ACC / AHA Guidelines for the Management of Patients with Unstable
advertisement

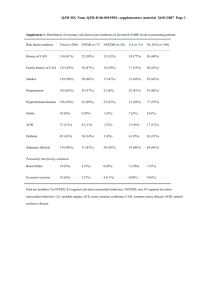
Acute Coronary Syndromes Jason Ryan, M.D. Acute Coronary Syndromes Unstable Angina + Non-ST-Elevation MI + ST-Elevation MI Acute Coronary Syndromes (ACS) UA + NSTEMI (life-threating but not medical emergency) STEMI (medical emergency) Acute Coronary Syndromes Generally, same symptoms for all – Squeezing, pressure-like, substernal chest pain – Often associated with shortness of breath and diaphoresis – Pearl: If nausea and vomitting think inferior wall MI – With UA/NSTEMI, often preceding history of exertional symptoms Remember the DDx for Chest Pain ACS Aortic Dissection Pulmonary Embolism Acute choleycystitis Pericarditis Costocondritis Esophogeal spasm Many others The Can’t Misses ST-Elevation MI ST-Elevation MI ST-Elevation MI ST-Elevation MI Coronary Stenosis: Progression to STEMI Serial Angiogrpahy in 239 Patients Stenosis Pre-MI 0% 25% 50% 75% 90-99% Nobuyoshi M et al., JACC 1991;18:904-10 Culprit For MI 8 10 29 5 6 10 39 ST-Elevation MI If you suspect STEMI: – OMI: Oxygen, monitor, IV access – ABC: Ensure patient is stable – Call cardiology – Pre-cath medication: Aspirin 325mg PO Lopressor 25mg PO (if BP and Pulse will tolerate) – Beware cardiogenic shock Heprin 5000U bolus (if no active bleeding issues) Discuss IIB/IIIA and Clopidogrel with cardiology Unstable Angina (UA) and Non ST Elevation Myocardial Infarction (NSTEMI) • 5,315,000 annual ER presentations for chest pain • 1,433,000 annual U.S. hospital admissions for UA/NSTEMI • 50 patients per month at BIDMC coded as: AMI, SUBENDOCARDIAL ISCHEMIA UA and NSTEMI Placebo Event Rates in Recent Trials of UA and NSTEMI Death/MI at 30 days PRISM1 7.1% PRISM-PLUS2 11.9% PURSUIT3 15.7% GUSTO-IV ACS4 PARAGON A5 1. PRISM Study Investigators. N Engl J Med 1998;338:1498-1505. 2. PRISM-PLUS Study Investigators. N Engl J Med 1998;338:1488-1497. 3. Harrington RA. Am J Cardiol 1997;80:34B-38B. 4. The GUSTO IV-ACS Investigators. Lancet 2001;357:1915-1924. 5. The PARGON Investigators. Circulation 1998;97:2386-2395. 8.0% 11.7% UA and NSTEMI Definitions – Unstable angina New onset angina Angina that occurs at rest Angina that occurs with accelerating frequency (crescendo angina) May have EKG changes (ST depression) Biomarkers will be negative UA and NSTEMI Definitions – NSTEMI Typical rise and fall of cardiac biomarkers plus at least one of the following: – – – – Anginal chest pain Ischemic EKG changes (ST-depression) Development of Q waves on EKG Coronary intervention Often can’t tell UA from NSTEMI at presentation Joint European Society of Cardiology/American College of Cardiology committee NSTEMI The Biomarkers: – CK Rises 4-6 hours after MI Peaks and falls by 36-48 hours after MI Total CK is non-specific CK-MB is more specific for cardiac tissue – (but there is still some in skeletal muscle!!) – Remember this is one component in the diagnosis of NSTEMI – CK alone cannot be used to diagnose NSTEMI NSTEMI The Biomarkers: – Troponin Rises 4-6 hours after MI Can remain elevated for up to two weeks! Very specific for cardiac damage Elevated in many other conditions than ACS – – – – Hypotension of any cause (~80% patients) Renal failure Congestive heart failure Many others Always predicts worse outcomes NSTEMI Four pieces to NSTEMI: – Symptoms – EKG changes – CK – Troponin ACC Guidelines for Management of UA/NSTEMI Chest Pain EKG No ST Possible UA/NSTEMI MSO4 NTG ASA Beta Blockers Definite/Likely UA/NSTEMI MSO4 NTG ASA Beta Blockers Heparin Plavix ST Follow ST Protocols Definite/Likely UA/NSTEMI with cath or PCI planned MSO4 NTG ASA Beta Blockers Heparin Plavix IIB/IIIA Inhibitor American College of Cardiology (ACC) 2002 Guidelines for UA/NSTEMI Medications with Class I indication First 24 hours •Morphine •Nitroglycerin •Aspirin •Beta Blocker •Plavix •Heparin •IIB/IIIA Inhibitors Discharge •Aspirin •Beta Blocker •Plavix •ACE Inhibitor •Statin ACC 2002 Guidelines for UA/NSTEMI How well do we do? 100% NRMI-4 NSTE MI Acute Care: 3rd Quarter 2001 85% 80% 71% 72% 60% 40% 24% 20% 0% ASA Beta Blocker Heparin (all) GP