The Digestive System
advertisement

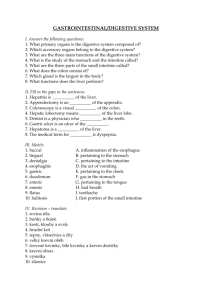
The Digestive System Functions of the Digestive System Ingest food Break down food into nutrient molecules Absorb molecules into the bloodstream Rid the body of indigestible remains Main Divisions of the Digestive System Alimentary Canal Continuous, muscular digestive tube winding throughout the body Digests and absorbs food particles Contains the following organs: Mouth, Pharynx, Esophagus, Stomach, Small and Large Intestines Accessory Digestive Organs Contains the following organs: Teeth, Tongue, Gallbladder, Salivary Glands, Liver, and Pancreas Digestive System Divisions Digestive Processes Ingestion Propulsion Mechanical digestion Chemical digestion Absorption Defecation Circulation of the Alimentary Canal/GI Tract Splanchnic Circulation Includes all arteries branching off the abdominal aorta and the hepatic portal circulation Arterial supply: Celiac Trunk (hepatic, splenic, and left gastric) Mesenteric Arteries: sup. and inf. Receives ¼ of the blood volume (CO); increases after a meal Histology of the Alimentary Canal/GI Tract From esophagus to anus, the walls of the alimentary canal have the same 4 layers: Mucosa (secretes hormones and mucus, absorbs end Submucosa (contains lymphoid follicles and elastic Muscularis externa (segmentation and peristalsis, products of digestion, and protects against infection tissue) contains inner circular layer and outer longitudinal layer, area where valves are found) Serosa (same as visceral peritoneum, made of areolar connective tissue) Histology of the GI Tract Peritoneum Peritoneum is the serous membrane lining the abdominopelvic cavity Visceral peritoneum covers the external surfaces of most digestive organs and is continuous with the parietal peritoneum that lines the body wall Between the two peritoneums is the peritoneal cavity Mesentery is a double layer peritoneum; provides routes for BV, lymphatics, nerves Alimentary canal organs are classified as Retroperitoneal - no mesentery and organs lies posterior to the peritoneum (SADPUCKER) Intraperitoneal - mesentery and organs lies within the peritoneal cavity Features and Functions of the Mouth Buccal/oral cavity Contains stratified squamous epithelium Vestibule: area bounded by lips and cheeks externally and teeth and gums internally Lips: posses no sweat or oil glands Palate: forms roof of the mouth, soft and hard palate, uvula Anatomy of the Mouth Features and Functions of the Tongue Helps grind food into a bolus which contains partially digested food and saliva Helps form words and is a sensory organ for taste Three surface features: Filiform papillae (roughness and grip) Fungiform papillae (contains taste buds) Circumvallate papillae (contains taste buds) Anatomy of the Tongue Features and Functions of the Salivary Glands Main functions: Produces and secretes saliva Cleanses the mouth Dissolves food chemicals so they can be tasted Moistens food, compacting it into a bolus Begins the chemical breakdown of food Salivary amylase: starch Types of Salivary Glands Submandibular Glands Sublingual Glands Found underneath the tongue Parotid Glands Found underneath the mandible Found anterior to the ear between masseter and skin Saliva travels to oral orifice via ducts from all three glands Anatomy of the Salivary Glands Composition of Saliva: 97-99.5% water pH 6.75-7.0 Sodium, potassium, chloride, phosphate, and bicarbonate Mucin Salivary amylase Features and Functions of the Teeth Break food into smaller parts, increasing surface area for digestion Types of Teeth Deciduous Teeth (“baby” teeth) Permanent Teeth Incisors- cutting and shredding Canines- piercing and tearing Molars- grinding Premolars- grinding and crushing Tooth Structure Crown: exposed portion of tooth covered by enamel which covers dentin Root: internal portion that is beneath the gums (gingiva) and is anchored by periodontal ligaments Deglutition and the Pharynx Deglutition = swallowing Oropharynx and Laryngopharynx are common passageways for food and air Pharynx contains stratified squamous epithelium (friction-resistant) Features and Functions of the Esophagus Muscular tube that propels food to stomach; bolus enters stomach through esophageal