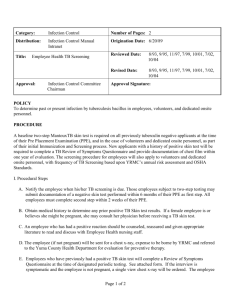
16Mycobacteriaceae2012 - Cal State LA
advertisement

Mycobacteriaceae Aerobic Gram-Positive Bacilli Form Filaments Stain Acid-fast FATHER DAMIEN (1840 – 1889) Lived and died for victims of Hansen’s disease (leprosy) on Molokai, Hawaii Mycobacterium: Genera • “fungus” “small rod” • Aerobic, fastidious, slow growing – Cell division 12-24 hr. – Lab culture 1-2 months • Large lipid content in cell wall, resistant to – – – – Disinfectants Detergents Common antibiotics Lab basic stains • ~100 species, many isolated in humans • Important human pathogens: – M. tuberculosis – “small swelling” – M. avian-intracellulare – “birds”; TB-like illness, common in AIDS patients – M. leprae – “scaly skin”; Hansen’s disease Nontuberculosis Mycobacteria: Runyon Classification • Based on growth rate, pigmentation • Non-Runyon Group: M. tuberculosis, M. leprae • Group I: Slow-Growing Photochromagen – No pigment grown in dark – Photoactivated pigment upon exposure to light • Group II: Slow-Growing Scotochromogen – Yellow, orange pigments grown in light or dark – Pigment deepens in two weeks • Group III: Slow-Growing Nonphotochromagen – Produce white, yellow pigment – Pigment not intensify upon exposure to light – M. avian complex • Group IV: Rapid Grower – Colonies in seven days Mycobacterium: Staining • G(+) bacilli, slender, branched filaments; stain poorly because of lipids (mycolic acid, waxD) in cell wall • Acid-fast stain – Presumptive diagnosis mycobacterial disease – Heating for stain penetration of high lipid cell wall – Stain penetrates, binds to mycolic acid, not remove with acid-alcohol treatment – Not easily decolorize, stain holds “fast”) Acid-Fast Stain • Ziehl-Neelsen stain – Carbol fuchsin - heat to penetrate – Acid-alcohol - decolorize – Methylene blue - counterstain • Kinyon stain – Carbol fuchsin – no heat, higher phenol allow penetration – Acid-alcohol - decolorize – Methylene blue - counterstain • Fluorochrome stain – – – – Auramine-rhodamine – stain, phenol Acid-alcohol - decolorize Acridine orange – counterstain UV microscope scan slide high dry, detect AFB by fluorescence – Read stained slide easier, faster Mycobacterium: Lab Culture • Work under biosafety cabinet • Specimen of choice – Patient coughs up sputum from lung – NaOH digest, decontaminate organic debris, RT normal flora – N-acetyl-L-cystine to liquify • Enrich, selective media – Egg or agar based – Antimicrobial agents - malachite green, cyclohexamide, nalidixic acid • Lowenstein-Jensen medium – egg based, colonies 18-24 days • Middlebrook 7H10, 7H11 medium – agar based, colonies 12-14 days Mycobacterium tuberculosis: Lab Culture • Solid media - rough, dry, granular, non-pigmented, buff color colony • Liquid media - contains Tween 80, albumin, faster growth • RT grow best 5-10% CO2 , 370 C • Skin lesion grow best, 30-330 C • RT culture 6-8 weeks before discard as negative • Skin lesion culture 12 weeks • CDC desires more timely report, possible with new DNA amplification methods of ID Mycobacterium: Lab ID • • • • Rate of growth Culture temperature Pigmentation and photoreactivity Biochemical testing: niacin production, nitrate reduction, catalase at 680 C, tween hydrolysis, arylsulfatase production, tellurite reduction, salt tolerance, pyrazinamidase production • Test of choice - DNA amplification; routinely done in PH lab, rapidly ID species Mycobacterium tuberculosis • Human only natural reservoir • Worldwide - third of population infected – ~2 billion people – ~8 million new cases/year – ~2-3 million deaths/year • USA ~10 million infected – Since 1985, dramatic increase number cases/year – Infections in homeless, drug and alcohol abusers, prisoners, AIDS patients – After 1992, now slowly decline due to increase PH prevention programs M. tuberculosis: Virulence Factors • Cord factor – cell wall glycolipid – Serpentine growth (filaments, cords), grow in close parallel arrangement – Toxic to leukocytes, anti-chemotactic – Role in development of granulomatous lesions • Iron capturing ability – required for survival inside phagocytes • Sulfolipids - prevent phagosome-lysosome fusion (important in intracellular survival) • Tissue damage - no known bacterial toxin or enzyme implicated; host immune response thought responsible, by inflammation, cell-mediate