The Neurological examination
advertisement

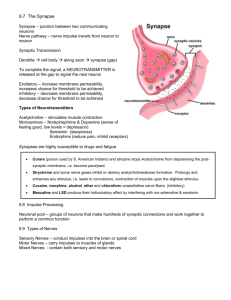
The Neurological examination Neurosurgical approach Step 1 – CT and/or MRI Step 2- Prof. Moshe Gomori Just that! • • • • • • • Mental status, cognition & language Cranial nerves Signs of meningeal irritation Motor system Sensory system Cerebellar functions Gait and balance • Remember that normal range of findings dynamically changes with age. • We all have some soft neurological signs – be symptoms oriented and try to look at the entire picture and not on a soft abnormal finding. Mental status, cognition & language Glasgow Coma Scale Glasgow Coma Scale – Children modified Speech evaluation • If during conversation you suspect any language abnormality test spontaneous conversation (fluency, paraphasia), understanding commands, low and high frequency naming, repetition, reading, writing. Distinguished and define dysarthria. • Aphasia/Disphasia → Globally/Sensory/Motor Meningeal irritation - nuchal rigidity Meningealism Cranial Nerves CN I - Olfactory Anosmia • • • • • • • • • • • • • • • • • • • • • • • • • • • • Upper respiratory tract infection (e.g., sinusitis or the common cold) Nasal polyps Idiopathic hypogonadotropic hypogonadism Hypothyroidism Head trauma, damage to the ethmoid bone Dementia with Lewy bodies Tumors of the frontal lobe Fibromyalgia Multiple sclerosis Hypoglycaemia Diabetes Asthma or Allergy Hayfever Chronic obstructive pulmonary disease (COPD) Long term alcoholism Cushing's syndrome Exposure to a chemical that burns the inside of the nose Stroke Epilepsy Radiation therapy to the head and neck Liver or kidney disease Parkinson's disease Alzheimer's disease Toxins (especially acrylates, methacrylates[ and cadmium) Old age Kallmann syndrome Primary ciliary dyskinesia Post-perfusion syndrome Laryngectomy with permanent tracheostomy Esthesioneuroblastoma is an exceedingly rare cancerous tumor that originates in or near the olfactory nerve. Symptoms are anosmia (loss of sense of smell) often accompanied by chronic sinusitis.[23] Intranasal drug use Samter's triad Foster Kennedy syndrome Cadmium poisoning Smoking Neurotropic virus Schizophrenia Pernicious anemia Zinc deficiency Bell's Palsy or nerve paralysis and damage Idiopathic intracranial hypertension Suprasellar meningioma Refsum's disease Adrenergic agonists or withdrawal from alpha blockers (vasoconstriction) Sarcoidosis Zinc-based intranasal cold products, including remedies labelled as "homeopathic" Chronic atrophic rhinitis Paget's disease of bone[ Cerebral aneurysm Wegener's Granulomatosis Primary amoebic meningoencephalitis Myasthenia gravis Foster-Kennedy Syndrome • • • • Optic atrophy in the ipsilateral eye Papilledema in the contralateral eye Central Scotoma in the ipsilateral eye Anosmia ipsilaterally “This syndrome is due to optic nerve compression, olfactory nerve compression, and increased ICP secondary to a mass.” CN II - Ophthalmic Visual Acuity Finger counting? Hand movements? Light perception? Visual fields (confrontation) Pupils (also CN III) Optic discs CN III(Oculomotor) , IV(Trochlear) & VI (Abducens) Distant large movements in 6 directions plus convergence Full coordinated movements, no pathological nystagmus CN III(Oculomotor) , IV(Trochlear) & VI (Abducens) CN V - Trigeminal Pinprick to compare sides in the distribution of the 3 branches CN VII - Facial Lower face Smile or blow chicks Upper face Forcefully close eyes or lift eye browses CN VII - Facial CN VIII - Vestibulocochlear Rub fingers, hair or paper near each hear separately CN VIII - Vestibulocochlear Damage to the vestibulocochlear nerve may cause: • hearing loss • vertigo • false sense of motion • loss of equilibrium (in dark places) • nystagmus • motion sickness • gaze-evoked tinnitus CN IX & X – Glossopharyngeal and vagus Look for deviation of the uvula, lowering of palatal arch or a coarse voice CN IX & X – Glossopharyngeal and vagus CN IX • general sensory fibers → from the tonsils, the pharynx, the middle ear and the posterior 1/3 of the tongue. • sensory fibers → (taste) posterior one-third of the tongue. • visceral sensory fibers→ from the carotid