Septic Shock
advertisement

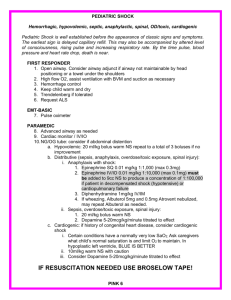
SHOCK September 6, 2005 Andrew Filiatraut In General Shock Clinical syndrome defined as hypoperfusion Hypotension and Cellular Hypoxia Elevated lactate Oliguria Hepatic/GI dysfunction Mental status changes In General Four Classifications Hypovolemic Cardiogenic Obstructive Distributive Septic, Addison’s, Anaphylactic, Neurogenic, Thyrotoxicosis, Beriberi, Paget’s, Cirrhosis, Chroinc Anemia, Osler-Weber-Rendu Hemodynamic Profiles TYPE BP C.O. PCWP SVR ↓ Vol. ↓ ↓ ↓ ↑ Cardio ↓ ↓ ↑ ↑ Tmpnad ↓ or N ↓ or N ↑ or N ↑ P. E. ↓ ↓ ↓ or N ↑ Distrib ↓ ↑ ↓ ↓ Septic Shock Epidemiology 751,000 cases of severe sepsis /year Up to half develop shock Overall mortality rate of 45% Cause Gram+ 35-40% Gram- 55-60% Slightly higher incidence in men, older adults (55-60 yrs) Definitions Infection Inflammation against microorganism Bacteremia Viable bacteria in blood Definitions SIRS Evidence of inflammation NOT necessarily infection 2 or more of the following Temp>38 or <36 HR >90bpm RR >20 or PaCo2 <32 WBC’s >12,000 or <4000 or >10% bandemia Definitions Sepsis systemic inflammatory response as a result of infection Severe Sepsis sepsis associated with organ dysfunction Lactic acidosis, oliguria, mental status change Septic shock sepsis-induced hypotension with presence of perfusion abnormalities Definitions Sepsis-induced hypotension SBP<90 or reduction of 40mm Hg from baseline without other cause Multiple Organ Dysfunction Syndrome Altered organ dysfunction in acutely ill patient requiring intervention to maintain homeostasis Pathophysiology Pathophysiology Focus of infection Pneumonia, UTI, cellulitits, abscess, indwelling device ICU: catheters, sinusitis, acalculus cholecystitis, C. diff, resistant organism, fungal infection Blood stream invasion or proliferation of organism at site Exogenous toxin release Activation of endogenous mediators Molecular Mediators in Pathophysiology Three phases Induction Cytokine synthesis & secretion Cascade Molecular Mediators in Pathophysiology Induction Interaction of microbial molecules with host Mediators activated that amplify & transmit the microbial signal to other cells Ex LPS binds to LPS binding protein which is detected by CD14 releasing TNF-alpha Peptidoglycan & lipoteichoic acid of gram (+) induce similarly Molecular Mediators in Pathophys Cytokine cascade Activation & release of central mediators Release of secondary mediators TNF-alpha and IL-1 IL-6, IL-8, PAF, PG’s, leukotrienes Activation of neutrophils, complement system, vascular endothelial cells Synthesis of acute phase reactants Molecular Mediators in Pathophys Parallel to SIRS is CARS Compensatory Anti-inflammatory Response System Attempts to down regulate the SIRS response IL-4, IL-10, transforming growth factor beta, CSF, soluble receptors to TNF, antagonists to TNF-alpha and IL-1 If CARS reaction is severe it will manifest as anergy and infection susceptibility Vasoactive Mediators in Pathophys Nitric Oxide Produced by endothelium Increased levels during shock Actions at high levels Mediator of vasodilation & hypotension Direct cellular toxicity Myocardial depression Increased permeability Clinical Features Clinical Features Constitutional Hyper/hypothermia Tachycardia Tachypnea Wide pulse pressure Mental status change Most likely obtunded Clinical Features Cadiovascular Early, vasodilators predominate Cardiac output is increased with tachycardia CO=SV x HR i.e. Initially patients will have warm extremities If not treated aggressively decompensation ensues Typically hypotension is not reversible with fluids alone Clinical Features Pulmonary Sepsis is most common condition associated with ARDS Lung edema from increased permeability Alveolar edema dyspnea, hypoxemia, opacities on CXR B/L infiltrates, wedge pressure <18 Endotoxin, TNF-alpha, IL-1, IL-6, IL-8, bactericidal/permeability-increasing (BPI) protein Clinical Features Pulmonary ARDS B/L pulmonary infiltrates PCWP <18 (non-cardiogenic pulm