Eckert - Glenwood Autism and Behavioral Health Center
advertisement

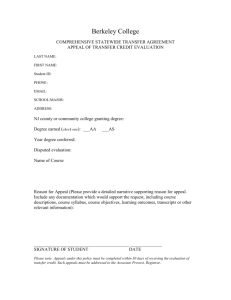
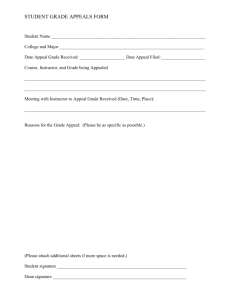
Autism Speaks Presentation October 21, 2011 Today’s Presentation MedClaims Liaison Overview • Our mission • What we do • Who we are • How we work Helping Families Access Insurance Reimbursement for Autism-Related Therapies • Common Insurance Pitfalls • Know the Codes • Questions to Ask the Insurance Company • Understand the Limitations of the Insurance Policy • Authorization, Adjudication, Appeal MedClaims Liaison Overview Our Mission “It all started with a friend in need…. “ MedClaims Liaison was launched in 2009. Our goal is to deliver relief, reassurance, and reimbursements to our customers through comprehensive management of their health insurance claims. Relief: • A complete, end-to-end solution for the work of interpreting, organizing, submitting, auditing, and pursuing claims. • Single resource for the management of all claims. Reassurance: • Confidence that an expert is handling your claims. • Confidence that your out-of-pocket costs are being properly accounted for. • Confidence that you’re getting all you deserve from your coverage. Reimbursement: • Full and timely compensation from carriers. Who We Are We are a team of passionate specialists who advocate on behalf of its Members to maximize healthcare benefits and minimize stress. Our claims specialists bring a range of skills to bear when managing claims on behalf of our customers Professional Backgrounds Skill Sets • Claims processing units of major health insurance carriers • Claims processing • Third party claims processors • Benefits administration • Third party administrators • HIPAA • Medical offices • Customer service! • Medical billing What We Do We provide a single resource for the management of the full lifecycle of our customers’ claims • Document organization • Advising customers re. balances due • Submission of new claims • Reviewing bills for accuracy • Auditing and pursuing existing claims • Negotiating with providers to reduce balances • Coordination of secondary/supplemental policies • Coordination of HSAs and FSAs • Filing and pursuing appeals • Annual statements summarizing insurance utilization • Understanding plan options upon renewals • Phone and online support How We Work (continued) Get started in 10 minutes. We start working immediately. We contact your healthcare providers and insurance carriers, obtain your historical bills and claims, and ensure you’ve been properly billed and reimbursed. You get all the money back that you are entitled to! Helping Families Access Insurance Reimbursement for Autism-Related Therapies Common Insurance Pitfalls • “Unclean Claims” get sucked into the insurance black-hole. Make sure the claim being submitted has all of the necessary elements to be processed before being submitted. 1. Service provider’s name, credentials, license # 2. Service provider address and phone number 3. Provider Tax ID and/or NPI 4. Itemized dates of service 5. Fees for services 6. CPT codes with corresponding units 7. Diagnosis codes 8. Patient Name 9. Bill/Receipt total 10. Indication of payment in full (if applicable) Common Insurance Pitfalls (continued) I have the benefits! I have a “Clean” claim to submit! I mailed my claims to the correct address! What do you mean my claims aren’t on file and they aren’t anywhere in the system?? Common Insurance Pitfalls (continued) Do’s and Don’ts of Insurance Customer Service: DO: Ask the customer service agent to document everything that was discussed during your phone call DO: Ask for the customer service agent’s name and reference # for the phone call – document the date of the call DON’T: Be afraid to ask difficult questions about the coverage of your plan DO: Trust your instincts – if you feel like the customer service agent was giving you wrong information, call back and ask to verify the information DON’T: Assume anything about your plan or benefits DON’T: Send documents via certified mail to a PO Box! DO: Follow up periodically to ensure that your claims are received and getting processed DON’T: Stop because you’re frustrated! Allowing too much time to pass can hinder your ability to get the money you’re entitled to! Know the Codes In order to ensure that the insurance company is reimbursing the maximum amount of health care costs, according to the benefits of the policy, you have to KNOW THE CODE. • Make sure that the CPT/HCPC code on the claim matches it’s description and has been billed with the appropriate unit/time ratio. • Make sure that the CPT/HCPC code accurately reflect the