bodies, carotid sinus. • parasympathetic fibers → parotid gland via the optic ganglion. • motor fibers → to stylopharyngeus muscle, the only motor component of this cranial nerve. • pharyngeal plexus. CN X - Pneumogastric nerve • • • • • • • • • • • • Auricular nerve Pharyngeal nerve Superior laryngeal nerve Superior cervical cardiac branches of vagus nerve Inferior cervical cardiac branch Recurrent laryngeal nerve Thoracic cardiac branches Branches to the pulmonary plexus Branches to the esophageal plexus Anterior vagal trunk Posterior vagal trunk Hering-Breuer reflex in alveoli CN XI - Accessory Sternocleidomastoid – ask patient to turn head against resistance (contralateral to turning direction) Trapezius - press shoulder against patient resistance CN XII - Hypoglossal Look for atrophy or fasciculations while mouth slightly open and tongue rests on the floor of the mouth Ask patient to stick tongue out CN XII - Hypoglossal Motor System • Observe •Passive tone • Muscle force • Reflexes Observe exposed limb / trunk No asymmetry, atrophy (hypertrophy) or fasciculations. No involuntary movements, or abnormal posture. Test passive tone by asking the patient to relax and moving his upper and lower limbs. Look for mild weakness by asking patient to close his eyes, stretch his arms with his palms up. Pronator drift Muscle strength grading Compare muscle force on both sides: Deltoid Biceps Triceps Grip (many muscles) Iliopsoas Quadriceps femoris Gastrocnemius Tibialis anterior Hamstrings (opposite) Deep Stretch reflexes Muscle Nerve Root Biceps Musculocutaneous C 5-6 Triceps Radial C 6-8 Brachioradialis Radial C 5-6 Quadriceps femoris Femoral L 2-4 Gastrocnemius S 1-2 Tibial Use reflex hammer as a pendulum: Biceps Triceps Quadriceps femoris Gastrocnemius Brachioradialis Test for pathological pyramidal release sign (Babinski): Equivalent signs: Plantar-flexion of toe Babinski Suspect pathological increased reflexes or wish to better localize lesion? Hoffman Tromner Ankle clonus: Abruptly dorsoflexed ankle. Supra-patellar reflex Pectoral reflex Cross-adductors reflex Suspect frontal lesion? Neurodegenerative disease? Check frontal release signs. Palmo-mental Snout Grasp Glabellar tap What is the origin of muscle weakness? Upper motor neuron Lower motor neuron Atrophy (in chronic disease) Severe with fasiculations None or mild due to disuse Tone Decreased Spastic in chronic stage, spastic or decreased in acute stage Deep tendon reflexes Decreased Increased Babinski sign Negative Positive Remember – motor system is not just about weakness but also deals with abnormal involuntary movements, fine movements etc and possible localization is not just upper vs. lower motor neurons but also frontal lobes, basal ganglia and cerebellum. Sensory Exam Sensory Exam Pinprick to compare sides and proximal vs. distal sensation. Ignore uncertain differences. Suspect peripheral neuropathy, spinal posterior columns involvement or hemi-spinal syndrome? Use you tuning fork. Ask patient to stand, close eyes and stretch arms (Romberg test) Remember you are testing proprioception (large diameter fibers, posterior spinal columns) and the integrative function of the vestibular system rather then cerebellar functions. Cerebellar functions Finger to nose test (slow): Alternating palm movements: Finger on target without significant corrections (dysmetria) or tremor at the end of the movement (intention tremor) Smooth and regular movements (no dysdiadochokinesia) Heel-to-shin test is the equivalent to finger-tonose test Gait & Balance While patient is bared-foot (if possible): Natural walking: Tandem walking (heel to toe): Steps are regular and in normal length, base in narrow and posture is erect. Patients younger than 65 years are expected to succeed - CVA - Head Trauma - Brain Tumor - CP - MS - UMN lesion - Parkinson - Liver failure - Multiple sclerosis - Spinal cord trauma - Spinal cord tumor - Syphilitic meningomyelitis - Foot drop - Polio - MS - Guillain-Barré - Spinal disc herniation - Fibular nerve Injury - Spondylolisthesis - Myopathy gait - Pregnancy - Cong. hip dysplasia - Muscular dystrophy - Spinal musc. atrophy Thanks!