PARENTERAL NUTRITION IN HAEMATOPOIETIC STEM CELL
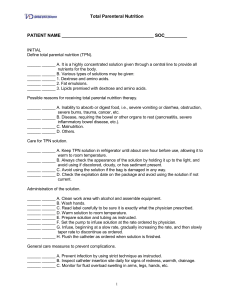
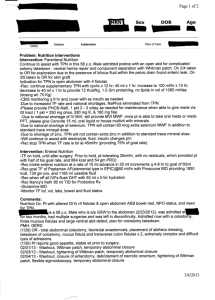
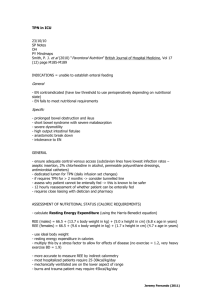
advertisement

PARENTERAL NUTRITION IN HAEMATOPOIETIC STEM CELL TRANSPLANTATION BY DR. IDEMUDIA J.O DEPARTMENT OF CHEMICAL PATHOLOGY UBTH, BENIN CITY OUTLINE: • INTRODUCTION • INDICATIONS FOR TPN IN HAEMATOPOIETIC STEM CELL TRANSPLANTATION • TIMING OF TPN • NUTRITIONAL CONTENT • BEGINNING TPN ADMINISTRATION • MONITORING • COMPLICATIONS • CONCLUSION INTRODUCTION • Parenteral nutrition is feeding a person intravenously, bypassing the usual process of eating and digestion. The person receives nutritional formulation that contains nutrients such as salts, glucose, amino acid, lipids, vitamins etc. • Parenteral nutrition is divided into two; (1) Partial parenteral nutrition in which case only part of the daily nutritional requirement is supplied, supplementing an oral intake. Many hospitalized patients are given dextrose, electrolytes or amino acid solutions by this • (2) Total parenteral nutrition (TPN) which supplies all daily nutritional requirements of the person. Because TPN solution is concentrated and can cause thrombosis of peripheral veins, a central venous catheter is usually required. INDICATIONS FOR TPN IN HAEMATOPOIETIC STEM CELL TRANSPLANTATION Mucositis of the gastrointestinal tract: • This is the main indication for TPN in patients undergoing HSCT • Usually develops within 7-10 days after chemotherapy and radiotherapy during conditioning of patient for BMT resulting in oroesophageal mucositis and gastrointestinal toxicity • This may result in decreased oral intake of food, nausea, vomiting, diarrhoea and decreased nutrient absorption which may last up to 2-3weeks after BMT Increased energy demand by the recipient • Metabolic effects of the conditioning regimens, and possible BMT complications such as sepsis and GVsHD • Impaired glucose tolerance resulting from steroid or cyclosporine administration or effect of BMT on pancreatic β cell function TIMING of TPN • TPN is often considered to be an expensive procedure and it is therefore started only when it becomes necessary • In some centres TPN is initiated before commencement of chemotherapy and irradiation and continued up to day 28 post BMT while in other centres, TPN is routinely initiated on day 1 after BMT and continued for 15 – 21 days NUTRITIONAL CONTENT • TPN requires water (30 to 40 mL/kg/day), energy (3060kcal/kg/day, depending on energy expenditure) amino acids and lipids (1 to 2g/kg/day depending on the degree of catabolism) vitamins and minerals. BASIC ADULT DAILY REQUIREMENTS FOR TOTAL PARENTERAL NUTRITION NUTRIENT AMOUNT Water (/kg body wt/day) 30–40 mL ENERGY (/kg body wt/day) Medical patient 30 kcal Postoperative patient 30–45 kcal Hypercatabolic patient 45–60 kcal AMINO ACIDS (/kg body wt/day) Medical patient 1.0 g Postoperative patient 2.0 g Hypercatabolic patient 3.0 g NUTRIENT MINERALS Acetate/gluconate Calcium Chloride Chromium Copper Iodine Magnesium Manganese Phosphorus Potassium SeleniumSome Trade Sodium Zinc AMOUNT 90 mEq 15 mEq 130 mEq 15 μg 1.5 mg 120 μg 20 mEq 2 mg 300 mg 100 mEq 100 μg 100 mEq 5 mg NUTRIENT AMOUNT VITAMINS Ascorbic acid 100 mg Biotin 60 μg Cobalamin 5 μg Folate (folic acid) 400 μg Niacin 40 mg Pantothenic acid 15 mg Pyridoxine 4 mg Riboflavin 3.6 mg Thiamin 3 mg Vitamin A 4000 IU Vitamin D 400 IU