hiatus Skeletal muscle (upper third for swallowing) and smooth muscle (lower third) for peristalsis Esophageal glands – produce mucus to lubricate bolus Esophageal sphincter – prevents backflow into oral cavity Cardiac sphincter- prevents backflow into esophagus Anatomy of the Esophagus Microscopic Anatomy of the Esophagus Digestive Processes in the Mouth, Pharynx, and Esophagus Mouth processes: Ingestion Mechanical digestion (e.g. salivary amylase) Initiation of Propulsion Mastication: chewing Pharyngeal processes: Deglutition = swallowing Voluntary Buccal phase Involuntary Pharyngeal-Esophageal Phase Esophageal processes: Peristalsis (rhythmic contractions, involuntary) Deglutition and the Pharynx Peristalsis Features and Functions of the Stomach Temporary storage area for food and allows it to mix with gastric juice to produce chyme Regions: cardiac, fundus, body, and pyloric Greater and Lesser Curvatures: connected to greater and lesser omentums Rugae folds: longitudinal folds in stomach wall - mucous b/w folds Muscle layers arranged circularly, longitudinally, AND obliquely (aids in digestion) Anatomy of the Stomach Microscopic Anatomy of the Stomach Simple columnar epithelium – contains gastric pits that secrete gastric juices Goblet cells – secrete mucus that coats stomach and prevents it from being digested itself Parietal cells – secrete hydrochloric acid (converts pepsinogen into pepsin) and intrinsic factor (necessary for absorption of vitamin B12) Chief cells – secrete pepsinogen which is converted to pepsin to aid in protein digestion Enteroendocrine cells – release hormones such as: Histamine, Serotonin, Gastrin, Endorphins, and Somatostatin Histamine - activates parietal cells to release HCl Serotonin - contraction of stomach muscle Gastrin - gastric glands to increase secretion Endorphins - natural opiates Somatostatin - sympathetic n.s. - inhibits gastric secretion - inhibits gastric emptying Microscopic Anatomy of the Digestive System Digestive Processes in the Stomach Gastric Secretion Cephalic Phase Stimulated by the thought, sight, taste, or aroma or food Inputs from olfactory receptors and taste buds travel to parasympathetic enteric ganglia which then stimulate stomach glands Gastric Phase Stomach distension activates stretch receptors Food chemicals (e.g. peptides, rising pH) activate chemoreceptors which activate G cells which secrete gastrin Intestinal Phase Presence of low pH and partially digested foods in duodenum stimulates intestinal gastrin secretion Digestive Processes in the Stomach Gastric Motility and Emptying Peristaltic waves approach stomach and become stronger near pyloric region Pyloric sphincter allows ~ 3 mL of chyme to pass to duodenum and the rest to return to stomach for further mixing Features and Functions of the Small Intestine Receives chyme from stomach; performs majority of digestion and absorption of nutrients Regions: Duodenum (upper region receiving chyme from stomach and digestive enzymes from pancreas and bile from liver and gallbladder) Jejunum/Ileum (lower regions where absorption occurs) Plicae circulares (permanent folds in mucosa and submucosa that slow movement of chyme) Anatomy of the Small Intestine Microscopic Anatomy of Small Intestine Villi: fingerlike projections that increase the surface area of the SI Microvilli: tiny projections on the plasma membranes of columnar cells that appear fuzzy (i.e. brush border cells) Crypts of Lieberkuhn: secrete intestinal juice and special lysozymes that protect against bacteria Peyer’s Patches: aggregated lymphoid tissues containing lymphocytes Microscopic Anatomy of the Small Intestine Secretions of the Small Intestine Secretin: released by enteroendocrine cells when acidic chyme enters SI; causes release of bicarbonate-rich pancreatic juices Somatostatin: slows gastric motility and emptying and inhibits production of gastric secretions Cholecystokinin (CCK): released when fatty, proteinrich chyme enters SI; causes release of enzyme-rich pancreatic juices and bile Brush border enzymes: process long peptides, nucleic acids, and sugars into smaller ones After Digestion: Absorption Protein Fats Functions of the Liver Largest internal organ Functions: Filters and processes