The Tissue Level of Organization

The Tissue Level of Organization
Chapter 4
1.
2.
3.
4.
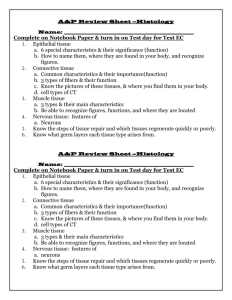
Four Basic Tissue Types
Epithelial
Connective
Muscle neural
Epithelial Tissue
Includes epithelia and glands
Epithelia – layers of cells that cover internal or external surfaces
Glands – secreting cells derived from epithelia
Important characteristics:
Cells bound closely together
A free (apical) surface exposed to the environment or to some internal chamber or passageway
Attachment to underlying connective tissue
By a basement membrane
Epithelial cells that are damaged or lost at the exposed surface are continuously replaced
Functions of Epithelia
1.
Provide physical protection
Protect exposed and internal surfaces
2.
3.
Control permeability
Provide sensation detect changes in the environment and relay the information to the nervous system
4.
Produce specialized secretions
Gland cells
Glandular epithelium
Exocrine – secretions discharged onto the surface of the epithelium
Endocrine – secretions into the surrounding tissues and blood (hormones)
Intercellular Connections
Must remain firmly attached to a basement membrane and each other
Tight junction
Lipid layers of adjacent cell membranes are tightly bound together by interlocking membrane proteins
Gap junction
Two cells are held together by embedded membrane proteins.
Form a narrow passageway to let small molecules and ions to pass through
Desmosome
Cell membranes of two cells are locked together by intercellular cement and by membrane proteins connected to a network of intermediate filaments
The Epithelial Surface
Have specialized structures that distinguish them from other body cells
Many that line internal passageways have microvilli on their exposed surface
Increases surface area about 20 times
A cell with a ciliated surface has about 250 cilia that beat in a coordinated fashion to move materials across the surface of the cell
Example: the respiratory tract
The Basement Membrane
A network of protein fibers
Lies between the epithelium and underlying connective tissues
Is a place of attachment for epithelial cells
Provides strength and resists distortion
Is a barrier between underlying connective tissues and the epithelium
Epithelial Renewal and Repair
Epithelium must continually repair and renew itself
Are lost or destroyed by chemical or physical wear and tear
Stem cells
Unspecialized cells
Found deep in the epithelium near the basement membrane
Continuously divide to replace dead or damaged cells in the epithelium
Classifying Epithelia
Two types of layering:
1.
2.
Simple
Stratified
1.
2.
3.
Three Cell Shapes:
Squamous
Cuboidal
Columnar
Table 4 – 1 page 93
Cell Layers
Simple epithelium
Single layer of cells covering the basement membrane
Line ventral body cavities, heart chambers and blood vessels
Where secretions or absorption occurs – thinness reduces diffusion time
Stratified epithelium
Has several layers of cells over the basement membrane
Provides more protection
Found in areas subject to more mechanical or chemical stress
Cell Shape
1.
Squamous epithelium
Cells are thin and flat
Looks like fried eggs laid side by side
2.
Cuboidal epithelium
Hexagonal boxes in 3D view, but in sectional view look like boxes
3.
Columnar epithelium
Also hexagonal but taller and more slender
Nuclei are crowded in a narrow band close to basement membrane
Simple Squamous Epithelia
Found in protected regions where absorption takes place or where a slippery surface reduces friction
Simple Cuboidal Epithelium
Provides limited protection
Secrete enzymes and buffers in the pancreas and salivary glands
Involved in the production of urine
Simple Columnar
Provides some protection and allow for absorption and secretion
Lines the stomach, intestinal tract and many excretory ducts
Pseudostratified Epithelia
Nuclei are at varying distances from surface, it has a layered appearance
Pseudostratified columnar epithelium
It is not stratified, all cells touch basement membrane
Typically possess cilia
Lines most of the respiratory tract
Transitional and Stratified
Transitional epithelium
Withstands considerable stretching
Lines ureters and urinary bladder
Stratified squamous epithelium
Found where mechanical stresses are severe
Surface of the skin, lining of mouth, tongue and esophogus
Figure 4 – 4 and 4 – 5, pgs. 95&96
Glandular Epithelia
Produce exocrine or endocrine secretions
Exocrine
Discharge products through a duct onto some internal or external surface
Can be characterized as unicellular glands (goblet cells) or multicellular glands (secretory sheet)
Endocrine (hormones)
Produced by ductless glands and released into blood or tissues
Mode of Secretion
Each glandular cell releases secretions by one of three mechanisms:
1.
