Chapter 5 - Victoria College
advertisement

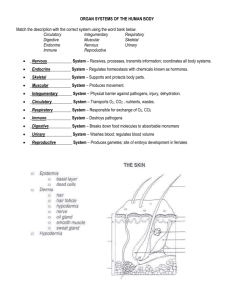
CHAPTER 5 The Integumentary System 1 INTRODUCTION • Integument = skin & accessory structures • Functions: – Guards body’s physical & biochemical integrity – Maintains constant body temperature – Provides sensory information about surrounding environment 2 STRUCTURE OF THE SKIN • Cutaneous membrane • Superficial portion = epidermis – composed of epithelial tissue • Deeper layer of skin = dermis – primarily connective tissue • Deep to dermis = subcutaneous layer (hypodermis) – not a part of skin – areolar & adipose tissue – fat storage – area for blood vessel passage – area of pressure-sensitive nerve endings 3 Principle Cells In Epidermis • Keratinocytes (90% of epidermal cells) – keratin: protect skin & underlying tissue from heat, microbes, & chemicals – lamellar granules: produce waterproof sealant • Melanocytes (8% of epidermal cells) – produce melanin •contributes to skin color •absorbs damaging ultraviolet (UV) light – sensitive to UV light 4 Principle Cells In Epidermis • Langerhans cells (small % of epidermal cells) – derived from bone marrow immune response – extremely sensitive to UV light • Merkel cells (least numerous cells) – contact flattened sensory neuron (Merkel disc) – function in sensation of touch 5 Layers of the Epidermis • Four or five layers, depending upon degree of friction & mechanical pressure applied to skin • From deepest to most superficial, the layers of the epidermis are: – – – – – stratum basale (stratum germinativum) stratum spinosum stratum granulosum stratum lucidum (only in palms and soles) stratum corneum 6 Stratum Basale • Also called stratum germinativum • Deepest layer of epidermis – Single layer of cuboidal or columnar keratinocytes – Merkel cells, melanocytes, & Langerhans cells – Tonofilaments eventually will form keratin in superficial layers – Desmosomes & hemi-desmosomes attach cells to each other & to basement membrane – Rapidly dividing layer • When destroyed, new skin cannot regenerate without a skin graft 7 Stratum Spinosum • Superficial to stratum basale • 8-10 layers of keratinocytes • Tonofilaments & desmosomes provide strength & flexibility • Langerhans cells & melanocytes also found in this layer 8 Stratum Granulosum • 3-5 layers of flat apoptotic keratinocytes • Tonofilaments more apparent • Lamellar granules release lipid that repels water • Keratohyalin converts tonofilaments into keratin • Keratinocytes die • **Transition between the metabolically active strata & dead superficial layer** 9 Stratum Lucidum • 3-5 layers of clear, dead, flattened keratinocytes • Present ONLY in fingertips, palms & soles ‘thick skin’ • Large amounts of keratin • Thickened plasma membranes 10 Stratum Corneum • 25 to 30 layers of flattened, dead keratinocytes • Continuously shed & replaced • Barrier to light, heat, water, chemicals & bacteria – Lamellar granules repel water • Callus = abnormal thickening of stratum corneum – from constant exposure to friction 11 Keratinization & Epidermal Growth • Stem cells in stratum basale divide to produce keratinocytes • Keratinocytes slowly pushed towards surface accumulate keratin @ each step •keratinization – occurs as cells move to skin surface (deep to superfic) – about 4 weeks from beginning to end • Epidermal growth factor (EGF) and other hormone-like proteins regulate epidermal growth • Psoriasis – Premature shedding of keratinocytes (7-10d) – Treated with UV light & topical ointment 12 Dermis • Connective tissue layer composed of collagen & elastic fibers, fibroblasts, macrophages & fat cells • Contains hair follicles, glands, nerves & blood vessels • Two major regions: – papillary region – reticular region 13 Dermis - Papillary Region • Top 20% of dermis • Mostly areolar CT – contains fine elastic fibers • Dermal papillae = finger-like projections – anchors epidermis to dermis – capillary loops feed epidermis – contains Meissner’s corpuscles & free nerve endings •touch sensations (Meissner’s) •heat, cold, pain, tickle, and itch 14 Dermis - Reticular Region • Attached to subcutaneous (sub-Q) layer • Dense irregular connective tissue – interlacing collagen bundles – coarse elastic fibers • Some adipose, oil glands, sweat glands, & hair follicles • Provides strength, extensibility & elasticity to skin – stretch marks = dermal tears from extreme stretching (striae) • Epidermal ridges form in fetus as epidermis conforms to dermal papillae fingerprints – genetically determined – increase grip of hand 15 Skin Pigments • Melanin produced in epidermis by melanocytes – tyrosinase converts tyrosine to melanin •UV light increases melanin production – differences in skin color determined by **AMOUNT** of pigment present • Clinical observations – freckles or liver spots = accumulation of melanocytes – mole = benign overgrowth of melanocytes – albinism = inherited lack of tyrosinase; no pigment – vitiligo = autoimmune loss of melanocytes in areas of skin produces white patches • Three pigments in dermis yield variety of skin colors – range from yellow to red & tan to black 16 Skin Pigments • Melanin – Pheomelanin (yellow to red) – Eumelanin (brown to black) – Increased synthesis results in “tan” protects from further damage (within limits) • Carotene in dermis – yellow-orange pigment (precursor of vitamin A) – found in stratum corneum & dermis • Hemoglobin – red, oxygen-carrying pigment in blood cells – epidermis is translucent so if other pigments not present, pinkness will be evident 17 Skin Color as a Diagnostic Tool • Color of skin and mucous membranes can provide clues for diagnosing certain problems – Jaundice •yellowish color to skin and whites of eyes •buildup of yellow bilirubin in blood from liver disease – Cyanosis •bluish color in nail beds and skin •hemoglobin depleted of oxygen looks purple-blue – Erythema •redness of skin due to enlargement of capillaries in dermis •caused by inflammation, infection, allergy or burns – Pallor = paleness of skin resulting from shock or anemia 18 Accessory Structures of Skin • Develop from embryonic epidermis • Cells sink inward during development to form: – hair – oil glands – sweat glands – nails 19 HAIR (PILI) • Present on all skin surfaces except palms, soles, & palmar/plantar surfaces of the digits • Eyebrows & lashes protect from foreign particles • Sense light touch • Anatomy – shaft – root – hair follicle • New hairs develop from cell division of matrix in the bulb 20 Structure of Hair • Shaft = superficial (visible) portion • Root = below the surface • 3 concentric layers – medulla •2-3 rows of irregularly. shaped cells – cortex •elongated cells – cuticle •single layer of thin, flat cells •heavily keratinized 21 Structure of Hair • Follicle surrounds root – Epithelial root sheath • external root sheath • internal root sheath • Dermal root sheath • surrounds follicle • Bulb = base of follicle • blood vessels (in papilla) • germinal cell layer (matrix) – arise from str. basale – **site of cell division** – gives rise to internal root sheath 22 Hair-Related Structures • Arrector pili – smooth muscle associated w/ hair – contraction causes goosebumps as hair is pulled vertically • Hair root plexus – surrounds follicle – touch-sensitive dendrites •detect hair movement 23 Hair Growth • Growth cycle = growth stage & resting stage – Growth stage • lasts for 2 to 6 years • matrix cells at base of hair root divide length – Resting stage • lasts for 3 months •matrix cells inactive & follicle atrophies •Old hair falls out as growth stage begins again – normal hair loss is 70 to 100 hairs per day • Rate of growth & replacement can be altered by illness, diet, blood loss, severe emotional stress, & gender • Chemotherapeutic agents affect rapidly dividing matrix cells 25 ACCESSORY STRUCTURES: Glands Specialized exocrine glands found in dermis: • Sebaceous (oil) glands • Sudiferous (sweat) glands • Ceruminous (wax) glands • Mammary (milk) glands 27 Sebaceous glands • • • • Usually connected to hair follicles Absent in palms and soles Secretory portion of gland is located in the dermis Produce sebum – lipid-rich, oily substance – moistens hairs – waterproofs and softens the skin – inhibits growth of bacteria & fungi • Acne – bacterial inflammation of sebaceous glands – caused by increased production of sebum 28 Sudoriferous glands • Simple, coiled tubular glands • Eccrine sweat glands (merocrine) = most common – secretory portion is deep in dermis – excretory duct terminates as pore at surface of epidermis – regulate body temp thru evaporation (perspiration) – help eliminate wastes such as urea 29 Sudoriferous glands • Apocrine sweat glands – limited distribution in body •found in armpit & groin regions – secretory portion in subcutaneous layer •secrete via exocytosis (merocrine manner) – excretory duct opens into hair follicle – more viscous sweat includes lipids & proteins – begin functioning @ puberty – responsible for cold sweats 30 Ceruminous Glands • Modified sudoriferous glands in external ear – produce waxy substance called cerumen – secretory portion in subcutaneous layer – excretory ducts open into ear canal or sebaceous gland – secretions = combination of oil & wax glands •sticky barrier against foreign substances • Impacted cerumen – abnormal amount of cerumen in external auditory meatus or canal – prevents sound waves from reaching ear drum 31 ACCESSORY STRUCTURES: Nails • Tightly packed, dead keratinized cells • Nail body – pink, visible portion • Free edge – extends past distal end of finger • Nail root – portion buried in fold of skin • Lunula – crescent-shaped area near proximal end • Hyponychium (nail bed) – secures nail to fingertip • Eponychium (cuticle) – stratum corneum layer • Nail matrix = growth region of nail 32 FUNCTIONS OF SKIN • Thermoregulation – Liberation of sweat lowers body temperature – Adjusts blood flow in dermis •Constriction of vessels = warming effect •Dilation of vessels = cooling effect – During exercise •moderate exercise: more blood brought to surface to lower temperature •extreme exercise: blood shunted to muscles & body temperature rises • Blood reservoir – extensive network of blood vessels – 8-10% total blood flow in adult 34 FUNCTIONS OF SKIN • Protection – – – – – physical, chemical & biological barriers keratin & tight cell junctions prevent bacterial invasion lipids retard evaporation pigment protects somewhat against UV light Langerhans cells alert immune system to presence of microbes, etc. • Cutaneous sensations – – – – touch pressure vibration tickle 35 FUNCTIONS OF SKIN • Synthesis of Vitamin D – UV light activates precursor molecule in skin – enzymes in liver & kidneys modify activated molecule to produce active form of vitamin D – necessary for absorption of calcium in the GI tract • Excretion/Absorption – 400 mL of water/day – 200 mL/day as sweat (for sedentary person) •excrete NH3, urea, salts via sweat – minimal absorption of fat-soluble vitamins 36 Transdermal Drug Administration • Method of drug absorption across epidermis & into blood vessels of dermis – drug contained in adhesive skin patch – drug absorption most rapid in areas of thin (scrotum, face and scalp) • Examples: – nitroglycerin (prevention of chest pain from coronary artery disease) – scopolamine (motion sickness) – estradiol (estrogen replacement therapy) – nicotine (stop smoking alternative) 37 Age-Related Structural Changes • Most age-related changes occur in dermis – Collagen fibers decrease in number & stiffen – Elastic fibers lose elasticity & thicken – Fibroblasts decrease in number •decreased production of collagen & elastic fibers •wrinkles • Decrease in number of melanocytes (gray hair, blotching) • Decrease in Langerhans cells (decreased immune responsiveness) • Reduced number and less-efficient phagocytes • Dermal blood vessels thicken – decreased nutrient availability – loss of subcutaneous fat 45 Photodamage • Ultraviolet light (UVA and UVB) both damage the skin • Acute overexposure causes sunburn • DNA damage in epidermal cells can lead to skin cancer • UVA produces oxygen free radicals that damage collagen and elastic fibers and lead to wrinkling of the skin 47 Skin Cancer • 1 million cases diagnosed per year • 3 common forms of skin cancer – basal cell carcinoma (metastasis rare) – squamous cell carcinoma (may metastasize) – malignant melanomas (rapid metastasis) •can result in death within months of diagnosis •key to treatment is early detection – ‘ABCD’ acronym •risks factors: skin color, sun exposure, family history, age & immunological status 48