edema) PaO2/FiO2 <200 If PaO2/FiO2 >200, but <300 then ALI Clinical Features Renal Acute renal failure w/ azotemia, oliguria, active urinary sediment Hypotension/Dehydration, aminoglycosides, pigmenturia (e.g. myoglobinuria) Immune complex deposition IgG, IgM,C3, bacterial antigens & antibodies Tubulointersitial disease S. pneumoniae, S. pyogenes, Legionella, salmonellosis, brucellosis, diptheria Clinical Features Gastrointestinal Accelerated apoptosis of GI epithelial cells Can lead to blood loss anemia Cholestatic jaundice (most frequent abnormality) Transaminase/Alkaline phosphatase 1-3x normal Bilirubin concentrations, usually not >10mg/dL Hemolysis of RBC’s, hepatocellular dysfunction due to endotoxin Clinical Features Hematologic Minor blood loss secondary to erosions in mucosal layer of stomach/duodenum Accelerated apoptosis of lymphocytes Possibly due to elevated glucocorticoids Most frequent changes are neutrophilia or neutropenia, thrombocytopenia, DIC Clinical Features Hematologic Neutrophilia Most common Left shift Demargination & release of less mature granulocytes from BM C3a causes release of neutrophil releasing substance Sustained neutrophilia is secondary to CSFs Clinical Features Hematologic continued Neutropenia Morphological changes of WBC’s in sepsis Increases mortality Increased peripheral use of cells, damage to cells by bacterial byproducts, depression of marrow by inflammatory mediators Toxic granulations, Dohle bodies, vacuolization Functional changes of WBC’s Increased phagocytic/cytotoxic activities Clinical Features Hematologic continued RBC production & survival are decreased Usually does not cause anemia unless infection is prolonged Low serum Fe concentrations Decrease by 50% Influx into liver & other reticuloendothelial cells Clinical Features Hematologic continued Thrombocytopenia Usual a consequence of DIC May be early sign of bacteremia Inhibition of thrombopoiesis, increased platelet turnover, increased endothelial adherence, increased destruction Clinical Features DIC Clotting & fibrinolytic systems activated Consumption of coagulation factors & platelets Clotting system activated through the extrinisic clotting system by bacteria, viruses, fungi, endo/exotoxins Gram(-) precipitate DIC more readily than gram (+) Fibrinolytic system is activated by tissue type plasminogen activator As sepsis progresses, increase release of plasminogen activator inhibitor type 1 Clinical Features DIC continued Two forms Compensated “slower” generalized activation Bleeding prevented by increasing coagulation factor production in liver, release of platelets from reserve, synthesis of inhibitors at accelerated rate Decompensated Clinical bleeding and/or thrombosis Thrombocytopenia, prolonged PT/PTT, decreased fibrinogen & antithrombin III, increased fibrin monomer/fibrin split products/D-dimer Clinical Features Endocrine Hyperglycemia Increased catecholamines, cortisol, glucagon, peripheral insulin resistance, impaired glucose use, decreased insulin secretion Significant risk for adverse outcome Must maintain tight control w/insulin infusion to keep b/w 80100 mg/dl (NEJM Nov 8, 2001; vol 345, #19) Hypoglycemia Assoc. w/S. pneumoniae, S. aureus, S. pyogenes, Listeria, Neisseria meningitidis, H. flu, Enterobacteriaceae Clinical Features Acid/Base Early in sepsis resp alkalosis Metabolic acidosis suggests inadequate perfusion, impaired hepatic clearance of lactate/pyruvate, increased glycolysis Hypoxemia often present due to vent/perfusion mismatch Clinical Features Cutaneous Direct bacterial involvement Lesions as a consequence of sepsis/hypotension/DIC Cellulitis, erysipelas, fasciitis Acrocyanosis & necrosis of peripheral tissue Lesions secondary to intravascular infection Microemboli &/or immune complex vasculitis Diagnosis Diagnosis Pt presents with Hypotension not responsive to fluid bolus Inadequate perfusion Complaints attributable to a serious infection Hot flushed skin Mental obtundation or agitation Widened pulse pressure Hyperventilation