Sciatic
advertisement

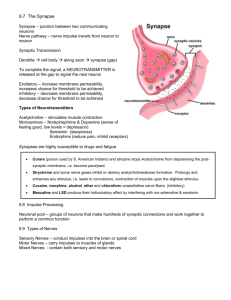
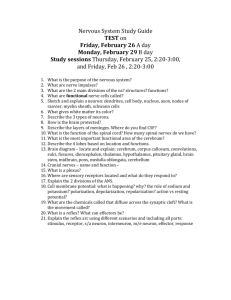
Biology 220 Anatomy & Physiology I Unit VIII SPINAL NERVES, RECEPTORS AND REFLEXES Chapter 13 pp. 475-483, 491-507 E. Gorski/ E. Lathrop-Davis/ S. Kabrhel Spinal Nerves • pass through intervertebral foramina (between vertebrae) • all are mixed (sensory/motor) • areas served: ° entire body ° in head/neck - spinal nerves only provide innervation for sympathetic division of ANS - other head/neck innervation comes from cranial nerves) Number and Naming • 31 pairs of nerves ° cervical -- 8 pair ° thoracic -- 12 pair ° lumbar -- 5 pair ° sacral -- 5 pair ° coccygeal -- 1 pair • cervical (in red) are named after the vertebra (in blue) below them (except C8); others (eg., T1 in orange) named after the vertebra above them C1 C1 C8 T1 T 1 Fig. 12.24, p. 463; see also Fig. 13.5, p. 491 Spinal Nerve Composition • Ventral root -- carries motor (efferent = outgoing) fibers (axons) of lower motor neurons and autonomic motor neurons • Dorsal root -- carries afferent (incoming) fibers from sensory neurons • Dorsal root ganglion -- consists of cell bodies of first-order sensory neurons ° sensory neurons are unipolar with a peripheral process extending from receptor toward cell body and a central process extending away from cell body and entering spinal cord Spinal Nerve Branches Spinal nerve formed from union of dorsal and ventral root continues for about 2 cm then branches into rami (mixed fibers): a. dorsal ramus -- serves skin and muscles of back b. ventral ramus -- primarily serves skin, muscles of anterior trunk and limbs c. rami communicantes (singular = ramus communicans) -- carry autonomic motor fibers between ventral ramus and autonomic ganglia Spinal Rami Dorsal Ramus Ventral Ramus Ramus communicans See Fig. 13.6, p. 492 Fig. 14.6, p. 521 Regeneration of Neurons: PNS • cell bodies -- if cell body is damaged, cell dies; neurons “downstream” from damaged neuron may die as well. • peripheral axons (PNS) ° portion of axon distal to site of damage is degraded within 1 week ° neurolemma usually remains intact (depends on severity of damage; myelin sheath degenerates) ° axon regrows at about 1-5 mm per day ° Schwann cells that form cord will eventually remyelinate regenerated axon Regeneration of Neurons: PNS Steps: 1. macrophages enter area and phagocytize debris after Wallerian degeneration of distal axon and myelin sheaths (neurilemma remains intact) 2. Schwann cells proliferate in response to mitosisstimulating chemicals released by macrophages 3. Schwann cells release nerve growth factor (NGF) and other chemicals that stimulate axonal growth 4. Schwann cells also form cellular cords which axon follows during regeneration Regeneration of Neurons: PNS Fig. 13.3, p. 482 Regeneration of Neurons: CNS • • • • CNS macrophages phagocytize debris more slowly than peripheral macrophages do normally, neuron dies because oligodendrites (supplying myelin sheath) associated with damaged neuron die, so do not aid regeneration of axon (fiber) nearby astrocytes may proliferate and produce scarring myelin sheaths (oligodendrites) of other, nearby axons secrete inhibitory proteins or die (secondary demyelination) ° note: in experiments, macrophages transplanted from outside CNS can secrete proteins that inhibit inhibitory proteins Nerve Plexuses Plexuses formed from branching and rejoining of ventral rami in cervical, lumbar and sacral regions (not in thoracic region) • each nerve leaving plexus contains fibers from several spinal nerves • muscles of limbs receive innervation from more than one spinal nerve • Thoracic spinal nerves T2-T12 do not form plexuses; they innervate external and internal intercostal muscles Cervical Plexus Formed from the ventral rami of C1-C5 • found in neck region under sternocleidomastoid muscle • sensory innervation from skin on back of neck, ear, over parotid gland, shoulder • motor innervation to lower muscles of neck, deep muscles of neck, trapezius, sternocleidomastoid • Phrenic nerve provides motor (and sensory) innervation to diaphragm Fig. 13.7, p. 494 Brachial Plexus Formed from ventral rami of C5-T1 (may get fibers from C4 and/or T2) • located in the inferior lateral neck and axillary region • serves arm and lateral shoulder, chest (pectoralis major and minor muscles) Major nerves: • Median • motor to flexor muscles of forearm (flexor carpi radialis, flexor digitorum superficialis) • sensory from skin of lateral 2/3 of hand Fig. 13.8, p. 496 Brachial Plexus: Major Nerves • • Radial ° motor to posterior arm extensors (triceps brachii), wrist extensors, supination (supinator), and thumb abduction ° sensory from posterior arm Ulnar ° motor to flexor muscles of anterior forearm (flexor carpi ulnaris) intrinsic muscles of hand (other than palm) ° sensory from medial 1/3 of hand (anterior and posterior) Fig. 13.8, p. 496 Brachial Plexus: Major Nerves • Axillary ° motor to deltoid and teres minor ° sensory from skin of shoulder region • Musculocutaneous ° motor to flexor muscles of arm (biceps brachii, brachialis) ° sensory from anterolateral forearm (varies) Fig. 13.8, p. 496 Lumbar Plexus Formed from ventral rami of L1-L4 • Femoral nerve ° motor to anterior muscles of thigh (thigh flexion and knee extension: quadriceps