Ventilators - Kentucky Hospital Association
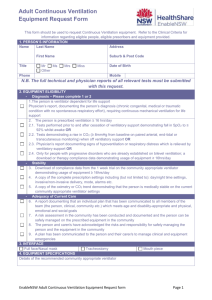
advertisement
Ventilators
Kindred Hospital Louisville
Education Module
Learning Objectives
Identify the mechanics of breathing
Identify indicators for mechanical ventilation
Identify two types of ventilators
Identify the Modes of Ventilation
Discuss the Adjuncts to Mechanical Ventilation
Identify the components of Ventilator Settings
Describe the Nursing Care of the Mechanically
Ventilated Patient
Discuss Arterial Blood Gases
Components of Respiratory System
Nasal & Oral Cavities
Nasopharynx
Oropharynx
Epiglottis
Larynx
Trachea
Left & Right Bronchus
Left & Right Lung
Alveoli
Pathophysiology of Breathing
During breathing, air is inhaled through the
airway into millions of tiny sacs where gas
exchange takes place (alveoli). Then the air
mixes with the carbon dioxide-rich gas
coming from the blood. This air is then
exhaled back through the same airways to the
atmosphere. Normally this pattern repeats
itself from 12 - 20 times a minute, but can
increase or decrease to meet our body’s
needs.
The gas exchange that takes place as
described above is the main function of the
lungs. It is required to supply oxygen to the
blood for distribution to the cells of the body,
and to remove the carbon dioxide that the
blood has collected from the cells of the body.
Pathophysiology of Breathing
Gas exchange in the lungs occurs only in the smallest airways and the alveoli.
It does not take place in the conducting airways (pathways) that carry the gas
from the atmosphere. The volume of these conducting airways is called the
anatomical “dead space” because it does not participate directly in the gas
exchange.
Gas is carried through the conducting airways through a process called
“convection”.
Gas is exchanged between the alveoli and the blood through “diffusion”.
In normal, healthy lungs the drive to breathe comes from the need to regulate
carbon dioxide levels in the blood, not from a desire to inhale oxygen.
Pathophysiology Cont’d
One of the biggest factors that determines whether
breathing is producing enough gas exchange to keep a
person adequately oxygenated is the ‘ventilation’ that each
breath is producing.
Ventilation is expressed as the volume of gas entering or
leaving the lungs in a given amount of time. It can be
calculated by multiplying the inhaled (or exhaled) volume
of a gas (Tidal Volume) times the breathing rate.
For example: A person breathing in 0.5 Liters per
respiration, who breathes 12 times a minute, has a volume
of 6 Liters/minute
Pathophysiology Cont’d
During normal breathing, the body selects a combination of tidal
volume that is large enough to clear the dead space and add fresh gas
to the alveoli, and a breathing rate that ensures the correct amount of
ventilation is produced.
There are two sets of forces that can cause the lungs and chest wall to
expand: the forces that are produced by the muscles of respiration
when they contract; and the force produced by the difference between
the pressure at the airway opening and the pressure on the outer
surface of the chest wall.
In normal respiration, the muscular force is the only one that comes
into play, when the respiratory muscles do the needed work to expand
the chest wall, decreasing the pressure on the outside of the lungs so
they expand, which draws air into the lungs.
Pathophysiology Cont’d.
When respiratory muscles are
not able to do the work required
for ventilation, the pressure at
the airway opening, and/or the
pressure at the outer surface of
the chest wall can be
manipulated to produce
breathing movements.
When altering either of those
pressures, you can do so in one
of two ways. Either increase
the pressure at the mouth and
nose, so that air is forced into
the lungs; or lower the pressure
on the chest wall external
surface.
Breathing Pathophysiology
Remember that an alteration in
any of the areas associated with
breathing/gas exchange can
produce undesirable effects in
your patient’s oxygenation.
Within the chest wall, there is
normally a constant negative
pressure that facilitates
respiration. If this negative
pressure is disrupted,
ventilation and oxygenation are
disrupted.