immunity (CMI) M. tuberculosis: Transmission • Close contact - person-to-person • Inhalation - infectious aerosols into alveolar spaces • Exposure to few organisms (10-200) may establish “infection” (elicit immune response, no disease) • Humans very susceptible to infection, but remarkably resistant to tuberculosis disease Primary Tuberculosis • Exposure - bacilli reach alveoli, ingested by macrophage • MO multiply - cause chemotactic response, recruits macrophages, T cells • Enzymes, cytokines release - start inflammatory response, wall off MOs (tubercle formation) • Inflammatory response also causes lung damage • Small number MO - no tissue damage • Large number MO - CMI response results in tissue necrosis • Patient becomes PPD skin test(+) Early Tubercle Reactivation Tuberculosis • Few weeks macrophages die - release bacilli, form caseous center in tubercle • In healthy individuals - disease usually arrested, lesions calcified • Tubercle bacilli - may remain dormant in lesion; later reactivation of disease • Host defenses fail - mature tubercle form; caseous center enlarge, liquify to form tuberculous cavity where bacilli multiply outside macrophage Mature Tubercle Extrapulonary Tuberculosis • Tubercle ruptures - release bacilli; disseminate throughout lung, circulatory, lymphatic system • Miliary (Extrapulmonary) TB – spread to lymph nodes, pleura, many other organs: – Progressive form of disease – Weight loss, coughing with blood, loss of vigor (old name consumption) Tuberculosis: Infection and Disease • In 3-6 weeks - patient’s CMI activated, bacteria replication stops • Within 2 years - 5% patients progress to active disease • Sometime later in life - 5-10% patients develop active disease • AIDS patient, TB infected: – Due to M. avian – 10% develop active disease within 1 year – 2x more likely to spread, rapidly progress to death – Impaired CMI unable to arrest infection M. tuberculosis: Treatment • Slow growth of MO, chronic infection require 6-9 months drug treatment • Combination of drugs to prevent emergence of resistant strains • Current recommended drugs: isoniazid (INH), ethambutol, pyrazinamide, rifampin • Drug resistance – 1990 report multidrug-resistant M. tb (MDRTB) in AIDS patients, homeless in N.Y., Miami – In developing countries, extensively drugresistant TB (XDR-TB), resistance to second line drugs, potentially untreatable M. tuberculosis: Prevention • BCG (bacille Calmette-Guerin) Vaccine – Attenuated M. bovis – Used where TB high – Reduce TB if vaccinated young age • Tuberculin skin test – PPD (purified protein derivative M. tb) injected under skin – Test host CMI response – Delayed-type hypersensitivity reaction (>10 mm induration), 48 hr., if previous or current infection; not necessarily active disease • Control disease – PH surveillance – Drug treatment and intervention – Case monitoring, prevent transmission M. avium-intracellular Complex • Common in soil, water, food • Before HIV - transient colonization in patients with compromised pulmonary function (bronchitis, obstructed pulmonary disease, previous infection); ~pulmonary TB • After HIV - USA most common mycobacteria disease in AIDS patients • Infection disseminated - all organs, large number MO M. avium-intracellular Complex • Transmission – ingestion of contaminated food or water, not person-to-person • Greatest risk for infection are immunocompromised • Multiply in localized lymph nodes, spreads to disseminated disease • Impair organ function due to replication MOs, host immune response • MO ubiquitous and control of exposure difficult Mycobacterium leprae: Hansen’s Disease • “to peel” “leprosy” • ~12 M cases worldwide (Africa, Asia, Latin America); rare USA • Reservoir of MO in armadillo • Does not grow in cell-free culture • Transmission by person-to-person, direct contact, inhale infectious aerosols • Requires prolonged, intimate contact for transmission • Two clinical forms of disease: – Tuberculoid – Lepromatous Hansen’s Disease • Mycobacteria obligate intracellular parasites in histiocytes, Schwann cells, epitheloid structures - called Lepra cells • Incubation period 2-4 years • Clinical manifestations depend upon adequacy of host CMI response • Like TB - many infected, few develop clinical symptoms of disease • Subclinical/Tuberculoid – infection contained by CMI • Lepromatous - large number bacilli in sputum, nasal secretion, skin Hansen’s Disease: Tuberculoid • Patient - strong CMI, weak antibody response • Lesions - skin, peripheral nerves, few in number; raised, erythematous margin, flat center • Nerve damage due to CMI response - loss sensation of touch, temperature; pain within lesion • Skin biopsy reveals many lymphocytic, epithelial cells, but no AFB • Infectivity, transmission low • Lepromin skin test (+) Hansen’s Disease: Lepromatous • Patient - strong antibody response, defective CMI (“foamy” macrophage, few lymphocytes, numerous bacilli) • Involve all areas of skin; waxy, nodular appearance, may thicken and fold • Destruction of cutaneous nerves, eyebrows, eyelashes, nasal septum • Skin biopsy reveals lymphocytes, many Lepra cells packed with AFB • Infectivity high • Lepromin skin test is (-) M. leprae: Treatment and Prevention • Tuberculoid form – rifampicin, dapsone; 6 months • Lepromatous – rifampicin, dapsone, clofazimine; minimum 1 year • Control by prompt recognition and treatment of infected patients • Lepromin skin test is similar to TB skin test The Gifts of Civilization: Germs and Genocide In Hawaii • O. A. Bushnell, University of Hawaii Press. 1993 • Hawaii isolated, difficult to reach by sea • 1778 – “discovered” by Captain Cook • Estimate ~1 million Hawaiian inhabitants • 1832 – census ~130,000 • 1900 - ~30,000 • Why decline? • Infectious diseases upon immune naive population i.e. STD, plague, cholera, TB, Hansen’s disease from Chinese immigrants, smallpox, chickenpox, measles, mumps, rubella; FATHER DAMIEN (1840 – 1889) The man who lived and died for the victims of Hansen’s disease (leprosy) Damien Born in Belgium 1840 • He was an ordinary boy, brother, and priest. • So what made him different? • Damien arrives Hawaiian Islands 1864 • He agreed to do a job that no one else would do. • He lived and worked for a group of people who had been sent away from their homes to a remote Hawaiian island, Molokai • They were outcasts because they had Hansen’s Disease. Hansen’s Disease • A scaly skin disease. • A chronic disease caused by a bacteria. • In those days there was no cure for Hansen’s Disease. • The outside world did not like to think about this awful disease, and chose to forget the people who suffered from it. • Damien gave back these people hope and pride. • He loved them like a family and in the end he died as one of them, a victim of Hansen’s Disease. • Damien’s life and death forced people to face the problem of Hansen’s Disease. • He said to the world that work needed to be done – and quickly! • Today, a cure for Hansen’s Disease has been found. • We no longer have to fear the disease or the people who suffer from it. • In 2009, for Father Damien’s many contributions to society, he was Canonized Saint Damien by the Vatican. Class Assignment • Textbook Reading – Chapter 26 Mycobacterium Tuberculosis – Omit: Clinical Significance and Differentiation of Nontuberculosis Mycobacterium • Key Terms • Learning Assessment Questions Case Study 7: Mycobacterium • A 35-year-old man with a history of intravenous drug use entered the local health clinic with complaints of a dry, persistent cough; fever; malaise; and anorexia. • Over the preceding 4 weeks, he had lost 15 pounds and experienced chills and sweats. • A chest radiograph revealed patchy infiltrates throughout the lung fields. Case Study 7: Mycobacterium • Because the patient had a nonproductive cough, sputum was induced and submitted for bacterial, fungal, and mycobacterial cultures, as well as examination for Pneumocystis organisms. • Blood cultures and serologic tests for HIV infection were performed. • The patient was found to be HIV positive. • The results of all cultures were negative after 2 days of incubation; however, cultures were positive for M. tuberculosis after an additional week of incubation. Case Study 7: Questions • 1. What is unique about the cell wall of mycobacteria, and what biologic effects can be attributed to the cell wall structure? • 2. Why is M. tuberculosis more virulent in patients with HIV infection than in nonHIV-infected patients? • 3. What is the definition of a positive skin test (PPD) result for M. tuberculosis? • 4. Why do mycobacterial infections have to be treated with multiple drugs for 6 months or more?