Ch24.Urinary.System.Lecture_1
advertisement

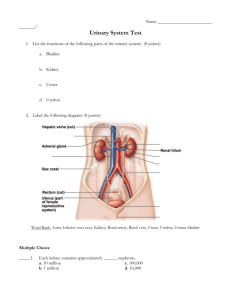
The Urinary System Ch 24 C. Babaian Human Anatomy Sonya Schuh-Huerta, Ph.D. Outline • Historical perspective • Kidney overview • Nephron structure & function • Ureters, Bladder & Urethra • Hot research • Disorders/diseases Organs of the Urinary System • • • • Kidneys Ureters Urinary bladder Urethra Why study the kidney? What does it do? L. Da Vinci, 1508 The kidney: a vital organ with many functions Filters the blood -Removal of wastes & toxins -Waste products: urea, uric acid, creatinine -Production of urine Homeostasis -Body fluids & pressure Kidney -Ions (Na+, K+, Cl-, Ca2+, HCO3-) -Acid-base balance Ureter -Blood sugar Production of hormones -Blood volume & pressure -Calcium metabolism -Red blood cell production Bladder What can urine tell us? • Historical interest in resolving urine’s composition & relation to health • Alchemists of Medieval Europe thought urine contained gold! • Urea isolated in 1773; 1st organic compound to be artificially synthesized Gerrit Dou, 1617 Urine color wheel What can urine tell us? • Yellow color: breakdown products of hemoglobin Modern-day urine color wheel Urine color & components tell a lot about a person’s health Salt & water balance • Huge variation in amount & concentration of urine • Kidney’s job: keep salt & water balanced (input = output) • Maintain osmolarity of ~300 mOsmol/L Matt Stonie, competitive eater The kidneys Renal artery Renal hilum Renal vein Kidney Ureter Urinary bladder Urethra Location & gross anatomy In almost all animals including humans Paired, “kidney” bean-shaped organs Located in the abdominal cavity: T12 – L3 Within the retroperitoneum Left kidney behind spleen Top of right kidney behind liver Hilum opening where renal artery, vein, & ureter join kidney Surrounded by fibrous capsule, fat & fascia Dorsal view Position of the kidneys Anterior Inferior vena cava Aorta Peritoneum Peritoneal cavity (organs removed) Renal vein Renal artery Renal fascia anterior posterior Perirenal fat capsule Body of vertebra L2 Fibrous capsule Body wall Posterior 12th rib Supportive tissue layers Gross anatomy of the kidney Renal cortex Renal medulla Major calyx Papilla of pyramid Renal pelvis Minor calyx Ureter Renal pyramid in renal medulla Renal column Fibrous capsule Gross anatomy of the kidney renal capsule medulla renal pelvis hilum Blood vessels of the kidney Cortical radiate vein Cortical radiate artery Arcuate vein Arcuate artery Interlobar vein Interlobar artery Segmental arteries Renal vein Renal artery Renal pelvis Ureter Renal medulla Renal cortex (a) Frontal section, posterior view, illustrating major blood vessels Blood vessels of the kidney Aorta Inferior vena cava Renal artery Renal vein Segmental artery Interlobar vein Interlobar artery Arcuate vein Arcuate artery Cortical radiate vein Cortical radiate artery Afferent arteriole Peritubular capillaries and vasa recta Efferent arteriole Glomerulus (capillaries) Nephron-associated blood vessels (see Figure 24.9) (b) Path of blood flow through renal blood vessels The kidney • Contains ~1 million tubular structures = nephrons • Carry out functions of the kidney At the microscopic level Nephron – the functional unit • Glomerulus & Bowman’s capsule • Proximal tubule • Loop of Henle • Peritubular capilaries & Vasa recta • Distal tubule • Collecting duct cortex Edward Sales First part of the nephron • Renal corpuscle Bowman’s capsule + glomerulus • Glomerulus = tuft of porous capillaries • Bowman’s capsule = surrounds glomerulus Glomerulus Madelaine Dela Cruz Glomerulus Glomerular filtration • Holds back proteins & RBCs • Allows small molecules through: Water Ions (Na+, Cl-, K+, Ca2+, HCO3-) Glucose Amino acids Urea & uric acid Efferent arteriole Glomerular capsular space Afferent arteriole Glomerular capillary covered by podocytes Proximal convoluted tubule Outer layer of Bowman’s capsule Glomerular filtration • Glomeruli – Porous capillaries – Fed & drained by afferent & efferent arterioles • Efferent arteriole has smaller diameter – Filter 1 liter of fluid every 8 minutes! • 180 liters of fluid per day • Total blood volume is filtered ~60X/day! Filtration membrane • Filter between blood in glomerulus & space of Bowman’s capsule 1. Endothelium of capillary 