Lung Anatomy
Indications for Mechanical
Ventilation
Acute dyspnea
Significant respiratory acidosis
Acute or impending ventilator failure (elevated
PaCO2 {>50 mmHg} with a pH < 7.30)
Severe oxygenation deficit despite high
supplemental oxygen delivery (PaO2 < 60 mmHg
on FiO2 > 60%)
Secretion/Airway Control
Apnea, Respiratory Arrest
Common Diseases Requiring
Mechanical Ventilation
Acute Obstructive Disease: acute severe asthma; airway
mucosal edema)
Altered Ventilatory Drive: hypothyroidism; intracranial
hemorrhage; dyspnea-related anxiety
Cardiopulmonary Problems: CHF; Pulmonary
Hemorrhage
Chronic Obstructive Pulmonary Disease: emphysema,
chronic bronchitis, asthma; cystic fibrosis; bronchiectasis
Neuromuscular Disease: ALS; Guillian-Barre; Cancer;
Malnutrition; Infections
Atelectatic Disease: ARDS; Pneumonia
Other Common Conditions
Requiring Mechanical Ventilation
Burns and Smoke Inhalation: inhalation injury, surface
burns
Chest Trauma: Blunt injury; flail chest; Penetrating
Injuries
Fatigue/Atrophy: Muscle overuse; disuse
Head/Spinal Cord Injury: Meduallary brainstem injury;
Cheyne-Stokes breathing; Neurogenic Pulmonary Edema
Postoperative Conditions: Cardiac & Thoracic Surgeries;
Pharmacological Agents/Drug Overdose: Muscle
relaxants; barbiturates; Ca+ channel blockers; long-term
adrenocorticosteroids; aminoglycoside antibiotics
Two Approaches to Mechanical
Ventilation
POSITIVE
PRESSURE
VENTILATION
Uses the technique of
applying positive
pressure (relative to
atmospheric pressure)
to the airway opening
NEGATIVE
PRESSURE
VENTILATION
Uses the technique of
applying negative
pressure (relative to
atmospheric pressure) to
the external body
surface
Positive Pressure Ventilators
Simplified
For safe operation of the ventilator, the following things are required:
• Patient Interface: The ventilator delivers gas to the patient through a set
of flexible tubes called a patient circuit. This can have one or two tubes.
The circuit typically connects the ventilator to the patient to either an
endotracheal tube or tracheostomy tube.
• Power Sources: Typically these are powered by electricity or compressed
gas. The ventilator is usually connected to separate sources of compressed
air and compressed oxygen. Because compressed gas has all the moisture
removed, a humidifier is needed to moisten the gases being delivered to
the patient.
• Control System: This ensures the patient receives the desired breathing
pattern. It involves setting the parameters of the size of the breath, how
fast it is brought in & out, and how much effort the patient must exert to
signal the ventilator to start a breath.
• Monitors: A pressure monitor, as well as volume and flow sensors to
provide alarms if readings are outside the desired range.
Negative Pressure Ventilators
Simplified
For safe operation of the automatic ventilator, the following things are
required:
Patient Interface: The patient is placed inside a chamber with his or her head
extending outside the chamber. The chamber may encase the entire body
except the head(iron lung) or it may enclose just the rib cage and abdomen
(cuirass: pronounced cure-ahs). It is sealed to the body where the body where
the body extends outside the chamber.
Power Sources: Electricity powered, to run a vacuum pump that periodically
evacuates the chamber to produce the required negative pressure.
Control System: Sets breathing patterns.
Monitors: Alarms.
Modes of Mechanical Ventilation
Controlled Mandatory Ventilation:
(CMV) The patient receives a set
respiratory rate at set time intervals with a
consistent tidal volume. This is generally
only used with much sedation or paralytics,
because patient efforts do not trigger the
delivery of a breath by the machine. This is
used when the patient must not expend
energy to breathe.
Modes of Mechanical Ventilation
Assist Control: (AC) The
patient receives a set
respiratory rate at set time
intervals with a consistent
tidal volume, but when the
patient initiates a breath on
their own, the preset tidal
volume is delivered. This
decreases the patient’s
effort of breathing, and
ensures volume delivery.
Modes of Mechanical Ventilation
Synchronized Intermittent Mandatory
Ventilation (SIMV): The patient receives a
preset respiratory rate at a set tidal volume, but the
machine allows for the patient to breathe
spontaneously during the machine breaths. If the
patient breathes near the time that the machine is
prepared to deliver the preset volume, the machine
will deliver the preset tidal volume. The breaths
that the patient initiates in between the machine
breaths are not supplemented by the machine. It is
usually tolerated well by the patient, because of
the synchronicity involved.
