Geriatric Psychiatry: Review and Update: Medical
advertisement

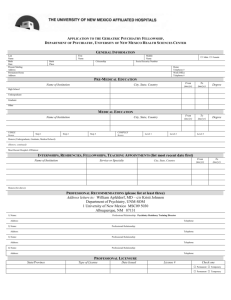
Geriatric Psychiatry: A Review & Update Medical and Neurologic Aspects J. Wesson Ashford University of Kentucky VAMC, Lexington Dementia Definition Multiple Cognitive Deficits: Memory dysfunction At least one additional cognitive deficit Cognitive Disturbances: Sufficiently severe to cause impairment of occupational or social functioning and Must represent a decline from a previous level of functioning Geriatric Psychiatry: A Review & Update Differential Diagnosis: Top Ten 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Alzheimer Disease (pure ~40%, + mixed~70%) Vascular Disease, MID (5-20%) Drugs, Depression, Delirium Ethanol (5-15%) Medical / Metabolic Systems Endocrine (thyroid, diabetes), Ears, Eyes, Environ. Neurologic (other primary degenerations, etc.) Tumor, Toxin, Trauma Infection, Idiopathic, Immunologic Amnesia, Autoimmune, Apnea, AAMI Geriatric Psychiatry: A Review & Update Diagnostic Criteria For Dementia Of The Alzheimer Type (DSM-IV, APA, 1994) A. Multiple Cognitive Deficits 1. Memory Impairment 2. Other Cognitive Impairment B. Deficits Impair Social/Occupational C. Course Shows Gradual Onset And Decline D. Deficits Are Not Due to: 1. Other CNS Conditions 2. Substance Induced Conditions E. Do Not Occur Exclusively during Delirium F. Not Due to Another Psychiatric Disorder Geriatric Psychiatry: A Review & Update Vascular Dementia (DSM-IV - APA, 1994) A. Multiple Cogntive Impairments B. Deficits Impair Social/Occupational C. Focal Neurological Signs and Symptoms or Laboratory Evidence Indicating Cerebrovascular Disease Etiologically Related to the Deficits D. Not Due to Delirium Geriatric Psychiatry: A Review & Update Factors Associated with Multi-infarct Dementia History of stroke (especially in Nursing Home) Step-wise deterioration Cardiovascular disease - HTD, ASCVD, & Atrial Fib Depression (left anterior strokes), personality change More gait problems than in AD MRI evidence of T2 changes (?? Binswanger’s disease) SPECT / PET show focal areas of dysfunction Neuropsychological dysfunctions are patchy Geriatric Psychiatry: A Review & Update Post-Cardiac Surgery 53% post-surgical confusion at discharge (delirium) 42% impaired 5 years later May be related to anoxic brain injury, apnea May be related to narcotic/other medication May occur in those patients who would have developed dementia anyway (? genetic risk) Cardio-vascular disease and stress may start Alzheimer pathology Any surgery may have a similar effect related to peri-op or post-op anoxia or vascular stress Geriatric Psychiatry: A Review & Update Newman et al., 2001, NEJM Drug Interactions Anticholinergics: amitriptyline, atropine, benztropine, scopolamine, hyoscyamine, oxybutynin, diphenhydramine, chlorpheniramine, many antihistaminics May aggravate Alzheimer pathology GABA agonists: benzodiazepines, barbiturates, ethanol, anti-convulsants Beta-blockers: propranolol Dopaminergics: l-dopa, alpha-methyl-dopa Narcotics: may contribute to dementia Geriatric Psychiatry: A Review & Update Depression Onset: rapid Precipitants: psycho-social (not organic) Duration: less than 3 months to presentation Mood: depressed, anxious Behavior: decreased activity or agitation Cognition: unimpaired or poor responses Somatic symptoms: fatigue, lethargy, sleep, appetite disruption Course: rapid resolution with treatment, but may precede Alzheimer’s disease Geriatric Psychiatry: A Review & Update Delirium Definition Disturbance of consciousness i.e., reduced clarity of awareness of the environment with reduced ability to focus, sustain, or shift attention Change in cognition (memory, orientation, language, perception) Development over a short period (hours to days), tends to fluctuate Evidence of medical etiology Geriatric Psychiatry: A Review & Update Ethanol Possibly Neuroprotective Accidents, Head Injury Dietary Deficiency Thiamine – Wernicke-Korsakoff syndrome Hepatic Encephalopathy Withdrawal Damage (seizures) Delayed Alcohol Withdrawal May not kill neurons directly Watch for in hospitalized patients Chronic Neurodegeneration Cerebellum, gray matter nuclei Geriatric Psychiatry: A Review & Update Medical / Endocrine Thyroid dysfunction Hypothyoidism – elevated TSH Hyperthyroidism Compensated hypothyroidism may