Vitamin E 15 mg Vitamin K 200 μg *Requirements for energy increase by 12% per 1° C of fever. BEGINNING TPN ADMINISTRATION • The first thing to do is to put a central venous catheter in place, because the central venous catheter needs to remain in place for a long time, strict sterile technique must be used during insertion and maintenance. The TPN line should not be used for any other purpose. The external tubing should be changed every 24hours with the first bag of the day. Dressing should be kept sterile and are usually changed every 48hours using strict sterile techniques. • The solution is started slowly at 50% of the calculated requirements, using 5% dextrose to make up the balance of fluid requirements. • MONITORING OF PATIENTS ON TPN • Progress should be followed on a flowchart. • Weight, electrolytes and blood urea nitrogen should be monitored daily. Plasma glucose concentration should be monitored every 6hours until patient’s blood glucose level becomes stable, blood tests can be done much less often. • If there is hyperglycaemia, 1iu of insulin should be added to every 10g of dextrose solution • Liver function tests, plasma total protein and albumin, plasma and urine osmolality, plasma calcium, magnesium and phosphate should be done twice a week until the patient is stable. • INDICES FOR MONITORING PATIENTS ON TPN BMI = ≥30kg/m2- Obesity 25-29.9kg/m2 – over weight <18.5kg/m2 – underweight NITROGEN BALANCE • Is the difference between nitrogen intake and nitrogen excretion. It is one of the major indicators of protein change and/or adequacy of feeding in a controlled setting. In a healthy adult anabolic and catabolic rates are in equilibrium, and the nitrogen balance approaches zero. Nitrogen balance is calculated as: 24hour-protein intake (g) 6.25 24hour UUN+4 Total Volume of urine(L) • Protein intake in grams is converted into grams of nitrogen by dividing by a factor of 6.25. • The factor of 4 represents non urinary losses of nitrogen (e.g from skin, faeces, hair, and nails) COMPLICATIONS: • About 5 to 10% of patients on TPN have complications related to central venous access, mainly sepsis. . Glucose abnormalities (hyperglycaemia or hypoglycaemia) or liver dysfunction occurs in >90% of patients. • TPN increases the risk of acute cholecystitis due to complete unusage of gastrointestinal tract, which may result in bile stasis in the gall gladder. ABNORMALITIES OF SERUM ELECTROLYTES AND MINERALS • This should be corrected by modifying subsequent infusion or, if correction is urgently required, by beginning appropriate peripheral vein infusions. • Volume overload: (Suggested by >1kg/day weight gain). • Metabolic bone disease: This occurs in patients receiving TPN for > 3months. There is severe pain in the back and lower extremities. Treatment is to temporarily stop TPN. • Adverse reaction to lipid emulsion: This occurs in the form of dyspnoea, cutaneous allergic reaction, nausea, head ache, back pain, dizziness and sweating. They are uncommon but may occur early, particularly if lipids are given at >1.0kcal/kg/hour. Temporary hyperlipidaemia may occur, particularly in patients with kidney or liver failure. Treatment is to either slow or temporarily stop lipid emulsion infusion. Conclusion: Despite all the complications associated with the use of TPN, its benefits cannot be overlooked and if all the necessary precautions are taken, the complications can be minimized.