Modes of Mechanical Ventilation
Continuous Positive Airway Pressure (CPAP):
Used either intermittently during long-term
weaning as a way to strengthen the muscles, or as
a final step before removing the patient from the
ventilator, to see how they tolerate the lack of
ventilatory assistance. All breaths are generated
by the patient, and the patient’s effort determines
the tidal volume. The machine simply provides a
continuous airway pressure, supplemental oxygen,
and apnea alarms. The continuous airway
pressure makes the effort of breathing easier for
the patient.
Modes of Ventilation
Pressure Support (PS): When this mode is
used, the patient initiates the breath, and the
inspiration ends when a preset flow amount
is delivered. The positive pressure is
applied throughout inspiration and helps to
increase the amount of tidal volume the
patient “pulls in” and decreases the energy
the patient has to use.
Adjuncts to Mechanical
Ventilation
Positive End Expiratory
Pressure (PEEP)
PEEP is the application
of continuous airway
pressure throughout
expiration. The presence
of this pressure in the
airway prevents the
complete collapse of the
alveoli, and helps
maintain that pressure
until the next inspiration
cycle begins.
Mode Review
Mode
Function
Controlled Mechanical
Ventilation (CMV)
delivers preset volume or pressure
regardless of patient’s own
inspiratory effots
Assit-Control Ventilation
Delivers breath in response to
patient effort and if paitent fails to
do so within preset amount of
time
Synchronous Intermittent
Ventilator breaths in response to
Mandatory Ventilation (SIMV)
patient effort and if patient fails to
do so within preset amount of
time
Pressure Support Ventilation (PS) Preset pressure that assists the
patient’s inspiratory effort and
decreases the work of breathing
Positive End Expiratory Pressure Positive pressure applied at the
(PEEP)
end of expiration
Continusous Positive AIrway
Pressure
Similar to PEEP but used only
with spontaneously breathing
patients
Clinical Use
Usually used for patients who are
apneic
Usually used for spntaneously
breathing patients with weakened
respiratory muscles
Usually used to wean patients
from mechanical ventilation
Often used with SIMV during
weaning
Used with CMV, A/C, and SIMV
to imporve oxygenation by
opening collapsed alveloi
Maintains constant positive
pressure in airways so resistance
is decreased
Components of Ventilator
Settings
•
•
•
•
Rate
Tidal Volume
Percentage Oxygen
Peep or Pressure Support
Rate
The rate is the number
of times the ventilator
is set to provide a
breath to the patient.
This may vary from
8-20 breaths per
minute.
Tidal Volume
Tidal volume is the amount of gas the the
ventilator is to provide to the patient with
each breath. This volume will vary based
on each patient’s height, weight, and gender.
To calculate a very rough estimate of tidal
volume, you can use 10 - 15cc per kilogram
of body weight. So a 75lb. patient might
have an ordered tidal volume of 750cc.
Percentage of Oxygen
The percentage of oxygen supplied to the
patient with every breath. This can be as
low as 40% to as much as 100%. Higher
oxygen percentages for long periods of time
increase the patient’s risk for oxygen
toxicity and other pulmonary complications.
PEEP
PEEP can be added to the regular ventilator
settings, to provide the positive end expiratory
pressure that helps to prevent the complete
collapse of the alveoli.
Pressure Support
The patient initiates the breath, and the
inspiration ends when the preset flow target
is delivered. The tidal volume will vary,
depending on the patient. The positive
pressure is applied throughout inspiration
and helps the patient to “pull in” the tidal
volume, and reduces their energy
expenditure.
Nursing Care of the
Mechanically Ventilated Patient
Nursing care of patients who are being
mechanically ventilated requires some
special considerations.
Some special considerations relate
specifically to the type of tube via which the
patient is being ventilated (i.e. endotracheal
or tracheostomy) and others related to the
patient, and the ventilator itself.
Nursing Care of the Patient with
an Tracheostomy Tube
Trach care should be performed at least every
shift, and as needed as ordered by the patient’s
Physician.
The patient should always be pre-oxygenated with
100% oxygen prior to suctioning.
Saline should not be routinely instilled into the
airway. Saline installation has been shown to
increase infection rates and to cause decreased
oxygen levels for longer periods of time than
suctioning without it.
Nursing Care of the
Mechanically Ventilated Patient
Pulmonary assessment is perhaps never as
important as it is in the mechanically
ventilated patient.
These patients require frequent
reassessments on a schedule and on an “as
needed” basis.
Further assessments can be documented in
Protouch under “Reassessments”.
Nursing Assessment
Components: Breath Sounds
Breath sounds should be assessed at least
every four hours, and more frequently as
needed.
