to find the lecture notes for lecture 6 nervous tissue click here
advertisement

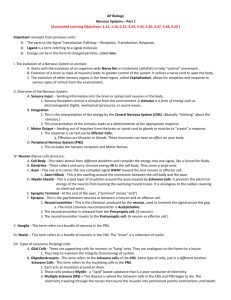
THE NERVOUS SYSTEM: NEURAL TISSUE Nervous system functions • 1. sensory function – sensory receptors detect internal and external stimuli – information is sent to CNS via sensory (afferent) neurons within sensory nerves • 2. integrative function – – – – – • integrates = processing of information within the CNS stores info and also makes decisions once info is processed one important integrative function = perception processed by interneurons within the CNS 90% of the neurons within the CNS are interneurons 3. motor function – decision usually manifests itself as a motor command – contraction of a muscle, secretion by a gland – motor commands travel along motor (efferent) neurons within motor nerves – commands are sent to effectors = muscles and glands Nervous system includes all neural tissue in body • about 3% of the total body weight • Central Nervous System – Brain and spinal cord (brain = 100 billion neurons, SC = 100 million neurons) • Peripheral Nervous System – All neural tissue outside CNS – includes the spinal and cranial nerves A schematic of the vertebrate nervous system Figure 21-6 Cells in Nervous Tissue • Neurons • Neuroglia Neuroglia (Glia) • • • • • • “glue” about half the volume of cells in the CNS smaller than neurons 5 to 50 times more numerous do NOT generate electrical impulses divide by mitosis – however, mature glial astrocytes may not be able to divide – only precursors to glial populations • • regulate the clearance of neurotransmitters participate in neural development – provide growth factors and chemical cues for the development of neurons and their axonal processes • Two types in the PNS – Schwann cells – satellite cells • Four types in the CNS – – – – Astrocytes Oligodendrocytes Microglia Ependymal cells Astrocytes • • • Largest of glial cells Most numerous Star shaped with many processes projecting from the cell body -two types: protoplasmic, fibrous -protoplasmic – short branches, found in gray matter -fibrous – many long unbranched processes, found in white matter -processes make contact with the capillaries supplying the CNS, the neurons of the CNS and the pia mater membrane covering the brain and spinal cord • Help form and maintain blood-brain barrier – processes wrap around the blood capillaries and isolate the neuron from the blood supply -also secrete substances that maintain a unique permeability for the endothelial cells that line these capillaries – restricts movement of substances out of the blood • Provide structural support for neurons – • • • • • • microfilaments within cytoskeleton Maintain the appropriate chemical environment for generation of nerve impulses/action potentials Regulate nutrient concentrations for neuron survival Regulate ion concentrations - generation of action potentials by neurons Take up excess neurotransmitters – take up excess GABA and glutamate Assist in neuronal migration during brain development Perform repairs to stabilize tissue – scar formation??? Oligodendrocytes • fewer processes than astrocytes • round or oval cell body • Each forms myelin sheath around the axons of neurons in CNS • Analogous to Schwann cells of PNS • Form a supportive network around CNS neurons Microglia • few processes • derived from mesodermal cells that also give rise to monocytes and macrophages • • • Small cells found near blood vessels 15% of the glial cells of the CNS Phagocytic role - clear away dead cells – derived from hematopoietic stem cells • • protect CNS from disease through phagocytosis of microbes migrate to areas of injury where they clear away debris of injured cells - may also kill healthy cells Ependymal Cells • epithelial cells arranged in a single layer • range in shape from cuboidal to columnar • Form epithelial membrane lining cerebral cavities (ventricles) & central canal - that contain CSF • Produce & circulate the cerebrospinal fluid (CSF) found in these chambers • CSF = colourless liquid that protects the brain and SC against chemical & physical injuries, carries oxygen, glucose and other necessary chemicals from the blood to neurons and neuroglia PNS: Satellite Cells • Flat cells surrounding PNS axons • Support neurons in the PNS • help regulate the chemical environment surrounding the neurons PNS: Schwann Cells • each cell surrounds multiple unmyelinated PNS axons with a single layer of its plasma membrane • Each cell produces part of the myelin sheath surrounding an axon in the PNS • contributes regeneration of PNS axons Neurons •what is the main defining characteristic of neurons? •have the property of electrical excitability - ability to produce action potentials or impulses in response to stimuli Representative Neuron http://www.horton.ednet.ns.c a/staff/selig/Activities/nervou