nutrient-rich blood of carbohydrates, proteins, and lipids from intestine Production and regulation of cholesterol Production of bile which emulsifies fats Removes drugs and hormones from circulation Storage of vitamins and minerals Anatomy of the Liver Right and Left Lobes: separated by falciform ligament Caudate and Quadrate Lobes: found on posterior side Blood vessels: Hepatic artery/vein and hepatic portal vein Gallbladder: found underneath left lobe, stores bile Gross Anatomy of the Liver Microscopic Anatomy of the Liver Liver Lobules: structural unit of liver Hepatocytes: liver cells contained within the lobules Hepatic portal vein & Hepatic Artery: the circulation of the liver, they bring blood into the liver where it is filtered through the liver sinusoidal capillaries Kupffer cells: remove debris Filtered blood drains into the central vein, then to the hepatic vein, and eventually to the inferior vena cava Bile (produced by hepatocytes) drains into the bile duct after passing through portal triad Bile then shipped to gallbladder for storage Microscopic Anatomy of the Liver Microscopic Anatomy of the Liver Blood supply - receives fresh O2 blood from hepatic artery (off of aorta) - receives deoxygenated blood with nutrients (from small intestine) - hepatic portal vein - From liver- hepatic vein- inferior vena cava Hepatic portal vein, hepatic artery and bile ducts make up the portal triad. Function and Regulation of Bile Bile ducts are present at every portal triad Bile flows down bile canaliculi (tiny canals) between adjacent hepatocytes towards bile duct branches at every portal triad Bile enters the bile ducts which drain into the common hepatic duct Bile emulsifies fats, separating them into smaller Bilirubin: the chief bile pigment, a waste product parts of the heme of hemoglobin formed during the breakdown of worn-out erythrocytes Regulation of Bile Production Bile exits cystic duct upon stimulation CCK released when acidic, fatty chyme enters intestines Causes: Gallbladder Contraction Pancreatic Juice Secretion Relaxation of hepatopancreatic sphincter Features and Functions of the Pancreas Pancreatic Juice secreted by acinar cells Islets of Langerhans release insulin and glucagon (important in glucose metabolism) Pancreatic Juice contains: Sodium Bicarbonate (buffers HCl in stomach) Proteases (break down polypeptides) Pancreatic amylase (digests oligosaccarides and disaccharides into monosaccharides) Pancreatic lipases (break down lipids into fatty acids and glycerol) Pancreatic nucleases (break down nucleic acids) Anatomy of the Pancreas Regulation of Pancreatic Secretion Features and Functions of the Large Intestine Functions: Reabsorption of remaining water and electrolytes Production and absorption of Vitamins B and K Elimination of feces Diameter is only 7 cm but is larger than that of the small intestine Gross Anatomy of the Large Intestine Teniae Coli: bands of smooth muscle that create pocket-like sacs (haustra) Cecum: sac-like connection between the small and large intestines Appendix: small structure containing lymphoid tissue; small immune function Ascending, Descending, Transverse, and Sigmoid Colon Splenic and hepatic flexure Rectum: storage area Anus: regulates defecation with two sphincter muscles; internal and external Anatomy of the Colon Microscopic Anatomy of the Large Intestine Simple columnar epithelium for absorption except in the anal canal where there is stratified squamous No villi, no digestive-secreting cells Goblet cells produce mucus for lubrication of feces Bacterial flora synthesize vitamin B and most of the vitamin K needed for blood clotting Microscopic Anatomy of the Large Intestine Summary of Digestion Summary of Digestion The Process of Absorption Clinical corner Peptic ulcers - gastric and duodenal, caused by Helicobacter pylori, NSAIDS, Hcl hypersecretion Cirrohsis - scarred liver due to chronic inflammation Hepatitis - A,B,C,D, and E Biliary calculi - gall stones - crystals of cholesterol in bile Borborygmus - rumbling noise caused by gas through intestines Cholecystitis - inflammation of gall bladder Colitis - inflammation of colon Dysphagia - difficulty in swallowing Enteritis - inflammation of the intestines Flatuation/erucation