnet
.ahrq.gov/. Published 2012. Accessed November
26, 2014.
jamasurgery.com
Original Investigation Research
neous condition with many open questions about optimal management, flexibility within a guideline is likely to increase its
acceptability.
Conclusions
Complicated appendicitis is an important target for quality improvement. In the absence of national management guidelines, individual institutions may develop their own guidelines based on the best available evidence, taking into account
their particular surgeons’ experience, case mix, trainee involvement, and imaging capability. A careful assessment for
local practice variation and undesirable outcomes will identify points of emphasis for institutional guidelines.
4. Keren R, Luan X, Localio R, et al; Pediatric
Research in Inpatient Settings (PRIS) Network.
Prioritization of comparative effectiveness research
topics in hospital pediatrics. Arch Pediatr Adolesc
Med. 2012;166(12):1155-1164.
5. Rice-Townsend S, Barnes JN, Hall M, Baxter JL,
Rangel SJ. Variation in practice and resource
utilization associated with the diagnosis and
management of appendicitis at freestanding
children’s hospitals: implications for value-based
comparative analysis. Ann Surg. 2014;259(6):12281234.
evaluation can decrease computed tomography
utilization while maintaining diagnostic accuracy.
Pediatr Emerg Care. 2013;29(5):568-573.
14. Slusher J, Bates CA, Johnson C, Williams C,
Dasgupta R, von Allmen D. Standardization and
improvement of care for pediatric patients with
perforated appendicitis. J Pediatr Surg. 2014;49(6):
1020-1024.
15. Institute of Medicine. Clinical practice
guidelines we can trust. http://www.nap.edu/read
/13058/chapter/2#4. Accessed February 5, 2015.
6. Rice-Townsend S, Hall M, Barnes JN, Baxter JK,
Rangel SJ. Hospital readmission after management
of appendicitis at freestanding children’s hospitals:
contemporary trends and financial implications.
J Pediatr Surg. 2012;47(6):1170-1176.
16. St Peter SD, Aguayo P, Fraser JD, et al. Initial
laparoscopic appendectomy versus initial
nonoperative management and interval
appendectomy for perforated appendicitis with
abscess: a prospective, randomized trial. J Pediatr
Surg. 2010;45(1):236-240.
7. Fraser JD, Aguayo P, Leys CM, et al. A complete
course of intravenous antibiotics vs a combination
of intravenous and oral antibiotics for perforated
appendicitis in children: a prospective, randomized
trial. J Pediatr Surg. 2010;45(6):1198-1202.
17. Blakely ML, Williams R, Dassinger MS, et al.
Early vs interval appendectomy for children with
perforated appendicitis. Arch Surg. 2011;146(6):
660-665.
8. St Peter SD, Tsao K, Spilde TL, et al. Single daily
dosing ceftriaxone and metronidazole vs standard
triple antibiotic regimen for perforated appendicitis
in children: a prospective randomized trial. J Pediatr
Surg. 2008;43(6):981-985.
18. Goldin AB, Sawin RS, Garrison MM, Zerr DM,
Christakis DA. Aminoglycoside-based
triple-antibiotic therapy versus monotherapy for
children with ruptured appendicitis. Pediatrics.
2007;119(5):905-911.
9. Myers AL, Williams RF, Giles K, et al. Hospital
cost analysis of a prospective, randomized trial of
early vs interval appendectomy for perforated
appendicitis in children. J Am Coll Surg. 2012;214
(4):427-434.
19. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez
N, Conde JG. Research electronic data capture
(REDCap)–a metadata-driven methodology and
workflow process for providing translational
research informatics support. J Biomed Inform.
2009;42(2):377-381.
10. Lee SL, Islam S, Cassidy LD, Abdullah F, Arca
MJ; 2010 American Pediatric Surgical Association
Outcomes and Clinical Trials Committee. Antibiotics
and appendicitis in the pediatric population: an
American Pediatric Surgical Association Outcomes
and Clinical Trials Committee systematic review.
J Pediatr Surg. 2010;45(11):2181-2185.
11. Nadler EP, Gaines BA; Therapeutic Agents
Committee of the Surgical Infection Society. The
Surgical Infection Society guidelines on
antimicrobial therapy for children with appendicitis.
Surg Infect (Larchmt). 2008;9(1):75-83.
12. Muehlstedt SG, Pham TQ, Schmeling DJ. The
management of pediatric appendicitis: a survey of
North American pediatric surgeons. J Pediatr Surg.
2004;39(6):875-879.
13. Russell WS, Schuh AM, Hill JG, et al. Clinical
practice guidelines for pediatric appendicitis
20. Saito JM, Chen LE, Hall BL, et al. Risk-adjusted
hospital outcomes for children’s surgery. Pediatrics.
2013;132(3):e677-e688.
21. Le J, Kurian J, Cohen HW, Weinberg G,
Scheinfeld MH. Do clinical outcomes suffer during
transition to an ultrasound-first paradigm for the
evaluation of acute appendicitis in children? AJR Am
J Roentgenol. 2013;201(6):1348-1352.
22. Toorenvliet BR, Wiersma F, Bakker RFR, Merkus
JWS, Breslau PJ, Hamming JF. Routine ultrasound
and limited computed tomography for the
diagnosis of acute appendicitis. World J Surg. 2010;
34(10):2278-2285.
23. Barrier A, Williams DJ, Connelly M, Creech CB.
Frequency of peripherally inserted central catheter
complications in children. Pediatr Infect Dis J.
2012;31(5):519-521.
(Reprinted) JAMA Surgery Published online March 30, 2016
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://archsurg.jamanetwork.com/ by a Vanderbilt University User on 04/01/2016
E7