femoris) ° sensory from medial leg and foot, anterior thigh • Obturator nerve ° motor to thigh adductors (adductor magnus, brevis, longus) ° sensory from skin of medial thigh Fig. 13.9, p. 498 Sacral Plexus Formed from L4-S4 • Sciatic nerve ° motor to posterior thigh (hamstrings), posterior and anterior lower leg (gastrocnemius, soleus, tibialis anterior) and adductor magnus (posterior portion) ° sensory from posterior skin Fig. 13.10, p. 500 Sacral Plexus • • Superior gluteal nerve ° motor to gluteus medius Inferior gluteal nerve ° motor to gluteus maximus Fig. 13.10, p. 500 Dermatomes • Area of skin innervated by cutaneous branches of single spinal nerve (all spinal nerves except C1) • dermatomes: ° trunk -- C2-T12 ° arm -- ventral rami of C5-T1 (sometimes T2) ° anterior leg -- ventral rami L1-S1 Fig. 13.11, p. 501 Dermatomes ° posterior leg and perineum -ventral rami of S2-S5 Fig. 13.11, p. 501 General Sensory Receptors • Classification based on: 1. Location 2. Type of stimulus detected 3. Structural complexity 1. Location • • • exteroceptors -- at body surface (skin); detect pain, temperature, pressure, touch interoceptors -- internal organs, blood vessels proprioceptors -- measure degree of stretch in muscles, tendons, joints, ligaments 2. Type of Stimulus Detected • mechanoreceptors -- respond to touch, pressure, vibration, stretch (when they or surrounding tissues are deformed) • thermoreceptors -- respond to heat or cold • photoreceptors -- respond to light energy (lightgated channels) • chemoreceptors -- respond to chemicals in solution (taste, smell, blood chemistry; chemically-gated channels) • nociceptors -- pain (chemicals released during tissue damage) • itch receptors - respond to histamine NOTE: over stimulation of any receptor causes pain 3. Structural Complexity Complex receptors ° associated with special senses (sight, hearing, smell, taste) ° involve more complex structures and tissues Simple receptors -- most common ° modified dendritic endings of sensory neurons associated with general senses ° found in epithelia, muscles, and connective tissues ° free dendritic endings or encapsulated receptors (mechanoreceptors) Free Dendritic Endings = naked dendritic endings • most are unmyelinated fibers (type C) • examples: ° free nerve endings -- pain, temperature, some mechanoreceptors (Merkel discs) ° root hair plexuses -- mechanoreceptors of hair movement Simple Encapsulated Receptors Meissner’s corpuscles -- fine touch in skin • Krause’s end bulbs -- touch in mucous membrane of mouth and eyes (conjunctiva), lips • Pacinian corpsuscles -- pressure and vibration in dermis, tendons, joint capsules; also found in viscera • Ruffini’s endings -- deep pressure and stretch in dermis, hypodermis, joint capsules • Simple Encapsulated Receptors • muscle spindles -- stretch in skeletal muscle • Golgi tendon organs -- stretch in tendons • joint kinesthetic receptors (Pacinian and Ruffini corpuscles, free dendritic endings, Golgi tendonlike organs) -- stretch, joint position, motion ° located in joint capsule of synovial joint ° important of proprioception Reflexes • Rapid, predictable, unlearned, involuntary motor response to specific stimuli • integrates sensory input with motor output without involving higher centers • used clinically to test condition of nervous system Fig. 13.12, p. 502 Components of the Reflex Arc 1. receptor -- specialized dendritic end 2. sensory neuron -- unipolar neuron carrying incoming impulse from receptor 3. integrating center within gray matter of spinal cord ° single synapse between sensory and motor = monosynaptic ° with interneuron = polysynaptic 4. motor neuron -- carries outgoing impulse to effector 5. effector -- muscle or gland that responds to motor impulse Types of Spinal Reflexes • • • • • Stretch reflex* ° Patellar reflex* ° Achilles' reflex* Flexor reflex Crossed extensor reflex Deep tendon reflex Superficial reflex* ° Plantar Reflex* (Babinski sign) *Lab Flexor Reflex=Withdrawal Reflex • • • • • polysynaptic, ipsilateral initiated by painful stimulus, which results in contraction of flexor to withdraw body part from stimulus may be intersegmental (may involve more than one spinal cord segment) may involve more than one muscle group e.g., moving hand away from flame Fig. 13.17, p.507 Crossed Extensor Reflex • • e.g., arm being grabbed (also stepping on Lego) two components: 1) ispilateral flexor reflex - afferent fibers (via dorsal root) --> ipsilateral interneuron (gray matter of spinal cord) --> ipsilateral flexor reflex (contraction of flexor on same side) 2) contralateral extensor reflex - same afferent fibers --> interneurons on opposite side (cross through gray commissure; contralateral) --> inhibit motor neuron to flexor on opposite side and stimulate motor neuron to extensor Crossed Extensor Reflex (con’t) Fig. 13.17, p.507 Deep Tendon Reflex • protects against over-stretching of tendon • causes inhibition (relaxation) of contracting muscle; stimulation of ipsilateral antagonist • steps: —> stimulation of Golgi tendon receptors —> afferent impulses to spinal cord enter through dorsal root —> synapse with interneurons to motor neuron of contracting muscle causing inhibition and stimulates motor neuron to antagonist muscle causing contraction Deep Tendon Reflex Fig. 13.16, p. 506