2. Basement membrane 3. Slits between foot processes of podocytes Cytoplasmic extensions of podocytes Filtration slits Podocyte cell body Fenestrations (pores) Glomerular capillary endothelium Foot processes of podocyte How does the nephron work? 1) Filtration Afferent arteriole Glomerulus – Blood filtrate leaves glomeruli Efferent arteriole 2) Reabsorption – Nutrients (glucose), H2O, & essential ions taken back into blood Bowman’s capsule Renal tubule 3) Secretion – Active process of removing undesirable chemicals from blood – Dumping them into tubules 4) Excretion – Filtrate leaves as urine Peritubular capillary Filtration Reabsorption Secretion Urine Different cell types & functions Renal cortex Renal medulla Glomerular capsule: parietal layer Renal pelvis Basement membrane Ureter Kidney Podocyte Renal corpuscle Glomerular capsule Glomerulus Fenestrated endothelium of the glomerulus Distal convoluted tubule Proximal convoluted tubule Glomerular capsule: visceral layer Microvilli Mitochondria Highly infolded plasma membrane Proximal convoluted tubule cells Cortex Medulla Distal convoluted tubule cells Thick segment Thin segment Loop of Henle Descending limb Ascending limb Collecting duct Nephron loop (thin-segment) cells Principal cell Collecting duct cells Intercalated cell Glomerular Filtration Rate • Glomerular Filtration Rate (= GFR) Volume of fluid filtered by the glomeruli per unit time 180 L/day or 125 ml/min – Can only be measured by compounds that are not reabsorbed or secreted Coupling of water reabsorption to Na+ reabsorption Lumen Tubule Cell Peritubular Capillary H2O Na+ H2O H2O H2O Na+ Na+ Na+ H2O Na+ Na+ low Na+ H2O Na+ Na+ H2O Na+ Na+ Na+ Na+ NaK H2O ATP ATPase + Na K+ H2O Na+ H2O Na+ K+ Na+ H2O Na+ H2O H2O Proximal convoluted tubule • Most solutes are reabsorbed here • All glucose is reabsorbed • Drugs/toxins are secreted • Filtrate is isoosmotic Loop of Henle • Ascending limb permeable to Na+, not H2O • Descending limb permeable to H2O, not Na+ • Concentrates medulla • Part of urine-concentrating system Countercurrent multiplier system Friedrich Henle, 1873 Countercurrent Multiplier System • Fluids in adjacent tubes running in opposite directions – promotes the exchange of material – Build-up of concentration – Movement of solutes – Examples in nature & mimicked in industry – Loop of Henle! Loop of Henle Cortical nephron • Cortical nephrons Juxtamedullary nephron Efferent arteriole Cortex • Juxtamedullary nephrons – Loop of Henle plunges deep into medulla Afferent arteriole Efferent arteriole Peritubular capillaries – Vasa recta Corticomedullary junction Vasa recta – Set up the concentration gradient of medulla – Create driving force for maximal H2O reabsorption from collecting ducts Collecting duct Medulla high osmolarity The kidney cortex & medulla cortex Edward Sales medulla Benjamin Yates Blood vessels of nephrons • Peritubular capillaries – Capillary network of cortical nephrons – Adapted for absorption • Low-pressure, porous capillaries • Vasa recta – Capillary network of juxtamedullary nephrons – Thin-walled looping vessels • Descend deep into the medulla – Part of the kidney’s urine-concentrating mechanism Adaptations of the kidney • Desert animals conserve H2O – Many long Loops of Henle – Highly concentrated urine (uric acid) – Urine “pellet” medulla Benjamin Yates Kangaroo rat Distal convoluted tubule • Permeable to (actively pumps) Na+ out of tubule • Impermeable to H2O • Filtrate hypoosmotic Collecting duct • Reabsorption of Na+ under hormonal control –Aldosterone (from adrenal gland) • Reabsorption of H2O under hormonal control –Antidiuretic hormone, ADH (from posterior pituitary) • The nephrons fine-tune the final concentration of urine based on body’s needs How does the nephron fine tune the reabsorption of Na+ and water? Juxtaglomerular Apparatus • Regulates salt & fluid balance • Special cells: granular cells & the macula densa Red blood cell Efferent arteriole Proximal tubule Macula densa cells of the ascending limb Lumens of glomerular capillaries Extraglomerular mesangial cells Granular cells Afferent arteriole Mesangial cells between capillaries Juxtaglomerular apparatus Juxtaglomerular Apparatus • Granular cells Modified smooth muscle cells of aff. arteriole –Make renin • Macula densa Cells of distal