Findings from evidence review
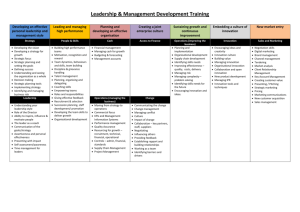
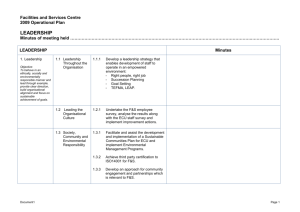
advertisement

Supporting professional nurse socialisation: Findings from evidence reviews Juan Carlos Rejon Research Analyst, RCN Chris Watts Research and Innovation Manager, RCN Appended report: Professional Socialisation: Insights from reviews of organizational culture and performance, Mark Newman & Catherine O’Keeffe, EPPI Centre Appended report: Social learning tools: are we online? Juan Carlos Rejon, RCN REPORT SUMMARY This report explores what is known about the professional socialisation of nurses, and explores strategies to support positive socialisation of nurses. The evidence reviews identify component areas of socialisation where efforts may be focused, and looks to key influences and tools in the context of the health care environment. Key findings Professional socialisation of nurses is a broad and complex topic. The terminology is commonly used as an ‘umbrella’ terms for a number of component activities relating to the education and assimilation of nurses into the professional environment. Socialisation may be usefully understood as characterised by four attributes: learning, interaction, development and adaptation. These attributes build upon three precedents: comprehensive orientation and educational programs, competent role models and adequate field experience. This report offers a picture of effective socialisation through considering these component attributes and precedents. Socialisation has a strong learning component. Learning can be formal (classes, workshops and online events) or informal on the job learning (observing, asking peers, through trial and error, working with others, coaches and mentors). Characteristics of an environment that is conducive to learning include the use of a multidisciplinary team in the delivery of teaching and assessment of educational processes, together with dedicated time, resources and assigned research staff that involve learners. Inter-professional education at undergraduate level may benefit ‘positive socialisation’, preventing stereotyped attitudes towards other health care professions and fostering positive attitudes towards the principles of team work. 1 Team training is a successful approach to improving process measures (e.g. reducing missed orders for treatment) and outcome measures (e.g. reducing mortality). There is some evidence to suggest that much of professional learning is informal. Likewise, some evidence suggests most of the investments that organisations make on learning are made on formal learning. Mentor experience is key in facilitating both formal and informal learning, and therefore supporting ‘positive’ socialisation. Mentors support students with difficulties associated with a new environment, increase self-esteem and help socialise students into the nursing role through the development circles of supportive friends and colleagues. Students learn, and may assimilate, leadership attributes by observing those displayed by mentors. Preceptorship experience is valued by newly qualified nurses, particularly when paired with preceptors who demonstrate high levels of authentic leadership. Preceptorship can have a positive effect on engagement and retention across all staff. A working environment that promotes perceptions of fair treatment towards staff has a positive effect on staff motivation and commitment to organisational goals. The value of a style of transformational leadership rather than authoritative top down practice has been observed in healthcare literature through links to safety initiatives, safety culture and improvements in safety outcomes. Engagement and wellbeing of staff is beneficial to an effective socialisation environment. There is strong evidence suggesting a positive relationship between staff wellbeing and engagement, staff reported patient care performance and patient experience of care. Assessment and improvement of organisational culture – the working environment in which the socialisation process takes place in the main – is much discussed as a key component in improving quality of care. However, assumptions that organisational culture is well defined or conceptualised may be misplaced, making it difficult to attribute a predictive casual relationship between organisational culture and organisational performance. There are potential benefits in seeking to measure how organisational culture might impact interventions to improve quality, safety and performance. These are: providing an informative overview of where a service stands; identifying areas that lag behind informing ongoing improvement; and, bringing issues about safety, quality and performance to the forefront of discussions. Social media may be playing a role in nurse socialisation. Integrating social learning tools into the work stream for professional and organisational purposes could enhance informal learning. Used effectively, these tools facilitate co-creation of content, a movement from 1-way to 2-way forms of communication, and favour a sharing approach to knowledge. 2 1. INTRODUCTION This report presents the findings of a set of evidence reviews exploring what is known about the professional socialisation of nurses. The overall review question was: What is known about strategies to support socialisation of nurses; promoting ‘positive’ socialisation and mitigating for ‘negative’ socialisation? Socialisation is a broad, complex topic and is frequently used as an ‘umbrella’ terms for a number of component activities relating to the education and assimilation of nurses into the professional environment. Given this complexity, a single review approach might provide scant understanding of the constituent elements of the socialisation process. For the purposes of this report, we have taken a pragmatic approach to understanding some of the components of socialisation, bringing these together to give insight into the overall picture of the process, and identify what effective and promising interventions are available. The report consists of set of a rapid evidence reviews examining interventions that support the ‘positive’ and / or mitigate the ‘negative’ socialisation of nurses. Structure and methodology The report begins by contextualising the review question, and describes what is meant by ‘professional socialisation’. These are broken down into three key areas: socialisation of teams; socialisation through formal education mechanisms (such as mentoring or preceptorship programmes); and impact of organisational factors (including organisational culture). A rapid evidence appraisal approach was taken to review the available literature, and searches were carried out for each of the key areas identified above. Literature searches were carried out on CINAHL, BNI and Medline databases from 2006 to present. The section on impact of organisational factors draws on commissioned work by the Evidence for Policy and Practice Information and Co-ordinating Centre (EPPI Centre) who carried out a ‘review of reviews’ examining the relationship between organisational culture and professional socialisation (Newman and O’Keefe, 2013). The EPPI Centre report is in Appendix 1. Appendix 2 presents the findings of a narrative synthesis considering emerging literature on the role of social media and social learning tools in the context of nurse socialisation. Overall, the research identified was of low quality, with little robust research indicating effective approaches to socialisation. Some research does suggest a link between interprofessional and multi-disciplinary team training and aspects of socialisation. One of the difficulties of carrying out research in this area is, as the appended EPPI Centre report explains, a lack of clarity or consensus around the concept of socialisation. Further exploration of this area may benefit from considering component parts of the socialisation process, rather than tackling the concept as a ‘whole’. That said, drawing together some of the components of socialisation does reveal an emerging picture of where mechanisms for change may lie, and these are presented here through the three key areas under consideration. 3 1. WHAT IS MEANT BY PROFESSIONAL SOCIALISATION? One purpose of this review is examine definitions of what is referred to as ‘professional socialisation’. A general definition may be a useful starting point. The Encyclopaedia Britannica defines socialisation as the process by which a human being beginning at infancy acquires the habits, beliefs, and accumulated knowledge of society through education and training for adult status.1 A useful definition from the nursing context is provided by Mackintosh (2006), who describes socialisation as the process by which individuals take on the characteristics, attitudes and values of a given profession. While the process of socialisation clearly has a strong learning component, formal education is not the only route successful learning. Informal on the job learning may account for the majority of the learning that takes place in practice (Cross, 2003; Jennings, 2010). Cross (2003) described suggests approximately 20% of learning is formal (such as classes, workshops and online events), while the remaining 80% of learning is informal (such as observing others, asking the person in the next cubicle, calling the help desk, trial-and-error, coaches, mentors and simply working with people in the know). Although the focus and investment of organisations may be centred on formal learning, it may be that informal learning is of equal if not more interest and importance. In the context of nursing, socialisation (or professional socialisation) begins upon entry into the nursing education program and continues with entry into the workforce (Weis, 2002; Wolf, 2007). There are numerous definitions of socialisation within nursing literature, but the most current follows a concept analysis undertaken by Dinmohammadi et al (2013). Their concept of nurse socialisation has four critical attributes: learning, interaction, development and adaptation. The precedents of these attributes are comprehensive orientation and educational programs; competent role models; and adequate field experience. Dinmohammadi et al (2013) suggest that professional socialisation is the consequence of both educational programs and professional environments, leading to positive and negative outcomes. Desired outcomes are the acquisition of a professional identity, ability to cope with professional roles, professional and organisational commitment, and thus improvement in the quality of care. Undesired outcomes may be the consequence of improper management of initial professional experiences, and include low motivation and productivity, demoralization, and decreased care of patients. Negative forms of socialisation can also cause other undesired consequences, such as frequent turnover, continuance of ritualised practice and bureaucratic views, role ambiguities, lack of critical thinking, repeated dismissal requests, increased attrition, and gradual desensitisation about humanistic patients needs. Socialisation may have both positive and negative consequences. Given this, there is clearly benefit in understanding the factors that can influence professional socialisation in a nursing context in order to maximize the desired outcomes of socialisation and minimize the unintended or negative ones. Our analysis of these discussions indicates that socialisation is a complex topic and not one that lends itself to understanding through a single definition. For the purpose of this report, we have considered three facets of socialisation drawn from the literature described above: socialisation of teams, including inter-disciplinary team working and training; 1 http://www.merriam-webster.com/medical/socialisation 4 socialisation through formal education mechanisms, particularly mentoring and preceptorship; impact of organisational factors, including cultural and leadership factors. 