have normal T4, FTI Apathetic, with anorexia, fatigue, weight loss, increased T4 Diabetes Hypoglycemia (loss of recent memory since episode) Hyperglycemia Hypercalcemia Nephropathy, Uremia Hepatic dysfunction (Wilson’s disease) Vitamin Deficiency (B12, thiamine, niacin) Pernicious anemia – B12 deficiency, ?homocysteine Geriatric Psychiatry: A Review & Update Eyes, Ears, Environment Must consider sensory deficits might contribute to the appearance of the patient being demented Central Auditory Processing Deficits (CAPD) Hearing problems are socially isolating Visual problems are difficult to accommodate by a demented patient, ?To do cataract op? Environmental stress factors can predispose to a variety of conditions Nutritional deficiencies (tea & toast syndrome) Geriatric Psychiatry: A Review & Update Neurological Conditions Primary Neurodegenerative Disease Focal cortical atrophy Primary progressive aphasia (many causes) Unilateral atrophy, hypofunction on EEG, SPECT, PET Normal pressure hydrocephalus Diffuse Lewy Body Dementia (? 7 - 50%) Fronto-temporal dementia (tau gene) Dementia with gait impairment, incontinence Suggested on CT, MRI; need tap, ventriculography Other Neurologic Conditions Geriatric Psychiatry: A Review & Update Tumor Toxins Trauma Geriatric Psychiatry: A Review & Update Infectious Conditions Affecting the Brain HIV Neurosyphilis Viral encephalitis (herpes) Bacterial meningitis Fungal (cryptococcus) Prion (Creutzfeldt-Jakob disease); (mad cow disease) Geriatric Psychiatry: A Review & Update Amnesic Disorders Amnesia Dissociative: localized, selective, generalized Organic - damage to CA1 of hippocampus Epileptic events thiamine deficiency (WKE), hypoglycemia, hypoxia Partial complex seizures Specific brain diseases Geriatric Psychiatry: A Review & Update Transient global amnesia Multiple sclerosis Age-Associated Memory Impairment vs Mild Cognitive Impairment Memory declines with age Age - related memory decline corresponds with atrophy of the hippocampus Older individuals remember more complex items and relationships Older individuals are slower to respond Memory problems predispose to development of Alzheimer’s disease Geriatric Psychiatry: A Review & Update Advances in Alzheimer’s Disease Uncovering etiology Understanding pathophysiology Better screening tools Improved diagnosis Developing interventions Etiology Age - therefore - design and stress Genetics (amyloid related) Relation to vascular factors, cholesterol, BP Education (? design vs protection) Environment - diet, exercise, smoking Geriatric Psychiatry: A Review & Update Neuropathology of AD Senile plaques Neurofibrillary tangles Neurotransmitter losses Inflammatory responses New Neuropath Mechanisms Amyloid PreProtein (APP - ch21) Tau phosphorylation (relation to dementia) Geriatric Psychiatry: A Review & Update Biopsychosocial Systems Affected by AD (all related to neuroplasticity) Social Systems Psychological Systems Basic ADLs - Late Primary Loss Of Memory Later Loss Of Learned Skills Neuronal Memory Systems Cortical Glutamatergic Storage Subcortical (acetylcholine, norepi, serotonin) Cellular Plastic Processes APP metabolism – early, broad cortical distribution TAU hyperphosphorylation – late, focal effect, dementia related Geriatric Psychiatry: A Review & Update Why Diagnose AD Early? Safety (driving, compliance, cooking, etc.) Family stress and misunderstanding (blame, denial) Early education of caregivers of how to handle patient (choices, getting started) Advance planning while patient is competent (will, proxy, power of attorney, advance directives) Patient’s and Family’s right to know Specific treatments now available, may delay nursing home placement longer if started earlier Geriatric Psychiatry: A Review & Update Need for Better Screening and Assessment Tools Genetic vulnerability testing Early recognition (10 warning signs) Screening tools (6th vital sign in elderly) Positive diagnostic tests CSF – tau levels elevated, amyloid levels low Brain scan – PET – DDNP, Congo-red derivatives Dementia severity assessments Tracking progression rate, prediction of change Geriatric Psychiatry: A Review & Update Alzheimer Warning Signs Top Ten Alzheimer Association 1. Recent memory loss affecting job 2. Difficulty performing familiar tasks 3. Problems with language 4. Disorientation to time or