ascending limb –Monitors solute concentration (Na+) –When BP is low (GFR low) Na+ low signals granular cells to secrete renin •Renin-Angiotensin System (RAS) Regulates sodium & fluid balance (& BP) Plasma Volume / Blood Pressure Macula densa Vascular & atrial pressure GFR / Flow / Posterior pituitary Antidiuretic hormone NaCl Granular cells Renin Collecting ducts from Liver Angiotensin II Aquaporin channels H2O Reabsorption Adrenal gland Aldosterone Excretion of salt & H2O Fluid Volume / BP Collecting ducts Sodium Reabsorption Renin-Angiotensin System • Many drugs interrupt steps of this system • Used to treat high BP (hypertension), congenital heart disease, kidney disease, etc. diuretics • Caffeine & alcohol also diuretics Rest of the urinary system: Ureters • Carry urine from the kidneys to the urinary bladder • Oblique entry into bladder prevents backflow of urine • Histology of ureter – Mucosa transitional epithelium – Muscularis 2 layers • Inner longitudinal layer • Outer circular layer – Adventitia typical connective tissue Transitional Epithelium – Review… • Description: – Has characteristics of stratified cuboidal & stratified squamous – Superficial cells dome-shaped when bladder is relaxed, squamous when full • Function: permits distension of urinary organs by urine • Location: epithelium of urinary bladder, ureters, proximal urethra Transitional Epithelium (h) Transitional epithelium Description: Resembles both stratified squamous and stratified cuboidal; basal cells cuboidal or columnar; surface cells dome shaped or squamous-like, depending on degree of organ stretch. Transitional epithelium Function: Stretches readily and permits distension of urinary organ by contained urine. Location: Lines the ureters, bladder, and part of the urethra. Basement membrane Connective tissue Photomicrograph: Transitional epithelium lining the bladder, relaxed state (390); note the bulbous, or rounded, appearance of the cells at the surface; these cells flatten and become elongated when the bladder is filled with urine. Histology of the ureter Lumen Longitudinal layer Transitional epithelium Lamina propria Mucosa Circular layer Muscularis Adventitia Urinary bladder • A collapsible muscular sac • Stores & expels urine – Full bladder spherical • Expands into the abdominal cavity – Empty bladder lies entirely within the pelvis Urinary bladder • Urachus closed remnant of the allantois • Prostate gland – In males (not females!) • Lies directly inferior to the bladder • Surrounds the urethra Urinary bladder Ureter not illustrated in (b) Uterus Urachus Urinary bladder Ductus deferens Pubic symphysis Prostate gland Vagina Urethra (a) Sagittal section through male pelvis, urinary bladder shown in lateral view (b) Sagittal section through female pelvis Urinary bladder • Urinary bladder is composed of 3 layers 1. Mucosa transitional epithelium 2. Thick muscular layer detrusor muscle 3. Fibrous adventitia Histology of the urinary bladder Lumen of bladder Transitional epithelium Lamina propria Muscular layer (detrusor) Transitional epithelium Basement membrane Adventitia (with fat cells) (a) Micrograph of the bladder wall (17X) Lamina propria (b) Epithelium lining the lumen of the bladder (360X) Urethra • Epithelium of urethra – Transitional epithelium • At the proximal end (near the bladder) – Stratified & pseudostratified columnar mid-urethra (in males) – Stratified squamous epithelium • At the distal end (near the urethral opening) Urethra • Internal urethral sphincter – Involuntary smooth muscle • External urethral sphincter – Voluntarily inhibits urination – Relaxes when one urinates Urethra • In females – Length: 3–4 cm • In males 20 cm in length; 3 named regions: – Prostatic urethra • Passes through the prostate gland – Membranous urethra • Through the urogenital diaphragm – Spongy (penile) urethra • Passes through the length of the penis Structure of urinary bladder & urethra Peritoneum Ureter Rugae Detrusor muscle Adventitia Ureteric orifices Trigone of bladder Bladder neck Internal urethral sphincter Prostate Prostatic urethra Membranous urethra External urethral sphincter Urogenital diaphragm Spongy urethra Erectile tissue of penis (a) Male. The long male urethra has three regions: prostatic, membranous, and spongy. External urethral orifice Structure