2. SOCIALISATION THROUGH TEAMS A rapid evidence review carried out for this report explored learning interventions that supported ‘positive’ socialisation as an outcome, with a focus on inter-professional and multidisciplinary team training. A search of CINAHL, BNI and Medline databases from 2006 to present was carried out to identify learning interventions that supported ‘positive’ socialisation as an outcome. Findings indicate the importance inter-professional working, together with multi-disciplinary team training as important in supporting the ‘positive’ socialisation of nurses, both in being integrated into a team (feeling ‘part’ of a team) and in subsequently in working effectively as a team. There are some promising indications that inter-professional collaboration interventions can improve health care processes and outcomes (Zwarenstein et al., 2009). A key recommendation from the Willis Commission (2012) emphasises the need to socialise health care professionals into interprofessional teams: “Interprofessional learning must play a key role in continuing professional development. Training professionals in teams must also have a much stronger focus in preregistration nursing education.” (Willis Commission, 2012, p.38) The review looked at outcomes of team training across different disciplines. Numerous organisations, including The Joint Commission and the Institute of Medicine in the US, have recommended team training as an effective approach to reducing medical errors (Institute of Medicine , 2001; Joint Commission, 2004; Kohn et al., 2000). Studies of the benefits of interprofessional learning interventions aimed at practice based changes are likely to employ process measures (such as: safety reporting, documentation of discharge decisions) or outcome measures (such as: length of stay, mortality) (Neily et al., 2010). Other complex industries, in which high risk has to be managed with extreme care (including the aviation industry) have used concepts of crew resource management to support safety and quality (Salas et al., 1995, Salas et al., 2001). Generally, the process of collaboration and its link to health care outcomes has not been systematically examined (Goldman et al., 2009). This review identifies studies that have reported improvements in process measures and/or in outcome measures in healthcare to highlight the potential of team training in improving the safety of a process and ultimately the impact of team training in a ‘hard’ outcome such as mortality. There are some studies that link team training to such beneficial outcomes. A recent US study of a piloted team training initiative in an outpatient oncology setting (Bunnell et al., 2013) used a train-the-trainer model to achieve a reduction in the incidence of missing orders for unlinked visits2 from 30% to 2%. 92% of breast cancer staff completed the training. Prevention of errors was supported by self reported improvements in efficacy and safety of care by over 70% by providers, infusion nurses and support staff. There was a likely positive effect on team dynamics, such as more respectful behaviour and improved relationship among team members. Patient satisfaction scores also improved. To achieve 2 Infusion visits at which chemotherapy is administered but a physician visit does not occur. 5 improvements in processes such as preventing missing orders for unlinked visits, a steering committee identified weaknesses in the process of writing orders, and added a control to it. The pharmacist on the committee noted that preparatory planning occurred in the pharmacy two days prior to visits. Using this opportunity to note the absence of orders, the pharmacist agreed to send reminder emails to the appropriate clinicians. This improved the process assuring a shared mental model and situational awareness for team members, which ultimately led to an improvement in the process measure (% of missing orders for unlinked visits). In another US study Neily et al. (2010) analyzed surgical mortality for facilities that received a team training program compared with those that had not yet received it. The study used crew management theory of aviation adapted for a healthcare context (Musson and Helmreich, 2004). The result was striking, with 74 facilities in the training program experiencing an 18% reduction in annual mortality (rate ratio [RR], 0.82; 95% confidence interval [CI], 0.76-0.91; P = .01) compared with a 7% decrease among the 34 facilities that had not yet undergone training (RR, 0.93; 95% CI, 0.80-1.06; P = .59). While these studies suggest the promise of teamwork training in improving safety and quality of health care, they don’t indicate a direct link to positive socialisation, but rather that an effective team is a more beneficial environment into which to be socialised. Building collaborative teams may also have an additional, indirect impact in daily work for the team members. A recent study based in neonatal intensive care reported the development of a workshop based on Team STEPPS to introduce new team-based practices (Brodsky et al., 2013). Staff satisfaction was rated higher after the training, with responses suggesting staff had greater job fulfilment. This indicates added value to team training through supporting engagement of teams (Thomas and Galla, 2013) and therefore staff. Adopting effective and appropriate approaches to team training need to be considered, and are perhaps the topic of a further review. Achieving improvements though team training is not an isolated, one-size –fits-all solution to safety and quality (Salas and Rosen, 2013). Discrepancy between expectations and goals and actual participation should be accounted for when planning team training for students. In a study of interprofessional training wards for health and social care students, the choice of setting and learning situations appeared to be crucial to the learning that occurred (Lidskog et al., 2009). The definitions explored above suggest that attitudes and values within a team are an important component of socialisation. Several studies explored how interprofessional education (IPE) can influence the attitudes of health care students towards team working. A Japanese study measured how lecture style and training style within IPE affected views of other professionals, suggesting that the introduction of IPE early in the curricula could prevent stereotyped perceptions, and change attitudes of students at an early stage (Hayashi et al., 2012). A Swedish follow-up study shows results that suggest that interprofessional training in undergraduate students education provides lasting impressions that may promote teamwork in their future professional life (Hylin et al., 2007). Half day and one day placement models of interprofessional learning amongst students had positive effects in students understanding of team working and collaborative practice (Anderson et al., 2006, Törnkvist and Hegefjärd, 2008). A UK study also shows positive results of IPE that includes facilitators and trained service users, which gave students the chance to learn and apply the principles of teamwork in putting service users at the centre of the care process (Cooper and Spencer-Dawe, 2006). A Canadian study did not find evidence of IPE curriculum at influencing attitudes of undergraduate students towards teamwork, although students were satisfied with it (Curran et al., 2010). 6 In general, the evidence seems promising of the positive effect of team training, with a higher potential if introduced early in the curricula through undergraduate IPE experiences. Students receiving IPE prepares them for the social nature of their future work within interdisciplinary teams. However, in general findings are limited. There is a lack of research examining longer term impact of IPE. Buniiss et al (2012) observe, teamwork training should not only be valued by the extent to which it may be linked to immediate quality improvements (including the introduction of an electronic workflow system into their practice processes in this particular study), but also through understanding iterative change over time (Bunniss et al., 2012). An additional piece of information that would be informative for decision makers and is usually disregarded in studies of health care education, is the cost of the intervention on top of the benefits they provide (Mazmanian, 2009). Having the evidence to assess the value for money of training and educational interventions would provide with the right arena for more informed decisions. 3. SOCIALISATION THROUGH FORMAL EDUCATION MECHANISMS In the UK nursing context there are two formal practices that can be clearly identified to support the transition from education into professional practice: mentoring (during preregistration education) and preceptorship (a structured period of support for nurses commencing professional practice). This section reports on a rapid evidence review examining how mentoring and preceptorship programmes might support professional socialisation. Mentoring The outcomes of a systematic review by Jokelainen et al (2011) provide a useful framework to understand the constituent themes of good mentorship, as have emerged from the empirical research (23 papers) from 20 years of nursing literature (1986-2006). Two themes and sub-themes are established from an inductive content analysis of this literature: 1. Facilitating students’ learning – including creating a supportive learning environment and enabling an individual learning process. 