IIb/IIIa ACC 2002 Guidelines for UA/NSTEMI How well do we do? NRMI-4 NSTE MI Discharge Care: 3rd Quarter 2001 100% 84% 75% 80% 71% 56% 60% 40% 21% 20% 0% ASA Beta Blocker * LVEF < 40% # Known hyperlipidemia ACE Inhibitor * Statins # Cardiac Rehab ACC 2002 Guidelines for UA/NSTEMI How well do we do? Gap between ‘Leading and Lagging’ US Hospitals Performance Quality Indicator ASA use < 24 h blocker use < 24 h Heparin use <24 h GP IIb-IIIa < 24 h D/C ASA use D/C blocker use D/C ACE-I use D/C lipid lowering Bottom 10% 54% 33% 50% 0% 54% 44% 21% 33% Top 10% 99% 98% 92% 51% 99% 96% 83% 99% ACC 2002 Guidelines for UA/NSTEMI Does doing well matter? Benefits of Using Evidence-Based Therapies (Non-ST ACS Patients from GUSTO IIb) Additional Lives Discharge Saved per 1,000 Therapy Current Use (ideal use) Aspirin 86% 9 Beta blockers 59% 11 ACE inhibitors 52% 23 Alexander K, JACC, 1998 Case 1 A 54 year old man with DM, HTN, and high cholesterol presents to the ER complaining of substernal chest pain. The pain feels like his chest is being squeezed. He first noted it two months ago when carrying packages up a flight of stairs. Last week he noticed it when walking to work. The past two days, the pain has occurred whenever he climbs the stairs in his house. This morning it occurred while driving to work. His initial EKG shows sinus tachycardia with anterior ST depressions. His initial cardiac biomarkers are negative. He becomes pain free during his first few minutes in the ER and his EKG changes resolve. Case 1 Is this an ACS? – YES!!! How should this patient be managed? – Morphine and NTG to make him pain free – Aspirin, Beta blocker, Heparin, Integrillin – Plan for catheterization with 24-48 hours Case 2 A 75 yom with HTN presents to the ER complaining of squeezing, substernal chest pain. The pain began this morning while taking a shower and has waxed and waned all day (~10 hours time). Initial EKG shows sinus tachycardia without ST changes Initial biomarkers: – CK 300, MB 20, Trop T 0.5 Case 2 Is this an ACS? – YES!!! How should this patient be managed? – Morphine and NTG to make him pain free – Aspirin, Beta blocker, Heparin, Integrillin – Plan for catheterization within 24-48 hours Case 3 A 82 yof is transferred to the ED from her nursing home where she was noted to be lethargic. For the past two days, she has had decreased POs and one episode of vomiting. The patient is unable to give a history. On initial ED eval, her blood pressure is 72/45 and her temp is 101.4 Initial EKG shows sinus tachycardia Initial biomarkers show CK 110, MB 6, Trop 0.5 Case 3 In this an ACS? – Unlikely How should this patient be managed – ASA if no contraindication – No BB given hypotension – No heparin or IIB/IIIA as this is not likely ACS – Work up fever and hypotension – Cycle biomarkers – Repeat EKG in 6-12 hours Case 4 A 62 yom with a history of ESRD on HD, Ischemic CM with EF 20% presents with lethargy and altered mental status for two days Initial vitals are remarkable for a room air O2 sat of 88% EKG shows sinus rhythm with old anterior Q waves (see on EKG 1 year prior). No new ST changes. Initial cardiac markers: – CK 200 MB 9 Trop 0.8 Case 4 In this an ACS? – Unlikely – Troponin is his only marker of ACS and he has at least two reasons for false positive (CRF, CHF) How should this patient be managed – ASA if no contraindication – BB if not in CHF – No heparin or IIB/IIIA unless further evidence of ACS develops – Work up lethargy and altered mental status – Cycle biomarkers – Repeat EKG in 6-12 hours Case 5 A 55 yom presents to the ED c/o episodic chest pain for one week. The pain is sharp, left sided, and lasts 10-15 minutes. The pain occurs when walking and never at rest, although sometimes he can walk without symptoms. He is pain free now. EKG shows sinus rhythm without ST changes. Initial biomarkers – CK 90, MB not done, Trop <0.01 Case 5 In this an ACS? – Can’t tell – Some features consistent, some not How should this patient be managed – ASA and BB – No heparin or IIB/IIIA unless biomarkers become elevated – Cycle biomarkers – Repeat EKG in 6-12 hours – If rules out, consider exercise stress test