Both the anterior and the posterior chest
need to be auscultated bilaterally.
Clearly document any adventitious breath
sounds that are heard, and report significant
alterations to the Physician.
Nursing Assessment
Components: Rate & Volume
Make sure to assess and document the
patient’s spontaneous respiratory rate and
tidal volume. This information tells you a
lot about the patient’s respiratory
functioning.
Note any changes in this area, and report
significant findings to the patient’s
Physician.
Nursing Assessment
Components:Pulse Oximetry
Pulse oximetry is a useful monitoring tool, but
provides minimal indication of the patient’s
ventilatory or acid-base status.
Readings can be affected by abnormal
hemoglobins, vascular dyes, and poor
perfusion.
Plus, the machine can’t distinguish between
normal and abnormal hemoglobins, so a
patient with carbon monoxide poisoning could
have a pulse ox reading of 100%.
Nursing Assessment
Components:Sputum
A respiratory system assessment should
include documentation of any sputum.
Note the color; tenacity; odor; frequency;
quantity; of sputum for a thorough
assessment.
Note if the patient is able to expectorate
his/her own sputum, or if suctioning is
required to remove it.
Complications of Mechanical
Ventilation
One of the reasons for such a frequent and
thorough assessment of the pulmonary
system while patients are being
mechanically ventilated is due to the many
complications that can occur with the use of
mechanical ventilation.
Thorough assessments can lead to the early
discovery of potential complications,
heading off more serious complications
later.
Complications of Mechanical
Ventilation
Positive Pressure Ventilation:
can cause:
hypotension
decreased venous return
decreased cardiac output
Other complications:
pneumothorax
subcutaneous emphysema
air embolus
localized pulmonary hyperinflation
nosocomial infections
increased intracranial pressure (cerebral edema)
ABG Overview
Understanding ABG’s
are critical to
understanding the
respiratory status of
the patient.
As a nurse, it is
essential you have a
working knowledge of
ABG’s. That
responsibility cannot
be “delegated” to R.T.
ABG Components:
pH
PCO2
HCO3
Base Excess/Deficit
PaO2
pH
pH is the relative
acidity or baseness of
the blood.
Normal human blood
pH ranges from 7.35 7.45
Less than 7.35 is
considered acidotic
and greater than 7.45
is considered alkalotic
pH
Conditions that alter
the pH of blood fall
into one of four
processes.
One or more of these
processes may be
present in a patient
with an abnormal
acid-base status.
Four Processes:
Metabolic Acidosis
Metabolic Alkalosis
Respiratory Acidosis
Respiratory Alkalosis
Metabolic Processes
Metabolic processes are those that primarily
alter the bicarbonate concentration in the
blood. A decrease in the blood
concentration of bicarbonate leads to
metabolic acidosis, while an increase in
serum bicarbonate levels leads to metabolic
alkalosis.
Respiratory Processes
Respiratory processes alter the pH of the blood, by
changing the carbon dioxide levels. Carbon
dioxide that accumulates in the blood causes an
acid state (carbonic acid).
As respirations increase or decrease in rate, the
level of carbon dioxide in the blood varies. Faster
respirations cause decreased blood carbon dioxide
levels, and slower respirations cause less carbon
dioxide to be “blown off”, causing an increased
serum carbon dioxide level.
Respiratory Processes
Respiratory alkalosis occurs when
respirations increase, leaving less carbon
dioxide in the blood, and when respirations
decrease, the carbon dioxide level in the
blood increases, which can lead to
respiratory acidosis.
PCO2
PCO2 is the partial pressure of dissolved carbon dioxide in
the blood.
Most is excreted by the lungs, some is excreted in the
kidneys as HCO3.
Normal level is 35 - 45 mmHg.
PCO2 level is a direct indicator of the effectiveness of
ventilation
As PCO2 rises, the blood becomes more acidic and the pH
drops
As PCO2 decreases the blood becomes more alkaline an
pH rises
If a change in the PCO2 level is the primary alteration, then
a respiratory problem exists
HCO3
Bicarbonate is the primary buffer in the
body. Buffers neutralize acids.
Normal range is 22 - 26 mmHg.
As the HCO3 level rises, the blood becomes
more alkaline and the pH increases.
As the HCO3 level falls, the blood becomes
more acidic and the pH decreases.
If a change in HCO3 is the primary
alteration, then a metabolic problem exists.
