Starting TPN in ICU
advertisement

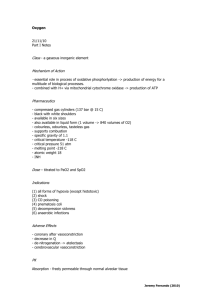
TPN in ICU 23/10/10 SP Notes OH PY Mindmaps Smith, P. J. et al (2010) “Parenteral Nutrition” British Journal of Hospital Medicine, Vol 17 (12) page M185-M189 INDICATIONS = unable to establish enteral feeding General - EN contraindicated (have low threshold to use perioperatively depending on nutritional state) - EN fails to meet nutritional requirements Specific - prolonged bowel obstruction and ileus short bowel syndrome with severe malabsorption severe dysmotility high output intestinal fistulae anastomotic break down intolerance to EN GENERAL - ensure adequate central venous access (subclavian lines have lowest infection rates – aseptic insertion, 2% chlorhexidine in alcohol, permeable polyurethane dressings, antimicrobial catheters) - dedicated lumen for TPN (daily infusion set changes) - if requires TPN for > 2 months -> consider tunnelled line - assess why patient cannot be enterally fed -> this is known to be safer - 12 hourly reassessment of whether patient can be enterally fed - requires close liaising with dietician and pharmacy ASSESSMENT OF NUTRITIONAL STATUS (CALORIC REQUIREMENTS) - calculate Resting Energy Expenditure (using the Harris-Benedict equation) REE (males) = 66.5 + (13.7 x body weight in kg) + (5.0 x height in cm) (6.8 x age in years) REE (females) = 66.5 + (9.6 x body weight in kg) + (1.7 x height in cm) (4.7 x age in years) - use ideal body weight - resting energy expenditure in calories - multiply this by a stress factor to allow for effects of disease (no exercise = 1.2, very heavy exercise BD = 1.9) - more accurate to measure REE by indirect calormetry most hospitalized patients require 25-30kcal/kg/day mechanically ventilated are on the lower aspect of range burns and trauma patient may require 45kcal/kg/day Jeremy Fernando (2011) NUTRITIONAL REQUIREMENTS Protein - utilisation of exogenous protein = 1.5g/kg/day - other techniques: -> non-protein calorie to nitrogen ratio (100-200kcal/g of nitrogen often used) -> nitrogen balance = (protein intake (g) / 6.25) – (urinary nitrogen (g) + 4) -> 4 = empirical factor added to account for non-urinary nitrogen loss (faeces and sweat) - cystalline solutions of L-amino acids (varying essential amino acids) Carbohydrates - daily requirement of glucose = 4-5g/kg/day in severely catabolic patients Lipids - requirements 1g/kg/day - 1/3 of energy given as non-protein - advantages: prevents fatty acid deficiency and provides more concentrated calories - disadvantages: can cause pancreatitis, immunosuppression, overfeeding -> increase in CO2 production - check lipids daily and check clearance of lipids Minerals and Micronutrients - Na+, K+, Ca2+, Mg2+, phosphate -> guided by serum plasma levels - inorganic trace elements - organic vitamins (thiamine, folic acid, fat soluble vitamins D, E, K, A, water soluble vitamins B and C) H2O - 25-40mL/kg/day (+ losses) MONITOR FOR COMPLICATIONS - catheter related sepsis catheter occlusion hyperglycaemia hypercholesterolaemia Jeremy Fernando (2011) - refeeding syndrome (phosphate, K+, Mg2+) - abnormal LFT’s - trace elemental deficiency: > 2-4 weeks of poor nutrition - copper: anaemia, neutropenia - iodine: hypothyroidism - chromium: glucose intolerance - zinc: mental apathy, diarrhoea, rash - selenium: cardiomyopathy -> treatment: supplement, follow levels (serum, tissue, white cells) PRESCRIPTION - total energy: 25 kcal/kg/day protein: 1.5g/kg/day carbohydrate: 4g/kg/day lipids: 1g/kg/day H2O: 30mL/kg/day + other losses electrolytes organic vitamins inorganic trace elements MY APPROACH - exhaust all means of feeding enterally dietician involvement calculate requirements (caloric and nutritional) start slowly monitor for refeeding and complications frequent reassessment about whether patient can be fed enterally Jeremy Fernando (2011)