place 5. Poor or decreased judgment 6. Problems with abstract thinking 7. Misplacing things 8. Changes in mood or behavior 9. Changes in personality 10. Loss of initiative Geriatric Psychiatry: A Review & Update Assessment History Of The Development Of The Dementia Physical Examination Neurological Examination Geriatric Psychiatry: A Review & Update Neurological Exam Cranial Nerves Sensory Deficits Motor Deep tendon Pathological Geriatric Psychiatry: A Review & Update SCORE ALZHEIMER DETERIORATION ON THE MINI-MENTAL STATE EXAM OVER TIME 30 25 20 15 10 5 0 -5 0 5 10 AVERAGE TIME OF ILLNESS (years) Geriatric Psychiatry: A Review & Update AD all (easiest to hardest at p=.5) Mini-Mental State Exam items PROBABILITY CORRECT 1 0.9 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0 -4 -3 -2 -1 Geriatric Psychiatry: A Review & Update 0 1 2 3 4 5 6 7 8 DISABILITY ("time-index" year units) 9 10 PENCIL APPL-REP WATC LOCATION PENY-REP TABL-REP CLOS-IS RIT-HAND CITY FOLD-HLF SENTENCE COUNTY NO-IFS FLOOR SEASON YEAR PUT-LAP MONTH ADDRESS DRAW-PNT DAY SPEL_ALL DATE APPL-MEM PENY-MEM TABL-MEM Laboratory Tests ROUTINE Routine – Blood tests & Urinalysis EKG Chest X-Ray Anatomical Brain Scan – CT (cheapest), MRI SPECIAL Functional Brain Imaging (SPECT, PET) EEG, Evoked Potentials (P300) Reaction Times CSF Analysis - Routine Studies Heavy Metal Screen (24 hr urine) Genotyping Geriatric Psychiatry: A Review & Update Justification for Brain Scan in Dementia Diagnosis Differential Diagnosis: Tumor, Stroke, Subdural Hematoma, Normal Pressure Hydrocephalus, Encephalomalacia Confirmation of atrophy pattern Estimation of severity of brain atrophy MRI shows T2 white matter changes Periventricular, basal ganglia, focal vs confluent These may indicate vascular pathology SPECT, PET - estimation of regions of physiologic dysfunction, areas of infarction Helps family to visualize problem Geriatric Psychiatry: A Review & Update Geriatric Psychiatry: A Review & Update Geriatric Psychiatry: A Review & Update Geriatric Psychiatry: A Review & Update Geriatric Psychiatry: A Review & Update Ashford et al, 2000 INTERVENTIONS Only successful intervention – Available Interventions – Cholinesterase Inhibition (1st double blind study - Ashford et al., 1981) Not yet proven or unconvincing effects Promising Interventions Geriatric Psychiatry: A Review & Update Other Medical Conditions Chronic pain syndrome Medical consultation-liaison Other Neurological Conditions Parkinson’s disease Guillan Barre syndrome Huntington’s disease Seizure disorders – partial complex seizures Geriatric Psychiatry: A Review & Update Parkinson’s Disease Increases steadily after 50 years of age Pathophysiology Concomitant conditions Parkinson signs Symptomatic treatment Geriatric Psychiatry: A Review & Update Electroencephalography Seizure disorders Episodic behavior problems Primary neurodegeneration Temporal slow waves may be “normal” Focal slowing (stroke, focal cortical disease) Specific neurologic syndromes Possible partial seizure disorder Generalized slowing Sensitivity – 50% (90% after 3 recordings) Creutzfeldt-Jakob disease Sleep disorders In sleep studies: used to define stages Geriatric Psychiatry: A Review & Update Behavioral Problems In Dementia Patients Mood Disorders – depression – early in AD Psychotic Disorders Particularly paranoia, e.g, people stealing things Agitation Meal Time Behaviors Sleep Disorders Geriatric Psychiatry: A Review & Update Neuropsychiatric Treatments First treat medical problems Second environmental interventions Third neuropsychiatric medications Geriatric Psychiatry: A Review & Update Sleep Disorders Primary sleep problems Breathing-related sleep disorders Narcolepsy / primary hypersomnia Circadian rhythm disorders Parasomnias Secondary sleep problems Due to a psychiatric condition: depression, psychosis Due to a medical condition: arthritis, parkinson’s Substance induced disorders Fragmented circadian rhythms, sleep in AD Geriatric Psychiatry: A Review & Update Insomnia 15% of patients in sleep labs have sleep disturbance not associated with extrinsic factors or other conditions Periodic limb movement, restless leg syndrome Sinemet or anti-convulsants PTSD, nightmares (trazodone, prazosin) Jet lag (? melatonin) Drugs: caffeine, nicotine, Sleeping pill rebound Geriatric Psychiatry: A Review & Update