Base Excess/Deficit
Measures the excess amount of acid or base
present in blood. This is independent of
changes in PCO2, so it’s a measure of
metabolic acid-base balance.
Increased HCO3 = base excess (alkalosis)
Decreased HCO3 = base deficit (acidosis)
PO2
The amount of oxygen dissolved in plasma
Normal is 80 - 100 mmHg in healthy people
breathing room air at sea level.
Normal PO2 will decrease with altitude and
aging.
PO2 > 60mmHg may be considered
acceptable in critically ill, mechanically
ventilated adults.
Adequacy of PO2 must be weighed against
the potential for oxygen toxicity
Analyzing Blood Gas Results
Use the following simple four step process
to interpret ABG’s.
Practice this until you are completely
comfortable with it.
Keep a “cheat sheet” with this information
written down and refer to it!
Practice, Practice, Practice!!!
Interpreting ABG’s
Step One: Check each pH
PaCO2
value against each
HCO3normal
BE/BD
Step Two
Determine primary
problem
pH
acid 7.35 —
7.45 base
base 35 — 45
mmHg acid
acid 22 — 28
mmol/L base
acid —2 — + 2
base
Is the pH
result acid or
base?
Note that PaCO 2
readings move in the
opposite direction to
the other 2 readings
we are looking at.
• Indicates whether the
patient has primary
acidosis or alkalosis?
Interpreting ABG’s
Step Three
Determine type of
problem by
matching with pH
PaCO2
HCO3-
Which of these two
results matches the
acid or base
derangement of the
pH?
• If PaCO2 matches, the
problemis respiratory
• If HCO3- matches, the
problem is metabolic?
Step Four
Determine
compensation
Absent?
What is happening
to the non-matching
value (from the
value that matched
the pH)?
Is it moving in the
opposite direction
yet to effect a
change in the acid
base ratio and
return the pH to
normal?
pH is back to
normal but there is
still evidence of
prior abnormality.
• Non-matching is
normal and pH still
abnormal =
compensation absent
ie no compensation so
the problem is acute
• Non-matching is
abnormal and pH still
abnormal = partial
compensation
• Non-matching is
normal and pH is normal
= complete
compensation
(important when
assessing pervious
problem)
Partial?
Complete?
Other Considerations
Consider the patient’s Chronic lung conditions
overall health and
Recent ventilator
disease processes.
changes.
For every year past age Recent changes in
60, the normal value for
patient status (i.e.
pO2 drops by 1 mmHg.
codes, decannulation,
Oxygen the person is
etc. )
receiving.
Hemoglobin level
Case Study
Mr. Hill has been on the ventilator for 24
hours. You volunteered to care for him
today, since you know him from
yesterday. The settings ordered by the
pulmonologist after intubation were as
follows: A/C, rate 14, VT 700, FIO2 60%.
Since 0700, Mr. Hill has been assisting
the ventilator with a respiratory rate of
24 (It’s now 1100).
Problem #1
Describe Mr. Hill’s ventilator settings.
Problem #2
You notice that Mr. Hill’s Which lab test should
pulse oximetry has
you check to find out
been consistently
what his true
documented as 100%
ventilatory status is?
since intubation. You
also notice that his
respiratory rate is quite
high and that he’s
fidgety, doesn’t follow
commands, and doesn’t
maintain eye contact
when you talk to him.
He hasn’t had any
sedation for 24 hours.
Problems 3 & 4
#3
#4
Which two parameters What are some possible
on the ABG will give
causes of Mr. Hill’s
you a quick overview
increased respiratory
of Mr. Hill’s status?
rate?
Give the nursing
interventions you would
do because of the
possible causes too!
Case Study Continued
Mr. Hill didn’t have an ABG done this
morning, so you get an order from the
pulmonologist to get one now (1130).
When it comes back, the PaCO2 is 28,
the pH is 7.48, and the PaO2 is 120
(normals: PaCO2 35-45 mm Hg, pH
7.35-7.45 mm Hg, PaO2 80-100 mm Hg).
Problem #5
Based on the ABG, the pulmonologist
changes the vent settings to SIMV, rate
10, PS 10, FIO2 40%. The VT remains
700. Why? And, how will these new
settings help Mr. Hill?
Wrap Up
Always remember that without an intact,
functioning respiratory system, you have no
patient.
BEWARE of the words “Keep Previous”
under your nursing assessment…always
document what YOU heard, saw, smelt, felt,
etc. Don’t use “Keep Previous”!
Turn in your answers to your nurse manager!