services that are being rendered. • Make sure that you find out which benefit the code is going to use under the benefits on the policy. Questions to Ask the Insurance Company • Is this a Fully-funded Insurance policy or a Self-funded policy? (Also know as fully-insurance or self-insured • If Self-funded, then state mandated coverage has to be specifically stated as applicable. • If Fully-funded, state mandates are eligible • Is this a Small Group or Individual Policy? • If the plan is either small group or an individual policy, state mandated benefits do not apply unless specified • Do state and/or federal mandates apply to this policy? (if the Rep sounds clueless, tell them to check the contract exceptions or certificate of coverage) • Are there exclusions for the coverage of Autism related treatments? • If yes, then claims with an ASD diagnosis will likely deny (299.XX) • If no, then claims will only receive ASD benefits with an ASD dx Understand the Limitations of the Policy • Check visit limits for Speech, Occupational, Physical, Behavioral Therapies Are these visit limits separate or combined? Are these visit limits separate or combined between the In-Network and Out-of-Network benefits? • Ask if authorization is required prior to services being performed. If so, is this something that can be performed by the parent or does it need to come from the provider’s office? • Check to see if there are Penalties for failure to obtain authorization prior to services If so, what are they? • Ask what are the Timely Filing Limitations of the policy What is timely filing for a Participating Provider claim? What is timely filing for a Non-Participating Provider claim? Ask if there are there any dollar limitations for a specific benefit? Authorization, Adjudication, Appeals Authorizations • Pre-Certification – Obtained PRIOR to services. Strive for this every time. It will expedite claims and alleviate requests for medical records. If the insurance company states that pre-certification is not required but that they can request medical records once a claim is submitted, request that a precertification can be performed. You will need to know the codes that are going to be billed. If the insurance company authorizes for a 96152 but the provider bills a 98960, the claim will deny and this is an appropriate denial. • Retro-Authorization – Performed after services have been rendered This type of authorization is typically done after services have been performed. The insurance company will request the provider’s medical records. Follow instructions closely so that potential for errors are minimized. Authorization, Adjudication, Appeals (continued) Adjudication There are a variety of ways an insurance company receives and processes claims. Understanding HOW a claim is processed gives insight when a claim is mis-processed. • Auto-Adjudication – Some claims submitted on standardized billing forms are electronically scanned for Data, entered, and then processed without a human ever touching the claim. Claims that are submitted electronically through a provider billing service are also often autoadjudicated. • Vendor Processing – Often times, some insurance companies will receive claims and then outsource their claim processing to a vendor or workshop. Actual claims representatives will process the claim . • Manual Processing – Claims are entered by claim and benefit analysts who manually enter the claim and benefit data. Authorization, Adjudication, Appeals (continued) Appeals Tips When it comes to filing an appeal, insurance companies will all have their own internal process. When a claim is denied , and there is recourse to Appeal, the instructions outlined on the Explanation of Benefits have to be followed CLOSELY. There are typically stringent time frames for a customer to respond. Do not send an Appeal via FedEx or Certified Mail unless a physical address is available Make sure that to include appropriate documentation and supportive evidence to “make a case” to the insurance company Do not give up because the insurance company has upheld the denial. Typically there are 2 or 3 levels of appeal that can be filed. If an insurance company continues to uphold a denial and all internal Appeal options have been exhausted, the next step is to contact your state Department of Insurance . They can provide direction on what the next steps are for filing a Grievance, a 3rd Party Review or other options available. Our Commitment to This Community Contact Information Jacqueline Eckert Director, Reimbursement Solutions jeckert@medclaimsliaison.com (484)493-7771 or 1(855) MCL-4YOU www.medclaimsliaison.com