2. Strengthening students’ professionalism – including empowering development of professional attributes and identity and enhancing attainment of professional competence. Strengthening students’ professionalism could be understood as strengthening the development of professional identity and values, creating resilience in presence conflicting priorities (efficiency / thoroughness; practice reality / professional ideals), all facets of professional socialisation. Mentoring itself is complex. Jokelainen et al. (2011) describes mentoring as an integration organisational and individual viewpoints, each with a range of environmental (or contextual), collegial (working relationships), pedagogical (educational approaches) and clinical attributes. Mentors play an important role in the socialisation process: helping nursing students to be accepted and supported on clinical placements, influencing the nursing students’ ability and motivation to engage in clinical learning opportunities (Pritchard and Gidman, 2012). 7 Mentors support students with difficulties associated with a new environment, increasing their self-esteem and help socialising students into the nursing role (Bulut et al., 2010). Mentors also support students in their ‘socialisation’ within a clinical placement, easing the socialisation process, and developing circles of supportive friends and colleagues (Bulut et al., 2010, Ousey, Zannini et al., 2011). There are promising strategies in fostering the type of mentoring that facilitates students’ learning, strengthens their professionalism, develops the skills of individuals and create an environment that is favourable to learning. These strategies include use of a multidisciplinary team in the delivery of teaching and the assessment of the educational processes, and dedicated and uninterrupted time for group and individual seminars and tutorials (Ousey, 2009; Pritchard and Gidman, 2012). This should provide some insight into how mentoring can help to mitigate negative forms of socialisation maximizing the positive effects of it. Also identified are some attributes of an effective mentor. Students learn leadership attributes through observing those displayed by mentors, including: communication skills (such as communicating with patients and relations), problem solving, prioritising, and decision-making strategies (Ousey, 2009). The experience of being mentored instils values and qualities in nursing students which they can use when they are in the position of being nurse mentors themselves.(Pritchard and Gidman, 2012) Preceptorship According to the Department of Health (2011), benefits to newly registered nurses receiving preceptorship include: the development of confidence; professional socialisation into the working environment; increased job satisfaction leading to improvement in delivery quality patient care; feeling valued and respected; feeling invested in future career development; feelings of pride and commitment to their employer’s strategy and objectives; development of greater understanding of the commitment to working within nursing and the regulatory requirements; and taking personal responsibility for maintaining up-to-date knowledge. However, Robinson and Griffiths (2009) report that there is no evidence to support the contention that preceptorship had any effect on the newly registered nurses’ choice of career direction. Despite a paucity of UK evidence, current strategic direction indicates a clear interest in preceptorship and the benefits that it can provide for the professional socialisation of newly registered nurses. Preceptorship has been identified by newly registered nurses as something they want and that most of them received. Self reports by newly registered nurses identified the key function of preceptors as supporting the development and consolidation of their clinical skills (Robinson and Griffiths, 2009). There is some evidence to support the idea that preceptorship increased newly registered nurses’ levels of competence although there is little evidence to support any contention that nurses in receipt of preceptorship had any effect on the quality of care (Robinson and Griffiths, 2009). Research from Canada (Giallonardo et al., 2010) reports that newly graduated nurses paired with preceptors who demonstrated high levels of authentic leadership felt more engaged and more satisfied with the preceptee-preceptor relationship and identified this as positively affecting their job satisfaction. Similar findings on the benefits of preceptorship have been reported in relation to community nursing (Maxwell et al., 2011, Morton et al., 2011), and acute nursing in the NHS (Morgan et al., 2012). 8 Whilst the Department of Health (2011) contends that preceptorship improves retention in nursing, Robinson and Griffiths (2009) find little evidence to support this. However research from the USA suggests preceptorship can have a positive impact on the recruitment and retention of new graduate nurses and nurse preceptors (Aaron, 2011, DeWolfe et al., 2010, Sherrod et al., 2008). A recent UK systematic review identifies strong evidence that newly qualified nurses benefit from a period of supported and structured preceptorship, translating into improved recruitment and retention for the employing organisations (Whitehead et al., 2013). Overall, although there is some evidence suggesting positive effects on newly qualified nurses, there is no evidence on the clinical or cost-effectiveness of preceptorship provision in the UK, with existing studies being generally descriptive and based on self-report. Implications for professional socialisation Although the strength of the evidence around different aspects of these forms of nursing socialisation from education to professional practice is variable, it does suggests that interprofessional learning, mentoring and preceptorship can support and enhance the benefits of nurse socialisation, and ease transition from student to being part of the workforce. There are self reported benefits by nurses both receiving and providing this form of support. Further exploration is needed to understand the long-term benefits of mentoring initiatives preceptorship programmes as a form of professional socialisation. Efforts should target this form of socialisation and its potential benefits on quality of care, measurements of engagement with newly qualified nurses, and retention and satisfaction of new staff, while accounting for the most suitable strategies to make them fit within the burden of work of preceptors minimising possible unintended negative consequences on patients (e.g., making time available for preceptors to guide newly qualified nurses). Measuring whether there are adequate staffing levels to guarantee that a sufficient number of nurses is ready, available and has the time available to take on the role of mentor and preceptor would inform decision makers about adequate policies to retain and promote leadership amongst the nursing workforce. Given an anticipated shortage of nurses and an increase in the burden of work that a mandatory period of preceptorship would pose on working nurses, it would be reasonable to explore how the nursing shortage would affect workload, staff patient ratios, preceptee-preceptor ratios, and how this could influence staff turnover, job satisfaction and staff wellbeing (Masters, 2013). The debate over the regulation of health care assistants opens an interesting area of enquiry. With the high variety of nursing roles, it is important that the public, other healthcare professions, and nurses themselves have a clear insight into the different roles and responsibilities of the different nursing roles (Gardner et al., 2007). This could provide a support to staff entering new teams, such as locum practitioners, independently from where they practice. Further research should also be targeted at ways to ease and inform the ongoing implementation of the processes and resources that foster forms of mentoring and preceptorship through case studies that inform the most effective methods of delivery (Whitehead et al., 2013). 4. ORGANISATIONAL FACTORS 9 A definition of organisational culture provided in a recent scoping review by The Health Foundation (2013) makes the following connection between organisational culture and socialisation: “Culture concerns the values, beliefs and assumptions that staff infer through story, myth and socialisation, and the behaviours they observe that promote success.” (Health Foundation, 2013, p.3) This definition suggests values, beliefs and assumptions will not be a constant given, but are built as part of a process of socialisation that will be conditioned by individual experience and interactions with a given context. It also points at observed behaviours that promote success as an important element of organisational culture. The healthcare arena is a complex mosaic of role players and institutions, and defining and measuring how organisational culture affects health care is problematic. An interpretive ‘review of reviews’ commissioned from the EPPI Centre (report appended) examines the relationship between organisational culture and professional socialisation (Newman and O’Keefe, 2013). The authors examined four systematic reviews, each addressing questions about the relationship between aspects of organisational culture and organisational performance (Parmelli et al, 2011; Jung et al, 2009; Greenhalgh, 2004; Scott et al, 2003). This report challenges many of the assumptions around the possibility of measuring organisational culture, and subsequently the ability to attribute a predictive casual relationship between organisational culture and organisational performance. It suggests that many of the constituents of what is described in the reviews as professional ‘culture’ bear strong resemblance to existing descriptions of nursing socialisation (Mackintosh, 2006), indicating that an overlap in terminology defining socialisation and professional culture. Whilst the term ‘organisational culture’ is widely used, it is a poorly specified concept, with little agreement as to how it is conceptualised, and little indication as to how component conceptions differ from other organisational features, such as leadership, policy or procedures. While many instruments exist for measuring organisational culture, there is little evidence that the validity of these is tested through relationships with other measures of culture. Scott et al (2003) suggest negative or unintended consequences of organisational culture are rarely investigated, and while insights from measures might be helpful they may