s/na1.htm 1. cell body or soma (or perikaryon) -single nucleus with prominent nucleolus (high synthetic activity) -Nissl bodies -rough ER & free ribosomes for protein synthesis -proteins then replace neuronal cellular components for growth and repair of damaged axons in the PNS -neurofilaments or neurofibrils give cell shape and support - bundles of intermediate filaments -microtubules move material inside cell -lipofuscin pigment clumps (harmless aging) - yellowish brown -the processes that emerge from the body of the neuron = nerve fibers -two kinds: dendrites & axons Neurons 2. Cell processes = dendrites (little trees) - the receiving or input portion of the neuron -short, tapering and highly branched -surfaces specialized for contact with other neurons -cytoplasm contains Nissl bodies & mitochondria 3. Cell processes = axons • • • • • • • • • • • Conduct impulses away from cell bodypropagates nerve impulses to another neuron Long, thin cylindrical process of cell contains mitochondria, microtubules & neurofibrils - NO ER/NO protein synth. joins the soma at a cone-shaped elevation = axon hillock first part of the axon = initial segment most impulses arise at the junction of the axon hillock and initial segment = trigger zone cytoplasm = axoplasm plasma membrane = axolemma Side branches = collaterals arise from the axon axon and collaterals end in fine processes called axon terminals Swollen tips called synaptic end bulbs contain vesicles filled with neurotransmitters Axonal Transport • Cell body is location for most protein synthesis – neurotransmitters & repair proteins • however the axon or axon terminals require proteins – e.g. neurotransmitters • Axonal transport system moves substances – slow axonal flow • movement of axoplasm in one direction only -- away from cell body • movement at 1-5 mm per day • replenishes axoplasm in regenerating or maturing neurons – fast axonal flow • • • • moves organelles & materials along surface of microtubules at 200-400 mm per day transports material in either direction for use in the terminals or for recycling in cell body Axonal Transport & Disease • fast axonal transport route by which toxins or pathogens reach neuron cell bodies – – – – tetanus (Clostridium tetani bacteria) – toxin = tetanospasmin disrupts motor neurons causing painful muscle spasms “lockjaw” – muscle stiffness usually involves jaw and neck first interferes with the release of neurotransmitters that result in inhibition of muscle contraction – neuronal targets are peripheral motor end plates, CNS, sympathetic NS – lethal dose = 2.5 ng per kg body weight (e.g. 70 ng for 175 lbs) • bacteria enter the body through a laceration or puncture injury – more serious if wound is in head or neck because of shorter transit time to the brain Structural Classification of Neurons • Based on number of processes found on cell body – multipolar = several dendrites & one axon • most common cell type in the brain and SC – bipolar neurons = one main dendrite & one axon • found in retina, inner ear & olfactory – unipolar neurons = one process only, sensory only (touch, stretch) • develops from a bipolar neuron in the embryo - axon and dendrite fuse and then branch into 2 branches near the soma - both have the structure of axons (propagate APs) - the axon that projects toward the periphery = dendrites Structural Classification of Neurons • Named for histologist that first described them or their appearance •Purkinje = cerebellum •Renshaw = spinal cord • others are named for shapes e.g. pyramidal cells Functional Classification of Neurons • Sensory (afferent) neurons – transport sensory information from skin, muscles, joints, sense organs & viscera to CNS • Motor (efferent) neurons – send motor nerve impulses to muscles & glands • Interneurons (association/integrative) neurons – connect sensory to motor neurons – 90% of neurons in the body The Nerve Impulse Terms to know • membrane potential = electrical voltage difference measured across the membrane of a cell • resting membrane potential = membrane potential of a neuron measured when it is unstimulated – results from the build-up of negative ions in the cytosol along the inside of the neuron’s PM – the outside of the PM becomes more positive – this difference in charge can be measured as potential energy – measured in millivolts • • • • polarization depolarization repolarization hyperpolarization Ion Channels • • • • ion channels in the PM of neurons and muscles contributes to their excitability when open - ions move down their concentration gradients channels possess gates to open and close them two types: gated and non-gated 1. Leakage (non-gated) or Resting channels: are always open, contribute to the resting potential -nerve cells have more K+ than Na+ leakage channels -as a result, membrane permeability to K+ is higher -K+ leaks out of cell - inside becomes more negative -K+ is then pumped back in 2. Gated channels: open and close in response to a stimulus A. voltage-gated: open in response to change in voltage - participate in the AP B. ligand-gated: open & close in response to particular chemical stimuli (hormone, neurotransmitter, ion) C. mechanically-gated: open with mechanical stimulation The resting potential, generated mainly by open “resting”, non-gated K+ channels -the number of K+ channels dramatically outnumbers that of Na+ -however, there are a few Na leak channels along the axonal membrane AXON ECF Graded potentials • local changes in membrane potential that occur in varying intensities (grades) – caused by the opening of ion channels in a region of the axonal membrane • usually ligand-gated or mechanically-gated channels – typically gated ion channels for sodium – results in a slight depolarization = graded potential – region that is being depolarized = active area • stronger the triggering event = stronger the graded potential that results – the stronger the trigger the more ion channels open, the greater the depolarization • spread by passive current flow – because a local area has begun to depolarize – charge of this area changes – specifically the inside area gets more positive in relation to the surrounding areas that are at rest – the outer area becomes more negative in relation to the surrounding areas that are at rest – this produces a current that starts to spread to the surrounding areas – depolarizing them • BUT they die over short distances – this current decreases as it travels further from the originating area Action Potential • • • • • Resting membrane potential is 70mV triggered when the membrane potential reaches a threshold usually -55 MV if the graded potential change exceeds that of threshold – Action Potential Depolarization is the change from 70mV to +30 mV Repolarization is the reversal from +30 mV back to -70 mV) • action potential = nerve impulse • takes place in two stages: depolarizing phase (more positive) and repolarizing phase (more negative - back toward resting potential) • followed by a hyperpolarizing phase or refractory period in which no new AP http://www.blackwellpublish can be generated ing.com/matthews/channel. html depolarization (increase in MP) results from opening of Na+ channels. This opens an increasing number of voltage-gated Na channels which depolarizes the membrane more. Once threshold is reached, a large # of voltage-gated Na+ channels open and a rapid increase in MP results outflow of K+ restores the resting MP. Na+ channels begin to open and K+ channels close. K+ outflow results in hyperpolarization (below resting) results in a refractory period. at a certain stage of depolarization, theMP also opens voltage-gated K+ channels which permit the outflow of K+ . The Na+ close and the MP becomes more negative returning toward resting MP Local Anesthetics • Prevent opening of voltage-gated Na+ channels • Nerve impulses cannot pass the anesthetized region • Novocaine and lidocaine – blocks nerve impulses along nerves that detect pain Continuous versus Saltatory Conduction • Continuous conduction (unmyelinated fibers) – An action potential spreads (propagates) over the surface of the axolemma http://highered.mcgrawhill.com/sites/0072437316/student_view0/chapter45/animations.html# Saltatory Conduction • Saltatory conduction -depolarization only at nodes of Ranvier - areas along the axon that are unmyelinated and where there is a high density of voltage-gated ion channels -current carried by ions flows through extracellular fluid from node to node http://www.blackwellpublishing.com/matthews/actionp.html Rate of Impulse Conduction • Properties of axon • Presence or absence of myelin sheath • Diameter of axon • The propagation speed of a nerve impulse is not related to stimulus strength. – Larger = faster conduction – Myelin 5-7 X faster – larger, myelinated fibers conduct impulses faster due to size & saltatory conduction Myelination increases the velocity of impulse conduction Figure 21-15 Action Potentials in Nerve and Muscle • Entire muscle cell membrane versus only the axon of the neuron is involved • Resting membrane potential – nerve is -70mV – skeletal & cardiac muscle is closer to -90mV • Duration – nerve impulse is 1/2 to 2 msec – muscle action potential lasts 1-5 msec for skeletal & 10-300msec for cardiac & smooth • Fastest nerve conduction velocity is 18 times faster than velocity over skeletal muscle fiber Synaptic Communication Synapse • Synapse • • • – Site of intercellular communication between 2 neurons or between a neuron and an effector (e.g. muscle) Permits communication between neurons and other cells – Initiating neuron = presynaptic neuron – Receiving neuron = postsynaptic neuron Most are axodendritic axon -> dendrite Some are axoaxonic – axon > axon • axon terminal swell to form synaptic end bulbs or form swollen bumps called varicosities • release of neurotransmitters from synaptic vesicles – multiple types of NTs can be found in one neuron type http://www.lifesci.ucsb.edu/~mcdougal/neurobehavior/modules_homework/lect3.dcr Synapses • NTs will cause either and excitatory or inhibitory response • If the NT depolarizes the postsynaptic neuron = excitatory – Often called an excitatory postsynaptic potential (EPSP) – Opening of sodium channels or other cation channels (inward) • Some NTs will cause hyperpolarization = inhibitory – Often called an inhibitory postsynaptic potential (IPSP) – Opening of chloride channels (inward) or potassium channels (outward) • Neural activity depends on summation of all synaptic activity – Excitatory and inhibitory Synapses • Chemical – Membranes of pre and postsynaptic neurons do not touch – Synaptic cleft exists between the 2 neurons – 20 to 50 nm – the electrical impulse cannot travel across the cleft – indirect method is required – chemical messengers (neurotransmitters) – Most common type of synapse – The neurotransmitter induces a postsynaptic potential in the PS neuron – type of AP – Communication in one direction only http://www.blackwellpublishing.com/matthews/nmj.html Chemical synapse – Is the conversion of an electrical signal (presynaptic) into a chemical signal back into an electrical signal (postsynaptic) • • • • • 1. nerve impulse arrives at presynaptic end bulbs 2. fusion of synaptic vesicles to PM - role for calcium 3. release of NTs 4. opening of channels in PM of postsynaptic neuron (e.g. sodium) 5. postsynaptic potential develops – depolarization & triggering of AP in postsynaptic neuron Chemical synapse • propagation of AP at the target post-synaptic neuron usually involves opening of ligand-gated Na+ channels on the membrane of the post-synaptic neuron – binding of NT to a receptor on post-synaptic membrane – this receptor is the ligand-gated channel Release of NTs from Synaptic end bulbs -synaptic vesicles are filled with NTs -the vesicles move into proximity near the PM of the end bulb = active zone -upon receipt of AP into these bulbs -causes the opening of voltagegated Ca2+ channels -the influx of calcium promotes the “docking” of the synaptic vesicle with the PM and the exocytosis of their contents -the synaptic vesicle components are recycled for future use Synaptic vesicles can be filled, exocytosed, and recycled within a minute Synapses • Electrical – Direct physical contact between cells required – Conducted through gap junctions – Two advantages over chemical synapses • 1. faster communication – almost instantaneous • 2. synchronization between neurons or muscle fibers – e.g. retina, heart-beat Neurotransmitters • More than 100 identified • Some bind receptors and cause channels to open • Others bind receptors and result in a second messenger system • Results in either excitation or inhibition of the target • Removal of NTs – 1. Diffusion • move down concentration gradient – 2. Enzymatic degradation • e.g. acetylcholinesterase – 3/ Uptake by neurons or glia cells • neurotransmitter transporters • e.g. NE, epinephrine, dopamine, serotonin 1. small molecules: Acetylcholine (ACh) • All neuromuscular junctions use ACh • ACh also released at chemical synapses in the PNS and by some CNS neurons • Can be excitatory at some synapses and inhibitory at others • Inactivated by an enzyme acetylcholinesterase • Blockage of the ACh receptors by antibodies = myasthenia gravis - autoimmune disease that destroys these receptors and progressively destroys the NMJ – Anticholinesterase drugs (inhibitors of acetylcholinesterase) prevent the breakdown of ACh and raise the level that can activate the still present receptors Neurotransmitters 2. Amino acids: glutamate & aspartate & GABA – Powerful excitatory effects – Glutamate is the main excitatory neurotransmitter in the CNS – Stimulate most excitatory neurons in the CNS (about ½ the neurons in the brain) – Binding of glutamate to receptors opens calcium channels = EPSP – GABA (gamma amino-butyric acid) is an inhibitory neurotransmitter for 1/3 of all brain synapses • GABA action is affected by a broad range of drugs called benzodiazepines – e.g. lorazepan – Ativan – e.g. diazepam - Valium • Various uses: hynoptic, sedative, anxiolytic, anticonvulsant, muscle relaxant, amnesic • Short lasting – half life is less than 12 hours – hypnotic effects – insomnia • Long lasting – half life is more than 24 hours GABA – anxiolytic effects (anti-anxiety drug) • Acts to enhance GABA – GABA – major inhibitory NT in the CNS – GABA binds to GABA receptors – several types – Benzodiazepines bind and modulate the activity of the GABAA receptor which is the most prolific NT receptor in the brain • GABAA receptor is comprised of 5 protein subunits • One