Dysthermia **beware of the old, young, immunocompromised Diagnosis Differential Diagnosis Other causes of shock Cardiogenic Neurogenic Hypovolemic Anaphylactic Obstructive (PE, tamponade) Endocrine (adrenal insufficiency, thyroid storm) Diagnosis H&P Basic lab and x-rays are usually successful in identification of source CNS Meningitis (nuchal rigidity, MS change, petechiae) Brain abscess, sub/epi dural empyemas Viral CNS infections Diagnosis Pulmonary Intra-abdominal processes Acute bacterial pneumonia Most common source of infection leading to sepsis Acute pancreatits Cholangitis Septic abortion/endometritis/myometritis Pyelonephritis Occult Abscess Skin Cellulitis (S.aureus, S.pyogenes) Decubitus ulcer(s) Diagnosis No obvious source Endocarditis Primary bacteremia S.aureus, S.pneumoniae, N.meningitidis Asplenia Salmonella, H flu, S pneumo, N. meningitidis IVD users, Pseudomonas & gram(-) bacteria Skin abscess from “popping” Diagnosis Ancillary Studies CBC DIC panel (PT,PTT,fibrinogen,D-dimer, ATIII) CMP (include Mag, Ca, Phosphate) Lactate level ABG UA CXR Cultures (blood, urine) If H&P suggest LP, CT (abd . . .) Consider CRP, pro-calcitonin, IL-6 level Standard Treatment Standard Treatment ABC’s! Maintain O2 sat’s above 90% Hemodynamic Stabilization Rapid fluid administration Rate of 0.5L of NS every 5-10min May require 2-6L in initial stabilization phase Be careful with heart failure patients Monitor response with BP, HR, RR, mental status, urine output (1cc/kg/hr), CVP, skin perfusion Standard Treatment ▪ Inotropic support If no response to fluids or signs of fluid overload present Goal is to keep MAP above 65 mm Hg Dopamine 5-20 micrograms/kg/min Beta-1, dopaminergic and alpha adrenergic activity Norepinephrine Beta-1 and alpha adrenergic stimulation Short term vasopressin infusion (0.04 units/min for 416h) Vasodilatory septic shock Standard Treatment End points Early goal directed therapy provides significant benefit & improves outcome Rivers et al. NEJM vol. 345:1368, 2001 Maintain CVP b/w 8-12 Hct 30% SVO2 >70% Reduction in mortality from 44% in control group to 29% in intervention group Standard Treatment Empiric Antimicrobial Therapy Start ASAP Try to get culture samples before Select based on adequate coverage of potential pathogens Should cover gram +/Give maximum dose allowed Give IV Empiric Antibiotics in Sepsis Table 32-3 Standard Treatment Removal of Source of Infection Indwelling catheters send tip for culture Replace Foley catheters Intra-abdominal or soft tissue sites of pus require urgent drainage Standard Treatment Initial Baseline Assessment & Continued Monitoring (again goal directed) Some use serum lactate to monitor response ABG’s to monitor ventilation & perfusion 2 large bore IV’s Consider central line early If requiring vasoactive drugs consider pulm artery thermal-dilution catheter Other monitoring gadgets Sublingual capnography, gastric pH tonometry, muscle oximetry, bioimpedance determination of CO New Innovative Therapies Innovative Therapy Based in premise that neutralizing bacterial toxins, cytokines, & other mediators could stop or slow the syndrome Innovative Therapies Corticosteroids Meta-analysis has shown physiologic doses of hydrocortisone improves outcomes (200-300mg/d) for 5-7 days Then tapered for 5-7 days Early studies (proir to 1989) used high doses and had increased mortality Those published after 1997 (5)used lower doses and reported improved survival similar to that of Activated Protein C Annal of Internal Med 2004;141:47-56 Innovative Therapy Activated Protein C (Xigris) Inactivates Factors Va and VIIIa Inhibits thrombin (decreases inflammation) Inhibits platelet activation, neutrophil recruitment, and mast cell degranulation Blocks cytokine production Inhibits cell adhesion Anti-apoptotic actions Apoptosis (i.e. GI epithelial cell) induces anergy Innovative Therapy Summary To date the only treatments shown to produce benefit Early goal directed hemodynamic stabilization Tight control of blood glucose