Merocrine secretion
Most common mode of secretion
Product released in vesicles by exocytosis
Mucus
2.
Apocrine secretion
Involves loss of both cytoplasm and secretory product
Outermost portion of cytoplasm becomes packed with secretory vesicles and is the shed
3.
Holocrine secretion
Entire sell becomes packed with secretions and then bursts apart and dies
Sebaceous glands
Modes of Secretion
Type of Secretion
Exocrine glands can be categorized as serous, mucous or mixed
Serous Glands
Watery solution containing enzymes
Mucous glands
Secrete mucins that form a thick, slippery mucus
Mixed glands
Contain both serous and mucous glands together
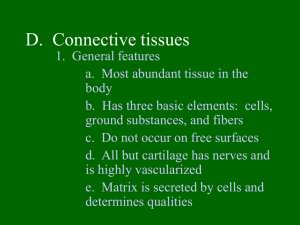
Connective Tissues
All have three basic components:
1.
2.
3.
Specialized cells
Protein fibers
Fluid known as ground substance
Protein fibers and ground substance form the matrix that surrounds the cells
Accounts for most of the volume of connective tissue
Connective Tissue Functions
Support and Protection
Bony structural framework
Protect delicate organs
Transportation of materials
Fluid connective tissues
Storage of energy reserves
Adipose cells (fat)
Defense of the body
Antibodies
Classifying Connective Tissues
1.
Connective tissue proper
Many types of cells and matrix fibers in a ground substance
Tissue under skin, fatty tissue, and tendons and ligaments
2.
Fluid connective tissues
Distinct cells in a watery ground substance with dissolved proteins
Blood and lymph
3.
Supporting connective tissues
Matrix of dense ground substance and closely packed fibers
Cartilage and bone
Connective Tissue Proper
Some cells are “permanent residents,” and others are not always present because they leave to defend and repair areas of injured tissue
The Cell Population
Fibroblasts – most abundant cells
Produce and maintain connective tissue fibers and ground substance
Macrophages – “big eater” cells
Phagocytize damaged cells or pathogens
Mobilize immune system
Fat cells – adipocytes
Large droplet of lipid that pushes nucleus and organelles to one side of the cell
Mast cells – found near blood vessels
release chemicals to begin body’s defensive activities after an injury or infection
Antibodies, white blood cells and stem cells
Connective Tissue Fibers
1.
Collagen fibers
Long, straight and unbranched
Strong and flexible, most common
2.
Elastic fibers – contain protein elastin
After stretching return to original length
3.
Reticular fibers – least common
Commonly form a branching, interwoven framework in various organs
Ground Substance
Fills spaces between cells and surrounds fibers
Clear, colorless and has consistency of maple syrup
Slows movement of bacteria and other pathogens
Loose Connective Tissue
Areolar tissue
Contains all cells and fibers found in connective tissue proper
Extensive blood supply
Forms a layer that separates the skin from underlying muscles
Provides padding and allowing movement
Adipose Tissue; Figure 4 – 9 pg. 102
Loose connective tissue containing large numbers of fat cells
Provides more padding and shock absorption for body
Insulation and energy storage
Dense connective tissue
Mostly collagen fibers
Two types: dense regular and dense irregular
Dense regular connective tissue
Collagen fibers packed tightly, parallel to one another
Tendons – attach muscle to bone
Ligaments – attach bone to bone; often contain elastic fibers
Dense irregular connective tissue
Interwoven network of collagen fibers
Provides support to areas subjected to stresses from many directions
Fluid Connective Tissues
Blood and lymph
Proteins dissolved in watery matrix do not form fibers
Watery matrix is plasma in blood
Red blood cell – makes up ½ of volume of blood
Transport oxygen
White blood cell – component of immune system
Platelets – cell fragments that function in blood clotting
Lymph forms as interstitial fluid enters small passageways, or lymphatic vessels
Cells of immune system monitor the composition of lymph
Supporting Connective Tissues
Cartilage and bone
Cartilage
Matrix of a firm gel with embedded fibers
Chondrocytes – only cells found in matrix
Live in small pockets called lacunae
Avascular – limits repair capabilities
Perichondrium
Structure that separates cartilage from surrounding tissues
TYPES OF CARTILAGE
1.