of urinary bladder & urethra Peritoneum Ureter Rugae Detrusor muscle Ureteric orifices Bladder neck Internal urethral sphincter Trigone External urethral sphincter Urogenital diaphragm (b) Female Urethra External urethral orifice Micturition Pons Pontine micturition center (+) 2 2 Integration in pontine micturition center initiates the micturition response. Descending pathways carry impulses to motor neurons in the spinal cord. Lower thoracic or upper lumbar spinal cord 4 (–) Inferior hypogastric ganglion Hypogastric nerve 3 Parasympathetic efferents stimulate contraction of the detrusor muscle and open the internal urethral sphincter. Sacral spinal cord Pelvic nerves 1 Bladder (+) (–) Internal urethral sphincter 1 Visceral afferent impulses from stretch receptors in the bladder wall are carried to the spinal cord and then, via ascending tracts, to the pontine micturition center. 3 Pelvic splanchnic nerves 5 External urethral sphincter 4 Sympathetic efferents to the bladder are inhibited. 5 Somatic motor efferents to the external urethral sphincter are inhibited; the sphincter relaxes. Urine passes through the urethra; the bladder is emptied. Visceral afferent Sympathetic Somatic efferent Parasympathetic Interneuron Hot Research • Adult reprogrammed cells (iPSCs) regenerate entire kidney in vivo (Usui et al., Amer J Path, 2012) Disorders affecting the kidneys • Diabetes mellitus (“flowing through” “sweet”) – Huge sugar load glucose in the urine & causes osmotic diuresis; can result in low BP, coma & death • Diabetes insipidus – Lack antidiuretic hormone (ADH) massive amount of dilute urine & dehydration • Renal calculi (kidney stones) – Too much salt, Ca2+, uric acid precipitates out of solution & blocks urine flow; very painful Disorders affecting the kidneys • Renal Disease & Failure –Glomerular dysfunction –Slowed GFR, massive reabsorption of salt & water, severe hypertension, edema –Dialysis & Kidney Transplants Disorders of the urinary system • Urinary tract infections – More common in females – Burning sensation during micturition • Bladder cancer – 3% of cancers more common in men • Kidney cancer – Arises from epithelial cells of nephron tubules Disorders of the urinary system • Congenital defects of the urogenital tract – Hypospadias –Abnormal placement of urethral orifice (opening); urethra opens anywhere along the urethral groove on ventral side of penis or scrotum –One of most common birth defects in boys (~1 out of 125 boys) –More severe forms interfere with urination & sexual function! –Most forms are correctable with surgery Disorders of the urinary system • Pelvic Floor Disorders dropping down (prolapse) of the bladder, urethra, small intestine, rectum, uterus, or vagina, caused by weakness of or injury to the tissues of the pelvic floor –Incontinence often develops –Only occurs in women –Incidence increases with age (1 in 3 over age 65) Urinary system throughout life: fetus • Embryo develops 3 pairs of kidneys • Only 1 persists to become kidney • By fetal week 8 kidney & nephrons fully formed • Produces urine by fetal month 3 • Contributes to amniotic fluid! Urinary bladder Gonad Urethra Kidney Anus Ureter 8-week fetus Rectum Urinary system throughout life: adult • Kidney & bladder function declines with advancing age – – – – – – Nephrons decrease in size & number Tubules less efficient at secretion & reabsorption Filtration declines Recognition of desire to urinate is delayed Loss of muscle tone in bladder & sphincters Incontinence can develop • And Yes,… exercise can help! Kegels Summary • Importance of the kidney & role in salt & water balance • Structure & function of the entire kidney, nephron, ureters, bladder & urethra Questions…? What’s Next? Madelaine Dela Cruz Lab: Urinary & Reproductive Systems Mon Lecture: Reprod & Endo Systems Mon Lab: Student Presentations & Potluck! & Endo Sys Wed Lecture: Finish Endo Sys & Review Wed Lab: Lab Exam 5! Review: Anatomy of the Kidney Review: Anatomy of the Nephron (Boron & Boulpaep, Med Phys., 2003) Renal Clearance • Renal Clearance (= RC) Volume of blood plasma from which a particular substance (x) is completely cleared RCx = Ux · V Px Where Ux = concentration in urine V = flow rate of urine Px = concentration in plasma – RC of creatinine & inulin = GFR – RC of glucose = 0 Why?