with insulin Activated protein C “Efficacy and Safety of Recombinant Human Activated Protein C for Severe Sepsis” NEJM 2001, vol. 344; 699-709 Cardiogenic Shock Cardiogenic Shock A state of decreased cardiac output(CO) producing inadequate tissue perfusion despite adequate or excessive circulating volume Cardiogenic shock Etiology AMI Depression of contractility Sepsis, myocarditis, contusion Mechanical obstruction Pump failure (40% of LV involved) Mechanical complications (MR,VSD,free wall rupture) RV infarction AS, hypertrophic CM, MS, LA myxoma Regurgitation of LV output AI, chordal rupture Pathophysiology AMI cell death loss of contractile function Decreased CO/SV tachycardia/hypotension decreased coronary perfusion/diastolic filling time Further ischemia SNS/Renin-Angiotension System activation Increased SVR and myocardial O2 consumption Cardiogenic Shock Clinical Features PE Hypoperfusion +/-hypotension (SBP<90) Skin mottling, obtunded May be compensated (pulse pressure <20, ST) or pre-existing hypertension Tachypnea, rales (clear if RV), JVD Murmur MR (chordae tendinea rupture): holosystolic at apex going to axilla VSD: holosystolic at L parasternal Cardiogenic Shock Ancillary Studies ECG: ischemia/infarction,electrolyte abnormality,drug toxicity CXR: helps r/o other causes (pneumonia, aortic dissection, pericardial effusion) Labs: BNP, cardiac enzymes, ABG, lactate, electrolytes, serum drug levels Echo: ventricular/valve dysfunction HD monitoring (table 33-3): invasive vs bioimpedance Cardiogenic Shock Differential Diagnosis AMI PE COPD Pneumonia Aortic dissection Tamponade Acute valvular insufficiency Hemorrhage Sepsis Drug OD of negative inotropic/chronotropic agent Cardiogenic Shock Treatment ABC’s first IV access/cardiac monitor/art line/foley Correct hypoxia/hypovolemia/rhythm disturbance/electrolyte abnormalities/acid-base alterations Hypotension Dopamine,dobutamine Fluid bolus if RV involved Acute MR consider dobutamine and nitroprusside IABP Cardiogenic Shock Treatment continued Thrombolytic therapy Intraaortic balloon conterpulsion Better outcomes if followed by revascularization Decreases afterload, increases diastolic BP Early revascularization Most important life saving intervention Cardiogenic Shock Treatment continued Inotropic agents Dopamine Dobutamine Use for signs of poor perfusion when SBP>90 2-20micrograms/kg/min Norepinephrine First line agent 2.5-5 micrograms/kg/min beta-1 5-10 alpha & beta-1 10-20 alpha Use only when inadequate response to other pressors 2 micrograms/min and titrate to response Milrinone 50 microgram/kg bolus followed by 0.5microgram/kg/min infusion—watch BP! Anaphylactic Shock Anaphylactic Shock Severe systemic hypersensitivity with multisystem involvement Life-threatening release of mediators by mast cells and basophils Anaphylactic Shock Pathophysiology 4 classic mechanisms 1. cross-linking of 2 IgE molecules on a mast cell or basophil by a multivalent antigen 2. reaction of IgM & IgG to cell surface antigens 3. soluble antigen-antibody complexes activating complement 4. activation of T lymphocytes Anaphylactic Shock Pathophysiology Classic anaphylaxis 2 separate exposures First the antigen or hapten-protein complex is processed by macrophage & dendritic cells Presented externally with MHC-2 T helper cells recognize and stimulate plasma cells to produce IgE Second exposure recognized by these IgE antibodies triggers degranulation of mast cells and basophils Anaphylactic Shock Pathophysiology Complement mediated reaction Occur after administration of blood products secondary to immune complexes C3a & C5a cause degranulation Non-immunologic anaphylaxis (anaphylactoid) Exogenous substances directly degranulate mast cells Radiocontrast dye, opiates, depolarinzing drugs, dextrans Anaphylactic Shock Pathophysiology ASA/NSAIDS Non-mast cell process Modulate cyclooxygenase-arachidonic acid metabolism Idiopathic anaphylaxis Diagnosis of exclusion Anaphylactic Shock Clinical Features Diffuse urticaria & angioedema +/- abd pain or cramping, N/V, diarrhea, bronchospasm, rhinorrhea, conjunctivitis, dysrhythmias, hypotension c/o “lump” in the throat heralds life-threatening laryngeal edema Usually begin w/in 60 minutes of exposure Faster the onset the more severe the reaction Biphasic phenomenon Second release of mediators clinically evident 3-4h after the initial manifestations clear Anaphylactic Shock Diagnosis History and physical 2 or more body systems involved Differential Vasovagal reaction, status asthmaticus, seizure, epiglottitis, hereditary angioedema, FB airway obstruction, carcinoid, mastocytosis, non-IgE drug reactions, AMI, dysrhythmias Anaphylactic Shock Treatment First Line ABC’s Epinephrine, oxygen, fluids (NS 1-2L) Epi 0.1mg in 10cc NS over 5-10minutes IV if signs of CV collapse If refractive start infusion: 1mg in 500ccD5W at 1-4 micrograms/min Less severe, give 0.3-0.5 mg IM in the thigh decontamination Anaphylactic Shock Treatment Second Line Corticosteroids Methylprednisolone 125mg IV 2mg/kg in children Antihistamines Diphenhydramine (H1) 25-50mg IV Ranitidine or cimetidine(H2) Avoid cimetidine in elderly, renal/hepatic failure, or if patient is on beta blocker Anaphylactic Shock Treatment Second Line Agents for bronchospasm Albuterol Ipratropium bromide Magnesium 2g IV over 20-30minutes 25-50mg/kg in children Glucagon 1 mg IV q 5min until response followed by infusion 5-15 micrograms/min if patient on beta blockers with refractive hypotension Anaphylactic Shock Disposition Unstable patients admit to ICU If patient received epi-observe for 4h Consider distance from care, someone to go home with, comorbidities, age Good discharge instructions is a must Send with epipen, short course of antihistamines and steroids Neurogenic Shock Neurogenic Shock Acute spinal cord injury Disruption of sympathetic outflow Hypotension & bradycardia Majority caused by blunt trauma MVA, falls, sports Cervical region most commonly injured Penetrating injury (10-15% of cases) GSW’s and stab wounds Neurogenic Shock Pathophysiology 33 bony vertebrae Anterior body, posterior arch, sup/inf articular processes, pedicles, laminae Spinal cord is cylindrical arising from base of brain & covered by 3 layers of meninges & CSF 31 pairs of spinal nerves exit the canal via intervertebral foramen Spinal nerves are formed by ant/post nerve roots Neurogenic Shock Pathophysiology Spinal cord contains white & gray matter White: nerve fibers running up & down in cord tracts Gray: nerve cells Autonomic Nervous System Sympathetic Outflow tracts in lateral gray horns of 1st thoracic to 2nd lumbar Controlled by hypothalamus Lateral hornanterior nerve rootganglia of paraspinal sympathetic trunktravel throughout the body Neurogenic Shock Pathophysiology Autonomic Nervous System Parasympathetic Cranial Nerves & 2-4th sacral segments (splanchnic nerves) Neurogenic Shock Clinical features Hypotensive with warm,dry skin Bradycardic ususally Hypothermic These symptoms last 1-3 weeks Neurogenic Shock Treatment ABCDE’s Investigate all other possible sources of hypotension & bradycardia Infuse crystalloids rapidly Attempt to keep MAP 85-90mm Hg for the first 7 days to minimize secondary cord injury Dopamine & dobutamine may be helpful Severe bradycardia can be treated with atropine or pacing Steroids are not indicated in the treatment of neurogenic shock per se Indicated in blunt injury with neuro deficits if started within 8h (30mg/kg bolus then 45 mins later infuse at 5.4mg/kg/h for 23h) Questions 1. In cardiogenic shock the PCWP is A. Decreased B. Increased C. Normal Questions 2. SIRS is defined as inflammation secondary to infection A. True B. False 3. Which is not a parameter used to define ARDS A. Bilateral infiltrates on CXR B. PCWP>18 C. PaO2/FIO2 <200 4. What is considered the first line inotrope in cardiogenic shock A. Dopamine B. Dobutamine C. Milrinone 5. Which is not considered a first line agent in treatment of anaphylaxis A. Epi B. Oxygen C. albuterol Answers 1. 2. 3. 4. 5. B B B A C