SHOCK2
advertisement
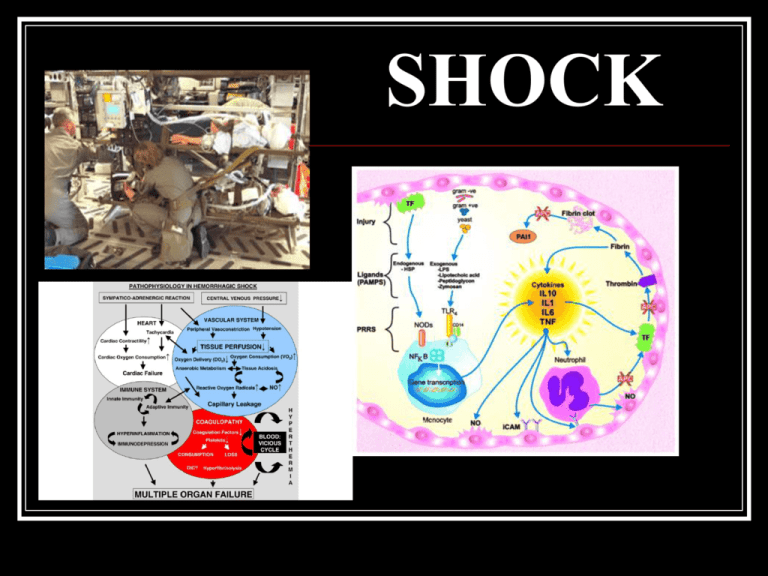
SHOCK History First used as a term to denote physiologic instability in 1815 by then English surgeon, George James Guthrie Before then a variety of more colorful terms were used to denote shock states: “final sinking of vitality” “great nervous depression” “sudden vital depression” Modern Working Definition The reduction of effective tissue perfusion leading first to reversible, then to irreversible cellular injury Traditionally catagorized Hypovolemic Cardiogenic Vasogenic (Distributive) Obstructive Alternatively….. Failure of Cardiac Output Failure of Peripheral Resistance ???? This is the time for audience participation.....WAKE UP CO = ____ x ____ 6 CO = SV x HR 7 Failure of Cardiac Output Heart Rate Too slow Too fast No flexibility to adjust to need Stroke Volume Failure to receive Hypovolemia MS Tampannade Failure to eject CHF PE Outflow obstruction Ohm’s Law of the Heart??? again, this is YOUR turn to talk.. MAP = ___ X ___ 9 MAP = CO x SVR systemic vascular resistance 10 Failure of Peripheral Resistance Anaphylaxis Sepsis Loss of vasomotor tone Spinal Shock Vasodilatory Shock 12 SO……practically speaking how does this help you care for patients? You are called to the ED at the Valley. There is a 2 year old, hit by a car. His VS: 66/48 180 28 92% (on oxygen) You are IT. The trauma team is busy with is mother who is in full arrest. The PICU attending is 30 minutes away. What do you do??? There was no LOC. He is moaning and localizing to painful stimuli. There is a noticeable tire mark across his pelvis which is unstable on exam. 14 The Proxy Measure Blood Pressure Ohm’s Law: V=IR (MAP=CO x SVR) Measureable since the early 1900’s Hypotension is late for most patients Still..it is the proxy measure Interventions ABC’s Volume Salt More salt Colloid Albumin or Starch Vasoactive medications Diagnostic Labs Volume Saline Ringers Albumin Starch solutions Hypertonic salt How much?? When to say when Positive fluid balance infers or confers morbidity Vasoactive Medications Which one? How much? When to say when or when to say ECMO? Dopamine..Why? Why not?? Vasopressin.. Why?? Why not?? The other interventions Central Access? Arterial Access? Antibiotics? Corticosteroids? Blood products? In parallel to exogenous support....the response of the body Catacholamine release Vasopressin surge Aldosterone and ADH defend intravascular volume Corticosteroid levels rise Insulin in suppressed, GH increases 20 And yet, even when we execute the perfect resuscitation and the body defends itself without limit, the irreversible nature of the initial insult often prevails. The patient develops MODS (MSOF) and dies.... 21 What is on the horizon? 23 The Aquatic Turtle? Has the capacity to downregulate metabolic pathways during hypoxia and upregulate that activity when O2 is available... 24 Inducing hypoxia tolerance 25 Closer to the bedside 27 Hydrogen Sulfide Third gaseous transmitter (NO, CO) Dose dependent pro or anti-inflammatory Dose dependent pro or anti-apoptotic **Inhibits cytochrome c oxidase Protects animals from MODS after hemorrhagic shock and profound hypoxemia Matches supply and demand October 10, 2006 | 1 comments Sewer Gas Sends Mice into Suspended Animation By David Biello Suspended animation may be closer than we think….. Sodium sulfide is in phase One trials NOW 29 30