Hyaline cartilage – most common
Closely packed collagen fibers
Tough but flexible
Connects ribs to sternum, supports respiratory tract, and covers opposing bone surfaces
2.
Elastic cartilage – numerous elastic fibers
Elastic flap of ear and epiglottis
3.
Fibrocartilage – little ground substance, lots of collagen
Extremely durable and tough
Spinal column, between pubic bones and pelvis and in a few joints
Resist compression, absorb shocks and prevent damaging bone – bone contact
Figure 4 – 10, page 104
Bone (osseous tissue)
Lacunae contain osteocytes (bone cells) and surround blood vessels
Canaliculi
Branching network within bony matrix
Periosteum
Covering of bone that has outer fibrous and inner cellular layers
Table 4 – 3 page 105
Membranes
Form barriers or cover and protect structures and tissues
Four types:
1.
Mucous membranes
2.
3.
4.
Serous membranes
Cutaneous membranes
Synovial membranes
Mucous Membranes
aka mucosae, line cavities that communicate with exterior
Kept moist at all times
Most lined by simple epithelia
Also simple columnar, stratified squamous and transitional squamous
Line the digestive, respiratory, reproductive and urinary tracts
Serous Membranes
Line the sealed, internal subdivisions of the ventral body cavity
Three kinds:
1.
Pleura – covering the lungs
2.
Peritoneum – lines organs of abdominal cavities
3.
Pericardium – covers the heart
Has parietal and visceral portions
Friction is reduced by water, serous fluid
The Cutaneous Membrane
Skin
Covers surface of the body
Thick, relatively waterproof, and usually dry
Synovial Membranes
Joins or articulations are surrounded by a synovial membrane
Ends of bones are covered by hyaline cartilage and separated by viscous synovial fluid
Helps lubricate the joint and permits smooth movement
Muscle Tissue
Specialized for contraction
Involves interaction between filaments of myosin and actin
Three types in the body:
1.
2.
3.
Cardiac
Skeletal
Smooth
Skeletal Muscle Tissue
Contains large, multinucleated cells
Are usually called muscle fibers
Produced through division of stem cells
Partial repairs can occur after injury
Marked by a series of bands called striations
Nervous system provides voluntary control over its activities
Striated voluntary muscle
Cardiac Muscle Tissue
Only found in the heart
Cells are interconnected at intercalated discs
Specialized attachment sites containing gap junctions and desmosomes
Very limited ability to repair itself
Do NOT rely on nerve activity
Specialized cells called pacemaker cells establish a regular rate of contraction striated involuntary muscle
Smooth Muscle Tissue
Walls of blood vessels, around hollow organs, and in layers around the respiratory, circulatory, digestive and reproductive tracts
No striations
Cells are able to divide
Regenerate after injury
Nonstriated involuntary muscle
Neural Tissue
Specialized for conduction of electrical impulses from one region of the body to another
Two types of cells:
Neurons – communicate through electrical events that affect their cell membranes
Neuroglia - provide physical support for neural tissue, maintain the chemical composition of the tissue fluids, supply nutrients to neurons and defend the tissue from infection
Neurons
Longest cells in your body (up to 39 in.)
Cannot divide – very limited ability to repair themselves
Contain three parts:
1.
Cell body – w/ large nucleus
2.
Dendrites – numerous branching projections
3.
Axon – long and slender part, communicate with other cells
End at synaptic terminals
Tissue Injuries and Repair
Inflammation – area is isolated from healthy tissue while damaged cells are cleaned up.
Swelling, warmth, redness and pain
Regeneration – second phase of following injury
Fibroblasts produce dense network of collagen fibers known as
scar tissue or fibrous tissue
Over time, scar tissue is remodeled and resumes normal appearance
Is more successful in some tissues than others
Permanent replacement of normal tissues is called fibrosis