equally put an organisation at a disadvantage if used inappropriately (Newman and O’Keefe, 2013). This in itself problematises any ambition to examine organisational culture as an influencing factor on professional socialisation, at least from the perspective of researchbased solutions. In this respect, the authors suggest, rhetoric and a practice targeting ‘organisational cultures’ is running ahead of research. A recent systematic review by Brennan et al (2012) captures the breadth of contextual and individual factors that could be measured when evaluating continuous quality improvement (CQI) in primary care settings. Organisational culture is one of the key elements of what the authors call organisational context. The conceptual framework covers three domains influencing quality improvement in healthcare: 19 instruments measured CQI use and implementation, 51 measured organisational context (organisational culture included) and 21 measured individual level factors. This type of framework may help position the role and the type of inputs and outputs that could be expected from initiatives, with organisational culture a component of complex efforts to improve health care. The role of organisational culture within an organisational context may be one further constituent and driver of continuous quality improvement, 10 although endeavours are tempered by the challenges identified in the EPPI Centre report (Newman and O’Keefe, 2013). Scott et al (2003) analyse the relationship between organisational culture and organisational performance in healthcare. Although the claim for a link between organisational culture and performance may be overstated, the review does identify a US study that shows that cultural orientation is associated with various aspects of performance, and that such an association is worthwhile investigating. Evidence on the NHS analysed in a recent review by West and Dawson (2012) suggests employee engagement is linked to a variety of individual and organisational outcome measures, including staff absenteeism and turnover, patient satisfaction and mortality, and safety measures, including infection rates. A UK survey carried out in 2007 to 276 to primary and acute NHS trusts in England (77% response rate) showed that around a third were using a culture assessment instrument to support their clinical governance activity (Mannion et al., 2008). Almost all the tools and instruments used focused wholly or in part on the assessment of safety cultures rather than broadly on perspectives of quality and performance (Mannion et al., 2008). Recent work from the Health Foundation (2013) suggests creating a “safe space” for staff to share staff stories is important in creating a positive safety culture. They give the example of Jönköping, in which sharing staff experiences improved job satisfaction and reporting rates. The report argues that the greatest value in using tools to measure safety cultures comes from the process of bringing it to the forefront of discussions rather than from the score or assessment that the tool provides. Recent research by the National Nursing Research Unit (2013) strongly suggests a relationship between staff wellbeing and staff reported patient care performance and patient-reported patient experience. Working towards a safe culture through the creation of “safe spaces” for staff to share work related experiences could therefore have a further indirect effect through improving reporting rates, improving job satisfaction, and therefore improving patient experience of care. An innovative approach to evaluation, the PRAXIS evaluation (McCormack et al., 2013) aims to provide a way of evaluation capturing and utilising the dynamics of individual, team and organisational transformation. In this model, common with other models of evaluation such as the Participatory Action Research model, evaluation is presented as a continuous process that informs ongoing action and improvement. There is a dual focus: on the outcomes, and the processes that enable desirable outcomes to happen or not to happen. Healthcare is not the only sector dedicated to public service dealing with complex and interrelated organisational factors influencing the attitudes and behaviours of their workforce. Research from policing context into organisational factors that may influence organisational and personal practice, motivations and wellbeing of staff, and the impact of changes in management in organisations provides insight into how improvements could be made in the future. A survey carried out in 2011examined how a ‘just’ organisational culture may enhance commitment to the organisation and its goals (Porter and Quinton, 2011). The theoretical basis of this work lies on organisational justice theory (Colquitt, 2008; Greenberg, 2011). The definition of organisational justice distinguishes between two elements of organisational justice (Blader and Tyler, 2009, Tyler and Blader, 2003): procedural (at supervisory and leadership levels), and distributive (perceived fairness with which inputs and rewards are distributed in the workplace). 11 The results of the analysis provide evidence that staffs’ motivations across a range of positive behaviours are associated with their perceptions of the fairness of both their immediate supervisors and the organisation as a whole (procedural justice at leadership and supervisory levels). This is in line with the findings of a study of organisational justice and the associations found with clinical performance in health care (Elovainio et al., 2013). A rapid review on what makes great leadership by the National Policing Improvement Agency stresses the value of transformational leadership behaviours that can adapt style to suit context (Campbell and Kodz, 2011). A publication in the field of health, studying the effect of transformational leadership in patient safety, has also attributed an important role to leadership for success, in this study relating it to driving a safety culture and safety initiatives that improve safety outcomes (McFadden et al., 2009). References Aaron, C.S. (2011) The Positive Impact of Preceptors on Recruitment and Retention of RNs in Long-Term Care: A Pilot Project. Journal of Gerontological Nursing, 37, 48-54. Anderson, E., Manek, N. & Davidson, A. (2006) Evaluation of a model for maximizing interprofessional education in an acute hospital. Journal of Interprofessional Care, 20, 182194. Blader, S. L. & Tyler, T. R. (2009) Testing and extending the group engagement model: Linkages between social identity, procedural justice, economic outcomes, and extrarole behavior. Journal of Applied Psychology, 94, 445. Brennan, S. E., Bosch, M., Buchan, H. & Green, S. E. (2012) Measuring organizational and individual factors thought to influence the success of quality improvement in primary care: a systematic review of instruments. Implementation Science, 7, 1-19. Brodsky, D., Gupta, M., Quinn, M., Smallcomb, J., Mao, W., Koyama, N., May, V., Waldo, K., Young, S. & Pursley, D. M. (2013) Building collaborative teams in neonatal intensive care. BMJ Quality and Safety, 22, 374-382. Bulut, H., Hisar, F. & Demir, S. (2010) Evaluation of mentorship programme in nursing education: a pilot study in Turkey. Nurse Education Today, 30, 756-762. Bunnell, C. A., Gross, A. H., Weingart, S. N., Kalfin, M. J., Partridge, A., Lane, S., Burstein, H. J., Fine, B., Hilton, N. A., Sullivan, C., Hagemeister, E. E., Kelly, A. E., Colicchio, L., Szabatura, A. H., Winer, E. P., Salisbury, M. & Mann, S. (2013) High performance teamwork training and systems redesign in outpatient oncology. BMJ Quality and Safety, 22, 405-413. Bunniss, S., Gray, F. & Kelly, D. (2012) Collective learning, change and improvement in health care: trialling a facilitated learning initiative with general practice teams. Journal of Evaluation in Clinical Practice, 18, 630-636. Campbell, I. & Kodz, J. (2011) What makes great police leadership? What research can tell us about the effectiveness of different leadership styles, competencies and behaviours. A Rapid Evidence Review. Available online at: http://www.college.police.uk/en/docs/Great_Police_Leader_REA.pdf (accessed 8 July 2013) 12 Colquitt, J. A. 2008. Two decades of organizational justice: Findings, controversies, and future directions. The Sage handbook of organizational behavior, 73-88. Cooper, H. & Spencer-Dawe, E. A. (2006) Involving service users in interprofessional education narrowing the gap between theory and practice. Journal Of Interprofessional Care, 20, 603-617. Cross, J. (2003) Informal learning: the other 80%. Available online at http://www.internettime.com/Learning/The%20Other%2080%25.htm (accessed 8 July 2013). Curran, V., Sharpe, D., Flynn, K. & Button, P. 2010. A longitudinal study of the effect of an interprofessional education curriculum on student satisfaction and attitudes towards interprofessional teamwork and education. Journal of Interprofessional Care, 24, 41-52. Dewolfe, J., Laschinger, S. & Perkin, C. 2010. Preceptors' perspectives on recruitment, support, and retention of preceptors. Journal of Nursing Education, 49, 198-206. Dinmohammadi, M., Peyrovi, H., & Mehrdad, N. (2013) Concept Analysis of Professional Socialization in Nursing. Nursing Forum, Vol. 48, pp. 26-34. Department of Health (2011) Preceptorship framework for newly qualified nurses, midwives and allied health professionals. Journal of Perioperative Practice, 21, 334. Elovainio, M., Steen, N., Presseau, J., Francis, J., Hrisos, S., Hawthorne, G., Johnston, M., Stamp, E., Hunter, M. & Grimshaw, J. M. 2013. Is organizational justice associated with clinical performance in the care for patients with diabetes in primary care? Evidence from the improving Quality of care in Diabetes study. Family practice, 30, 31-39. Gardner, G., Chang, A. & Duffield, C. (2007) Making nursing work: breaking through the role confusion of advanced practice nursing. Journal of advanced nursing, 57, 382-391. Giallonardo, L., Wong, C. & Iwasiw, C. (2010) Authentic leadership of preceptors: predictor of new graduate nurses' work engagement and job satisfaction. Journal of Nursing Management, 18, 993-1003. Goldman, J., Zwarenstein, M., Bhattacharyya, O. & Reeves, S. (2009) Improving the clarity of the interprofessional field: implications for research and continuing interprofessional education. Journal of Continuing Education in the Health Professions, 29, 151-156. Greenberg, J. (2011) Organizational justice: The dynamics of fairness in the workplace. Greenhalgh T., Robert G., Macfarlane F., Bate P., Kyriakidou O. (2004) Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Quarterly 82(4), 