subunit is the alpha subunit • BZ’s bind to the alpha subunit only and increase its affinity for binding the GABA neurotransmitter • The GABAA receptor is a ligand-gated chloride channel • Binding of GABA increases the inward flow of chloride ions which hyperpolarizes the neuron and inhibits its ability to make a new action potential • Therefore BZ’s potentiate the inhibitory effects of GABA Valium • top selling drug from 1969-1982 – GABA agonist – Also decreases the synthesis of neurosteroid hormones (e.g. DHEA, progesterone) which may regulate emotional state – Acts on areas of the limbic system, the thalamus and the hypothalamus (anti-anxiety drug) – Metabolized by the liver into many metabolites – Gives rise to a biphasic half live of 1-2 days and 2-5 days! – Lipid-soluble and crosses the blood-brain barrier very easily – Stored in the heart, the muscle and the fat – Some drugs (barbituates), anti-depressants and alchohol can enhance its effect – Smoking can increase the elimination of valium and decrease its effects Neurotransmitters 3. Biogenic amines: modified amino acids – catecholamines: norepinephrine (NE), epinephrine, dopamine (tyrosine) – serotonin - concentrated in neurons found in the brain region = raphe nucleus • derived from tryptophan • sensory perception, temperature regulation, mood control, appetite, sleep induction • feeling of well being – NE - role in arousal, awakening, deep sleep, regulating mood – epinephrine (adrenaline) - flight or fight response – dopamine - emotional responses and pleasure, decreases skeletal muscle tone Other types: a. ATP - released with NE from some neurons b. Nitric oxide - formed on demand in the neuron then release (brief lifespan) -role in memory and learning -produces vasodilation • Involved in feelings of pleasure, strength • Also mediates skeletal muscle contraction • Neurotransmitters like dopamine, serotonin, glutamate, acetylcholine etc… are secreted and then rapidly internalized by transporters in order to control their levels within the nervous system • Many drugs affect these transporters • Ritalin = methylphenidate Dopamine – – – – – Stimulant used to treat ADD, ADHD, narcolepsy amd chronic fatigue 1954 – initially prescribed for depression and narcolepsy 1960 – prescribed to children with ADD, ADHD Reason?? Might be due to an imbalance in dopamine Binds both dopamine and norepinephine transporters and inhibits their ability to take these NTs back up (keeps their levels high in the synapse) – Dopamine transporters (DAT) found in the PM of neurons (presynaptic) • • • • Transports dopamine back into the neuron along with sodium ions (symporter) This terminates the dopamine signal Chloride ions are also required to enter the neuron to prevent depolarization In adults – these transporters regulate dopamine levels • Cocaine – binds and inhibits DATs – increasing dopamine in the synapse • Amphetamines – binds amphetamine receptors on a neuron which causes the internalization of the DAT into the neuron – increasing dopamine in the synapse Neuropeptides • widespread in both CNS and PNS • excitatory and inhibitory • act as hormones elsewhere in the body -Substance P -- enhances our perception of pain -opioid peptides: endorphins - released during stress, exercise -breaks down bradykinins (pain chemicals), boosts the immune system and slows the growth of cancer cells -binds to mu-opioid receptors -released by the neurons of the Hypothalamus and by **acupuncture the cells of the pituitary may produce loss enkephalins - analgesics of pain sensation -breaks down bradykinins (200x stronger than morphine) because of release -pain-relieving effect by blocking the release of of opioid-like substance P substances such as dynorphins - regulates pain and emotions endorphins or dynorphins Morphine • Opiate analgesic • Principal agent in opium – Acts on the CNS – Acts on the GI tract – decrease motility, decrease gastric secretion, decreases gastric empyting, increases fluid absorption • Other opiates: heroin, codeine, thebaine • Acts on the neurons of the CNS (specifically the nucleus accumbens of the basal ganglia) • Binds to the mu-opioid receptor – Found throughout the brain – especially in the posterior amygdala, the hypothalamus and thalams, the basal ganglia, the dorsal horn of the spinal cord and the trigeminal nerve – Relieves the inhibition of GABA release by presynaptic neurons – Also relieves the inhibition of dopamine release (addiction) – Binding activates the receptor and gives rise to: analgesia, euporia, sedation, dependence and respiratory and BP depression. • Acts on the immune system! – increase incidence of addiction in those that suffer from pneumonia, TB and HIV – Activates a type of immune cell called a dendritic cell – decrease their activation of B cells – decreased antibody production – decrease immune function