581-629. Hayashi, T., Shinozaki, H., Makino, T., Ogawara, H., Asakawa, Y., Iwasaki, K., Matsuda, T., Abe, Y., Tozato, F., Koizumi, M., Yasukawa, T., Lee, B., Hayashi, K. & Watanabe, H. (2012) Changes in attitudes toward interprofessional health care teams and education in the firstand third-year undergraduate students. Journal of Interprofessional Care, 26, 100-107. Health Foundation (2013) Safety culture: what is it and how do we monitor and measure it? A summary of learning from a Health Foundation roundtable. Event report: March 2013. Available online at: http://www.health.org.uk/public/cms/75/76/313/4156/Safety%20culture%2013 %20What%20is%20it%20and%20how%20do%20we%20monitor%20and%20measure%20it .pdf?realName=xn5DLO.pdf (accessed 10 July 2013). Hylin, U., Nyholm, H., Mattiasson, A. & Ponzer, S. 2007. Interprofessional training in clinical practice on a training ward for healthcare students: a two-year follow-up. Journal of Interprofessional Care, 21, 277-288. Institute of Medicine (2001) Crossing the quality chasm: A new health system for the 21st century. National Academies Press. Jennings, C. (2010) Real learning – let’s not confuse it with completing templated exercises. Available online at http://charles-jennings.blogspot.co.uk/2010/06/real-learning-lets-notconfuse-it-with.html (accessed 8 July 2013) Joint Commission (2004) Sentinel event alert: Preventing infant death and injury during delivery. The Joint Commission: Sentinel Event Alert, Issue 30. Jokelainen, M., Turunen, H., Tossavainen, K., Jamookeeah, D. & Coco, K. (2011) A systematic review of mentoring nursing students in clinical placements. Journal of Clinical Nursing, 20, 2854-2867. Jung, T., Scott, T., Davies, H.T.O., Bower, P., Whalley, D., McNally, R., Mannion, R. (2009) Instruments for Exploring Organizational Culture: A Review of the Literature. Public Administration Review, 1087-1096. Kohn, L. T., Corrigan, J. M. & Donaldson, M. S. (2000) To err is human: building a safer health system. National Academies Press. Lidskog, M., Löfmark, A. & Ahlström, G. 2009. Learning through participating on an interprofessional training ward. Journal of Interprofessional Care, 23, 486-497. Mackintosh, C. (2006) The socialisation of pre-registration student nurses: A longitudinal qualitative descriptive study. International Journal of Nursing Studies, 43(8), 953-962 Mannion, R., Davies, H. & Konteh, F. (2008) Measuring and Assessing Organisational Culture in the NHS. Research Report by Centre for Health and Public Services Management. Masters, K. (2013) Role development in professional nursing practice. Jones & Bartlett Learning. Maxwell, C., Brigham, L., Logan, J. & Smith, A. (2011) Challenges facing newly qualified community nurses: a qualitative study. British Journal of Community Nursing, 16, 428-434. Mazmanian, P. E. (2009) Continuing medical education costs and benefits: Lessons for competing in a changing health care economy. Journal of Continuing Education in the Health Professions, 29, 133-134. McCormack, B., Manley, K. & Titchen, A. 2013. Practice Development in Nursing and Healthcare, Wiley-Blackwell. McFadden, K. L., Henagan, S. C. & Gowen, C. R. (2009) The patient safety chain: Transformational leadership's effect on patient safety culture, initiatives, and outcomes. Journal of Operations Management, 27, 390-404. 14 Morgan, A., Mattison, J. & Stephens, M. (2012) Implementing structured preceptorship in an acute hospital. Nursing Standard, 26, 35-39. Morton, S., Howes, N., Leech, S. & Smith, K. (2011) Starting with support. Community Practitioner, 84, 40-41. Musson, D. M. & Helmreich, R. L. (2004) Team training and resource management in health care: current issues and future directions. Harvard Health Policy Review, 5, 25-35. National Nursing Research Unit (2013) Does NHS staff wellbeing affect patient experience of care? Policy+Issue 39. Available online at: http://www.kcl.ac.uk/nursing/research/nnru/policy/Currentissue/Policy--Issue-39.pdf (accessed 10 July 2013). Neily, J., Mills, P. D., Young-Xu, Y., Carney, B. T., West, P., Berger, D. H., Mazzia, L. M., Paull, D. E. & Bagian, J. P. 2010. Association between implementation of a medical team training program and surgical mortality. JAMA: the journal of the American Medical Association, 304, 1693-1700. Newman, M. and O'Keefe, C. (2013) Professional socialization: insights from reviews of organizational culture and performance. Report by EPPI Centre, Institute of Education: University of London. Ousey, K. (2009) Socialization of student nurses: the role of the mentor. Learning in Health and Social Care, 8, 175-184. Parmelli, E., Flodgren, G., Schaafsma, M. E., Baillie, N., Beyer, F. R. & Eccles, M. P. (2011) The effectiveness of strategies to change organisational culture to improve healthcare performance. Cochrane Database Syst Rev, 1. Porter, G. and Quinton, P. (2011) Staff well-being, motivation and morale: gaining and using insights. Presentation available online at: http://www.crim.cam.ac.uk/events/conferences/ebp/2012/quintonorganisationaljustice.pdf (accessed 10 July 2013). Pritchard, E. & Gidman, J. (2012) Effective mentoring in the community setting. British Journal of Community Nursing, 17, 119-124. Robinson, S., & Griffiths, P. (2009) Scoping review: Preceptorship for newly qualified nurses: impact, facilitators and constraints. Available online at: https://www.kcl.ac.uk/content/1/c6/05/06/70/PreceptorshipReview.pdf (Accessed 4 July 2013) Royal College of Nursing (2013) Research and development by the RCN 2013-2016. Website. Available online at http://www.rcn.org.uk/development/researchanddevelopment/policy/rcn_randd_refresh/revie wing_knowledge (accessed 8 July 2013). Salas, E., Bowers, C. A. & Cannon-Bowers, J. A. (1995) Military team research: 10 years of progress. Military Psychology, 7, 55-75. 15 Salas, E., Burke, C. S., Bowers, C. A. & Wilson, K. A. (2001) Team training in the skies: does crew resource management (CRM) training work? Human Factors: The Journal of the Human Factors and Ergonomics Society, 43, 641-674. Salas, E. & Rosen, M. A. (2013) Building high reliability teams: progress and some reflections on teamwork training. BMJ quality & safety, 22, 369-373. Scott, T., Mannion, R., Marshall, M. & Davies, H. (2003) Does organisational culture influence health care performance? A review of the evidence. Journal of health services research & policy, 8, 105. Scrivener, R. & Watts, C. (2013c) Framing the fluid: mapping the systemic factors influencing professional nursing attitudes and behaviours. Evidence Live. Poster presentation. University of Oxford, UK; 25-26 March 2013. Sherrod, D., Roberts, D. & Little, B. (2008) Where have all the new grads gone? Nursing Management (USA), 39, 8-12. Thomas, L. & Galla, C. (2013) Building a culture of safety through team training and engagement. BMJ Quality and Safety, 22, 425-434. Törnkvist, L. & Hegefjärd, C. (2008) Evaluation of interprofessional training in home care. Journal of Interprofessional Care, 22, 509-520. Tyler, T. R. & Blader, S. L. (2003) The group engagement model: Procedural justice, social identity, and cooperative behavior. Personality and social psychology review, 7, 349-361. Weis, D., & Schank, M. J. (2002) Professional values: key to professional development. Journal of Professional Nursing, 18, 271-275. West, M. & Dawson, J. (2012) Employee engagement and NHS performance. The King’s Fund. Whitehead, B., Owen, P., Holmes, D., Beddingham, E., Simmons, M., Henshaw, L., Barton, M. & Walker, C. (2013) Supporting newly qualified nurses in the UK: A systematic literature review. Nurse education today. Willis Commission (2012) Quality with compassion: the future of nursing education. Report of the Willis Commission 2012. Available online at: http://www.williscommission.org.uk/__data/assets/pdf_file/0007/495115/Willis_commission_r eport_Jan_2013.pdf (accessed 10 July 2013). Wolf, L. E. (2007) A study of socialization of accelerated BSN graduates. Kent State University. Kent State University, Ohio. Zannini, L., Cattaneo, C. & Brugnolli, A. (2011) How do healthcare professionals perceive themselves after a mentoring programme? A qualitative study based on the reflective exercise of 'writing a letter to yourself'. Journal of Advanced Nursing, 67, 1800-1810. Zwarenstein, M., Goldman, J. & Reeves, S. (2009) Interprofessional collaboration: effects of practice-based interventions on professional practice and healthcare outcomes. Cochrane Database Syst Rev, 3. 16 APPENDIX 1: EPPI Centre report Professional socialization: Insights from reviews of organizational culture and performance. Mark Newman Catherine O’Keeffe June 2013 17 Abstract Four systematic reviews that investigated the conceptualization and measurement of organizational culture, the relationship between organizational culture and organizational performance and changing organizational culture were analyzed to identify insights relevant to the question of the relationship between organizational culture and professional socialization. The results of this review suggest that although the term occupational culture is widely used it remains a poorly specified concept with numerous distinct but overlapping definitions. Moreover it is unclear whether any of these conceptions are unique phenomena discrete from another organizational feature such as leadership or policy and procedures. This of course means that there is little if any consensus about how to ‘measure’ organizational culture. There does not appear to be research evidence to support the claim for a predictive causal relationship between organizational culture and organizational performance or evidence about how to change organizational cultures. Given these limitations the findings raise questions about the utility of framing considerations of perceived problems in professional socialization or performance in relation to organizational culture. It would certainly suggest that research based solutions are unlikely to be available. Introduction: Why the interest in organisational culture? Professional socialization refers to a process by which persons acquire the knowledge, skills and disposition that makes them more or less effective members (of a profession) and a subconscious process whereby persons internalize behavioural norms and standards and form a sense of identify and commitment to a professional field. (Mackintosh 2006) i.e they take on the normative values of the professional culture. The nature of this process and of professional cultures is a contested and dynamic field but given the inherently social nature of the process it is widely believed this socialization process is influenced by the culture of the organisations in which it takes place. For nurses in the UK this socialization process takes place in the wider society, in the NHS in which they learn and work and in the Higher Education Institutions in which they study. That organizational culture affects in some way professional socialization requires at least three conditions. That organisations in which professionals practice posses something called organisational culture that can be measured and enumerated in some way. That there is something called professionalism or professional culture that is or has the potential to be distinct in some way from organisational and wider social cultures; And that the process of becoming a professional requires or includes a process of socialization in to this professional culture. All of the reviews referred to in this paper note how organizational culture is widely considered to be one of the most significant factors in shaping how organizations function and bringing about organizational change. Arguably the specification of ‘NHS Values’ as ‘the common ground for co-operation to achieve shared aspirations, at all levels of the NHS’ (Department of Health 2013) can be viewed as a statement of or about NHS Organisational Culture. The concept has also permeated training for 18 healthcare professions in the UK, for example the NHS Education Outcomes Framework has as an outcome that all Healthcare staff in the NHS should adhere to ‘NHS Values and Behaviours’ (HEE 2013). Parmelli et al (2011) refer to a survey conducted by Mannion et al (2009) in 275 English National Health Service (NHS) organisations which highlighted that one-third of the organisations currently used a culture assessment instrument to support their clinical governance activity. Incidents of poor performance in healthcare delivery are also often attributed to problems with organisational and/or professional cultures as in the Francis reports which stated that ‘"The extent of failure of the system shown… suggests that a fundamental culture change is needed" (Francis 2013 p 8). The question of why the concept of organizational culture has come to be seen as so significant is not discussed in the reviews in any detail but each review highlights a number of different theoretical and practice roots for the idea. It maybe noteworthy that the growth of interest in the idea has coincided with the growing influence of organisation and management theory and practice in the public sector both in practice and in theoretical/ research terms. The acceptance of the idea of organisational culture has led to a practical need to explore, understand and change organizational cultures to achieve desired policy and practice outcomes and /or reduce undesirable outcomes. The work of this report This paper reports an interpretive review of four previously published systematic reviews each of which addresses questions about the relationship between aspects of organisational culture and aspects of organisational performance. None of these reviews used the terms ‘professional culture, professional socialization or indeed ‘organizational socialization’. However it is argued that that in taking ‘organisational culture’ as a central feature of analysis each review provides useful insights that can illuminate any consideration of the relationship between organisational culture and professional socialization. Jung et al (2009) reviewed existing research instruments for the exploration and measurement of organizational culture. The objectives of the review carried out by Parmelli et al (2011) were to determine the effectiveness of strategies to change organisational culture in improving healthcare performance and to examine the effectiveness of these strategies according to different patterns of organisational culture. The review by Scott et al (2003) asked the question does organisational culture influence healthcare performance. The review by Greenhalgh et al (2004) was concerned to address the issue of how to spread and sustain innovations in health service delivery. Each of the reviews addressed a slightly different question and/or took a different approach and therefore not every review contributed to all the content summarised in this paper. The authors of this paper read each review, and this paper is based on their interpretation of the useful messages from each review. 19 The characteristics of organisational culture All the reviews make the point that despite its intuitive appeal and widespread use by researchers, practitioners, and policy makers, there is little agreement as to how organisation culture should be conceptualized. Jung et al (2009) argue that within the literature well over 100 dimensions associated with organizational culture can be identified (see box 1 for a list of conceptions provided by Scott et al 2003 p 106). They further note that the typologies that have been developed differ in scope, number of items, and defining characteristics. They also note that the apparent under specification of the concept and lack of agreement on the basic tenets of the concept has not prevented the development of ever more complex models of culture replete with levels and specific recommendations for measuring and managing different aspects of organisational culture (see box 2 from Scott et al for an example of levels). The most simple definitions of organisational culture are a variant of ‘the way we do things around here’. More complex models are variants on the idea proposed by Schein: ‘the pattern of shared basic assumption – invented, discovered or developed by a given group as it learns to cope with its problems of external adaptation and internal integration – that has worked well enough to be considered valid and 20 therefore to be taught to new members as the correct way to perceive, think and feel in relationship to those problems’ (Schein 1985 cited by Scott et al 2003). This pertains to the multiple aspects of what is shared among people within the same organisation: for example beliefs, values, norms of behaviour, routines, traditions, sense making (Parmelli et al 2011). Scott et al (2003) add that this is not just about observable behaviours but also the shared cognitive and symbolic context within which an organisation can be understood. Parmelli et al (2011) suggest that culture is therefore a lens through which an organisation can be understood and interpreted by itself and by others. Jung et al (2009) argue that it is important to distinguish between organizational culture and organisational climate. They argue that although similar the two concepts are borrowed from different ‘domains’ and address different ‘levels’, with ‘culture’ being interpreted as a more encompassing and global concept (and presumably has a causal relationship to performance though they do not make this clear). ‘Climate’, with its meteorological roots and psychological thrust, can be perceived as an index rather than a causative factor in an organization’s operation. However, the significance of this distinction is not entirely clear through their review or the other reviews but may pertain to the practicalities of research that aims to measure ‘culture’ or climate in some ways. Greenhalgh et al (2004) sought to investigate the relationship between features of an organisation and the adoption of an innovation (which the review appeared to define as a positive feature). Of interest here are the characteristics they identify rather than the strength of any evidence for the claimed relationship. If we assume that the adoption of innovations is indicative of good organisational performance then the organisational characteristics associated with this may be relevant to considering professional socialization. Clear strategic vision, strong communication across departmental boundaries that communicates a shared and emergent organizational story about ‘what we are doing’, good managerial relations and visionary staff in pivotal positions were all highlighted as important factors. Some of the other characteristics they identified as positive influences may appear more problematic when viewed from the perspective of professional socialization for example ‘a climate conducive to risk taking and experimentation’ and ‘strong leadership that encourages members to break out of the convergent thinking and routines that are the norm’. It is not difficult to conceive how such characteristics could equally result in poor performance as well as good and/or may clash with professional cultures that emphasise the reduction of risk and evidence based practice. What is the relationship between organisational culture and organisational performance in health care? Scott et al (2004) point out the difficulties involved in researching the relationship between organisational culture and performance. They argue that previous reviews of empirical research, which claimed a causal relationship between the two phenomena, were methodologically flawed. They also point out that the negative or unintended consequences of organisational culture is rarely investigated or 21 discussed. They conclude therefore that the evidence base linking culture and performance in non health care organizations is suggestive but far from definitive. The Scott review included ten studies of the relationship between organizational culture and performance in ten Healthcare providers in different countries. The report of the review does not make clear how these particular studies were selected neither is there assessment of the quality of the individual studies. However the review authors describe their review as providing a description of the individual studies and discussion which they say provides a narrative about what organisational culture is, its relationship with performance and how performance is conceptualized and measured. So in essence they appear to be saying that the outcomes of the study are not of interest as such but more ‘what was studied’ and how. Nevertheless the authors do report that four studies found “some plausible evidence for a link between culture and performance, four found little evidence for such a link and two had unclear findings due to significant methodological issues” (Scott 2003 p108). The Scott review was sceptical about the claims made in the studies for a link between organisational culture and performance. However they did argue that one of the studies (carried out on management in Healthcare institutions in the USA) did provide convincing evidence that Healthcare organisations do differ in their dominant cultural orientation and that cultural orientation is associated with various aspects of performance. They conclude that this means that it is important to explore which aspects of performance will be valued in the dominant culture. In this respect they point to a theoretical model called the competing values framework which identifies four different categories of organisational type which they argue reflect different competing value positions on key aspects of organisation structure, value, and leadership type. The review authors claim that the competing values framework has ‘strong provenance’ in social and organisational theory. However it is not clear what ‘provenance’ means in this context and no further references or data are supplied to support this point. One of the studies included in the review was about Nursing Culture and performance in the USA. An analysis of nursing culture assessed 235 nursing department staff in 13 units as a precursor to changing their care delivery model. Nursing unit culture was measured by the Nursing Unit Cultural Assessment Tool. Performance was measured in terms of unit skill-mix, cost, worked hours per patient day, quality assurance, documentation of care planning and discharge, and patient satisfaction. The review authors were however not convinced of the quality of the study and did not therefore trust the study results Which interventions are effective in changing organisation culture? If organizational culture does influence professional socialization it is important to understand how we change organizational cultures to improve or support appropriate professional socialization. Parmelli et al (2011) sought to answer the question of which interventions are effective in changing organizational culture. The authors of this review argued that as the question that they were seeking to answer was causal 22 in nature the only studies that they would include in their review were those that could provide a valid evidence of a causal relationship. They therefore restricted their review to studies using experimental research designs. Only two studies were included in the review and the review authors argued that both of these studies were at a high risk of bias. The authors of the review therefore concluded that the evidence available at the time of the review did not identify any effective, generalisable strategies to change organisational culture How can we measure or explore organisational culture? If we wish to understand the relationship between organizational culture and professional socialization then we will need to be able to measure or explore organizational cultures in order to identify the similarities and differences between different organizational cultures in a valid and reliable fashion. Jung et al (2009) sought to review research instruments developed for this purpose. The review identified seventy instruments for exploring and assessing organizational culture. The authors point out that this number may not be definitive as it was not always clear whether some of the instruments identified were actually the same but just with a different name or different version. The authors appear to have taken a broad view of what counted as an instrument to measure organisational culture as the list of instruments includes titles such as ‘Critical Incident Technique’ and ‘Semiotics’ neither of which might immediately be associated with instruments to measure organizational culture. The list of instruments they identify includes five which appear to be focussed nursing cultures; the ‘Nurse Medication Questionnaire’; ‘Nurse SelfDescription Form’; ‘Nursing Unit Cultural Assessment Tool’; ‘Nursing Work Index/Nursing Work Index–Revised’ and the ‘Ward organizational features scale’ all of which they report have been subject to psycho-metric assessment. The instruments measure a myriad of items (see Box 3 below). However the majority focus on the tangible and intangible aspects that are assumed to correlate with individual and organizational performance. These include shared beliefs, emotions, internal and external environments, goals, identity, norms, practices, structures, values, and vision. A spectrum of data-generating methodologies were identified among the instruments, ranging from structured questionnaires to comparatively unstructured and emergent ethnographic approaches. The most common include Likert scales, Q-methodology, and ipsative measures. Although there had been psychometric assessment of 48 of the instruments (with 22 reporting adequate measures of internal consistency), there was little evidence of tests of validity in terms of relationships with other measures of culture i.e. although these instruments claim to measure something called organisational culture (or a particular aspect of it) there is little evidence to support that this is the case. There does not, seem to be a clear basis in the research evidence for making choices about which instruments to choose for any particular purpose. The review authors also caution that while insights from cultural assessment might be helpful, their inappropriate use could put an organization at a disadvantage. Cultural assessment could be a starting point to solve problems, but also could create problematic solutions 23 Box 3 Items in ‘organizational culture instruments (from Jung et al 2009) Discussion: Does organizational culture exist as a distinct entity from professional culture in ways that it is possible to specify, measure and manipulate ? The evidence reviewed in this paper raises doubts at least about all of the conditions required to demonstrate a relationship between organizational culture and professional socialization. An individual’s views, beliefs and behaviour shapes and is shaped by a wide range of factors. In the context of the workplace the idea that one of these factors is the values, beliefs and practices of other co-workers would appear to be a reasonable proposition. But is it reasonable to assume that these ‘collective’ values beliefs and practices constitute an ‘organisational culture’? This certainly seems to be the view of those who attribute differing levels of performance to differing organisational cultures. Similarly a question about the relationship between organizational culture and professional socialization presumes that there is a 24 phenomena called organizational culture that can be clearly distinguished from other aspects of organizational structures, roles, rules and performance. At the very least the reviews explored here raise questions about whether organisational culture is a distinct phenomena in its own right or whether it is in fact just a different label for something else such as ‘leadership’. This confusion also seems evident in claims about what needs to be done to improve organisational culture in situations where there has been poor performance. These tend to emphasise specific practices such as ‘improving communication’ or more nebulous ideas such having a ‘patient centred care approach’. Communication is a clear distinct set of practices in itself and is clearly affected by cultural practices but it is not in itself organisational ‘culture’. Similarly a patient centred care approach may imply a particular set of values or beliefs but is it organisational culture? Another assumption that appears to be embedded in the question of the relationship between organizational culture and professional socialization is that organizational culture and professional culture are somehow different or at the very least that organizational culture can potentially produce a less desirable or non normative professional culture. Quite aside from the issue of the contested nature of nursing professional culture, the discussion of what constitutes and measured as organizational culture (see boxes 1, 2, 3) seem to produce a model of the constituents of ‘culture’ which are very similar to what is described as the products of nursing socialization (see for example Mackintosh 2006). So organizational and professional cultures may in fact be the same thing. This does raise the question of whether a discrete focus on professional socialization is a useful way of trying to understand why particular organizations and the people in them do not always appear to act in the way that society and their professional peers might expect them to. Professional socialization’ could be viewed as a type of ‘performance’ outcome i.e that certain kind of organizational culture produce certain kinds of professional socialization that would seem to be the implication of the framing of the question. Professional socialization is not mentioned as an outcome in any of the reviews and it may not be appropriate to read such an interpretation across from for example the evidence about the adoption of innovations. Furthermore even if we accept that organisational culture exists as a distinct phenomena the direction of the relationship between ‘organisational culture’ and ‘organisational performance’ is unclear. The advocates of the importance of organisational culture suggest that organisational culture predicts performance i.e. that particular kinds of organisational culture produce better or worse performance. But the reviews argue that there is no evidence to support this claim and Scott et al (2003) argue in their review the two concepts emerge together in a reciprocal relationship. Similary Parmelli et al (2011) did not find evidence that organizational culture could successfully changed to produce different outcomes Each of the reviews discussed here found no strong evidence to support the claims made that organisational culture is related to performance, that we can successfully change organisational culture, or that we can measure organisational culture. It is important to recognise that absence of evidence is not evidence that organisational 25 culture is not related to performance, cannot be changed or measured. These reviews are of course based on a perspective that looked first to organizational culture and performance constructed in particular ways. Literature that looked first to professional or nurse socialization may provide a different illumination on the factors affecting professional socialization. If however it characterized these factors as ‘organizational culture’ the evidence reviewed here at least would suggest this was problematic. In this respect it would appear that rhetoric and an practice targeting ‘organizational cultures’ is running ahead of research on this particular issue. The question for practice is whether in any particular instance using the vocabulary and ideas linked to the concept of ’organisational culture’ is useful to help understand what may or may not be happening in an organisation and/or to make changes to how an organisation works with respect to professional socialization. In this respect Jung et al (2009) argue that organizational culture is just one of the many pieces that make up the puzzle of public sector organizations and as such, should not be considered the answer to all organizational problems, nor applied to all organizational issues. The framing of the issue as one of a relationship between organizational culture and professional socialization as in this case may not be productive for finding solutions. At least not solutions based on research evidence. Evidently more research is needed. Practitioners and policy makers should be aware that using these concepts may obscure certain kinds of problems in organisations and mask or distract attention from possibly effective solutions. References Department of Health (2013) The NHS Constitution London Department of Health Frances, R (2013) Report of the Mid Staffordshire NHS Foundation Trust Public Enquiry: Executive Summary London The Stationary Office Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O (2004) Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Quarterly. 82(4):581-629. Health Education England (2013) Introducing Health Education England: Our Strategic Intent Leeds/London Health Education England Jung T , Scott T , Davies HTO, Bower P, Whalley D, McNally R , Mannion R (2009) Instruments for Exploring Organizational Culture: A Review of the Literature. Public Administration Review pp1087-1096 Mackintosh C (2006) The socialisation of pre-registration student nurses: A longitudinal qualitative descriptive study. International Journal of Nursing Studies .pp 953-962 Mannion R, Koneth, FH, Davies HT (2009) Assessing organisational culture for quality safety improvement: a national survey of tools and tool use. Quality and Safety in Healthcare pp 153-156 18 (2) 26 Parmelli E, Flodgren G, Beyer F, Baillie N, Schaafsma ME, Eccles MP (2011) : The effectiveness of strategies to change organisational culture to improve healthcare performance: a systematic review. Implementation Science 6:33. Scott T, Mannion R, Marshall M, Davies HTO (2003) Does organisational culture influence health care performance? A review of the evidence Journal of Health Services Research & Policy Vol 8 No 2, 105–117 27 Appendix 2: SOCIAL LEARNING TOOLS: ARE WE ONLINE? Juan Carlos Rejon Research Analyst, RCN This appendix discusses findings from a narrative review of recent literature (2010 – present) addressing the emergence of social media as a learning tool. Learning, interaction, development and adaptation are present in formal forms of training delivery and in informal workplace learning integrated in the work stream. However, any dialogue about socialisation that did not the role of information technologies in the era of internet and social media would overlook a growing area of activity. The emergent use of social learning tools in the last decade is increasingly reaching professional fields such as nursing, meaning socialisation activities are taking place both in physical work places and also progressively more through online communication tools. An indicative example is the data presented by Chin (2013) in a discussion piece about the activity of the nursing community on Twitter. This shows a fivefold increase in nursing related tweets between 2011 and 2012, going from 3812 to 24231 tweets. Chin observes that not only were the number of tweets increasingly dramatically, they also demonstrated a tendency towards increasingly focused discussions. Hart (2011) describes the core uses applied to social media as: personal use, professional use, internal organisational use and external organisational use. The breadth of professional and organisational uses of social media identified by Hart is summarised in table 1 below. This multiplicity of uses suggests that a complementary approach to formal training is emerging, perhaps particularly in younger users accustomed to routine use of social media, and any consideration of contemporary socialisation processes of professional nursing need to be mindful of this. A product of this review has been the observation of an increasingly active socialisation of nurses through online media. Further exploration as to how enhancing informal social learning in the workplace and integrating social learning tools into the work stream for professional and organisational purposes would be beneficial for nurses and the organisations they work for. The breadth of online communication tools is striking, with a ‘Top 100 Social Learning Tools’ being released annually, thirteen of the top fourteen of which are free and many support cocreation of content (Hart, 2012). Tools might usefully be grouped by recognising the needs that they meet, such as: finding information; keeping up to date; building a trusted network of colleagues; communicating effectively with colleagues; sharing resources and ideas with colleagues; collaborating effectively with colleagues; improving personal and team productivity (Hart, 2011). A current example of the influence of social media tools such as Twitter on socialisation of nurses can be seen in the website Nurchat.co.uk, which facilitates bi-weekly discussions on nursing related topics using the #Nurchat hashtag. Most recently, and of resonance in the context of this review, a discussion about preceptorship considered nurse experiences and views around this issue (nurchat.co.uk, 2013), reaching some interesting consensus points around the importance of effective support and guidance. 28 Table 1: Professional and organisational uses of social media Professional use Internal organisational use External organisational use Keeping up to date with profession Keeping up to date with industry Communicating with existing clients/customers Professional networking Organisational networking and sharing Marketing & PR Professional development Customer service Team collaboration Job seeking Online recruitment Job/Team productivity Social training Source: “The Social Learning Handbook”. (Hart, 2011) This example highlights an essential difference of social technologies as compared with early web technologies. Web technologies are “read-only webs” with content created by an expert and published for users to read. Social technologies are “read-write” webs that provide users with a framework to co-create content, collaborate and share (Hart, 2011). The potential for large scale, co-created content to surface commonly agreed information is observed by Giles (2005) who compares traditionally authored Encyclopaedia Britannica and user-created Wikipedia. An example where the use of technologies can support design of strategies to mitigate negative aspects of socialisation of nurses can be found in the area of school nursing. School nursing has been recognised as a specialty of nursing in which the context of practice can involve some degree of professional isolation (Sortedahl, 2012). Barriers to the use of online tools for professional educational purposes in school nursing have been identified as: lack of time to find educational information; lack of knowledge about computers, technology, the Internet and specific programs; and lack of administrative support from school officials (Anderson and Enge, 2012). A promising use of online tools has been explored in building online journal clubs for nurses experiencing practice isolation, enabling them to connect with colleagues through online avenues (Sortedahl, 2012). This knowledge transition example in the context of school nursing provides an informative scenario where a problem has been identified (professional isolation), where the use of technologies with social learning purposes show promising results at building a network to connect professionals in the form of online communities of practice (journal clubs) that offer an arena for professionals with a common interest to interact. Networking and communicating with peers is a practice that frequently supports the activities of nurses (Ballard, 2011). Social media has been an integral part of many of our personal lives for some years and facilitates daily tasks like messaging friends, planning events, or following up on the latest activity and interests of those we connect with. This growth of social networking media has seen a movement into the professional field with the emergence professional social network, such as LinkedIn. Closer to the specific needs and requirements of the healthcare context is the creation of DocCom in 20073, a clinical social network for improving communication in hospitals. This 3 http://www.doccom.me/ 29 resource adapts features of social networks to meet safety requirements of patient data management, and provide added value in terms of efficiency and security of communications. The possible uses and examples presented suggest that the use of technologies as social learning tools in the professional arena and the co-creation of contents of all types is increasingly relevant, particularly within the context of professional socialisation throughout the nursing career. There is a clear role for professional bodies in fostering open discussions amongst members, experts and the public on relevant topics, or for the cocreation and monitoring of content. The social media adoption curve presented in figure 4 gives an indication of the phases involved in the process of familiarisation, adoption and use of social media for individuals and organisations. This figure allows individuals or organisations to identify current standing and visualise potential ways of profiting from a progression in adopting social media. Figure 1: Social media adoption curve Source: http://mixtmedia.wordpress.com/2008/11/12/social-media-adoption-curve/ References 30 Anderson, L., S. & Enge, K. (2012) Education and Information for Practicing School Nurses: Which Technology-Supported Resources Meet Their Needs? Journal of School Nursing, 28, 358-369. Ballard, J. (2011) OH professional practice, part 2: skills, decision-making, advice, information and professional development. Occupational Health [at Work], 8, 25-33. Chin, T. (2013) The Baseline. Professional website: Online Professional Community Development. Available online at: http://teresachinn.co.uk/the-baseline/ (accessed 9 July 2013). Giles, J. (2005) Internet encyclopaedias go head to head. Nature, 438, 900-901. Hart (2011) Social Learning Handbook. Hart (2012) Top 100 tools for learning 2012. Website: Centre for Learning and Performance Technologies. Available online at http://c4lpt.co.uk/top100tools/ (accessed 9 July 2013). Nurchat.co.uk (2013) Preceptorship: the way it should be? Website. Avialable online at: http://www.nurchat.co.uk/index.php/2013/06/04/nurchat-11062013-preceptorship-the-way-itshould-be/ (accessed 9 July 2013). Sortedahl, C. (2012) Effect of Online Journal Club on Evidence-Based Practice Knowledge, Intent, and Utilization in School Nurses. Worldviews on Evidence-Based Nursing, 9, 117125. 31