Renal System
advertisement

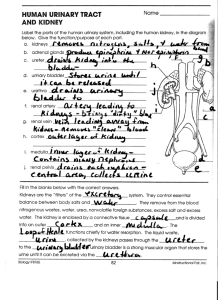
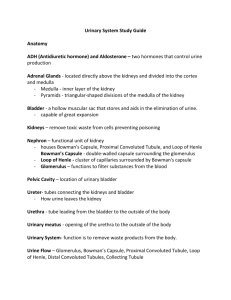
Formation of Urine Excretion or Conservation of Water Electrolyte Balance Acid-base Balance Activation of Vitamin D Production of Erythropoietin Production of Renin Glomerular filtration Glomerular filtration rate Tubular reabsorption › Include water and electrolytes Tubular secretion Urine concentration Renal Filtrate Kidneys form in 1 minute Averages 100-125 mL/minute Renin-angiotensin-aldosterone system › Role in blood pressure and sodium reabsorption Erythropoietin › Role in RBC production Vitamin D and calcium regulation Acid-base balance Ureters: carry urine from kidneys to bladder Bladder: temporary storage of urine and its elimination Urethra: carries urine from bladder to exterior Amount: 1000-2000 mL/24 hours Color: straw or amber Clarity: clear Specific Gravity: 1.010-1.030 › Lower=Dilute; Higher=Concentrated pH: 4.6-8.0 Constituents › 95% water › Waste products: Urea, Creatinine, Uric Acid Renal Mass Smaller Renal Flow Decreased 50% Decreased Tubular Function Bladder Muscles Weaken Bladder Capacity Decreases Voiding Reflex Delayed Nephrons lost with aging › Reduces kidney mass and GFR Less urine concentration › Risk for dehydration Health History Pain/Burning with Voiding New Onset Edema, Shortness of Breath, Weight Gain Fluid Intake Functional Ability Color, clarity, amount of urine Difficulty initiating urination or changes in stream Changes in urinary pattern Dysuria, nocturia, hematuria, pyuria Vital Signs Lung Sounds Edema Daily Weights Intake and Output Skin Assessment Urinalysis › Common test › Voided or Cath Specimen 24 hour Clean catch › 10 mL of urine collected › Color, odor, clarity Urine Culture › Identifies bacteria present › Urine collected before antibiotics › Sensitivity test determines antibiotic that will destroy bacteria Renal Function Tests › Serum Creatinine › Blood Urea Nitrogen › Uric Acid › Creatinine Clearance Test Kidneys-Ureter-Bladder › Show tumors, swollen kidneys, kidney stones Intravenous Pyelogram › Dye injected › Dye outlines renal structures › Check allergies › Increase fluids afterward Renal Angiography › Dye visualizes renal arteries › Check allergies Cystoscopy and Pyelogram › Surgery: Cystoscope inserted in bladder through urethra › Pyelogram: dye injected in kidney pelvis › X-rays taken Noninvasive sound waves examine anatomy of urinary tract Shows kidney enlargement, kidney stones, chronic infection, tumors Percutaneous or Open Before - NPO, Mild Sedative After › Vital signs › Observe for bleeding Biopsy site, Urine › Pressure dressing, sandbag › Bed rest for 24 hours Types › Stress › Urge › Functional › Overflow › Reflex total Postvoid residual urine Ultrasonic bladder scan Cystometrography Uroflowmetry Medications › Inhibit detrusor muscle contractions › Increase bladder capacity › Estrogen therapy Surgery › Bladder neck suspension › Prostatectomy Impaired Urinary Elimination Toileting Self-Care Deficit Social Isolation Evaluating › Keep voiding diary › Identify wetting episodes › Assess willingness to participate in social activities Teaching › Home environment › Voiding diary › Therapies Occurs when bladder cannot empty May be caused by obstructive or functional problem › Benign prostatic hypertrophy › Surgery › Drugs › Neurologic diseases › Trauma Acute › Anesthesia, medications, local trauma to urinary structures Chronic › Enlarged prostate, medications, strictures, tumors Manifestations › Overflow voiding › Incontinence › Firm, distended bladder May be displaced Monitor › Urine output › Bladder distention › Bladder Scan Residual volume of 150-200 cc urine Indicates need for treatment Complications › Hydronephrosis › Acute renal failure › Urinary tract infection Diagnostic tests › Portable bladder scan Treatment depends on cause › Surgery › Medications › Stimulation techniques › Catheterization Identify clients Take measures to promote urination Indwelling Catheters › Justifiable reasons Shock Urinary tract obstruction Neurogenic bladder › Urinary incontinence is NOT justification Urinary catheters result in infection Intermittent catheterization › Best › Reduces risk of infection › Patients may self-cath Suprapubic Catheter › Indwelling catheter inserted through incision in lower abdomen into bladder Invasion of urinary tract by bacteria Women > Men Aging › Older men due to enlarged prostate › Women due to declining estrogen › Nosocominal infections common Stasis of urine Contamination in Perineal/Urethral area Instrumentation Reflux of urine Previous UTIs Dysuria Urgency Frequency Cloudy, foul-smelling urine Urethritis: inflammation of urethra Cystitis: inflammation/infection of bladder wall Pyelonephritis: infection of the kidneys Dysuria, flank pain, fever, chills, malaise Urine examined for cloudiness, blood, foul odor Predisposing factors Urinalysis and culture results Urinalysis Urine culture & sensitivity CBC with differential IP Voiding cystourethrography Cystoscopy Acute pain Impaired urinary elimination Risk for injury Knowledge deficit Monitor symptoms Monitor intake and output Pain control Teaching › Medications: take all antibiotics – 3-7 days › Prevention Obstruction of urine flow is always significant Backup of urine destroys kidney Urethral Strictures › Urethra lumen narrowing due to scar tissue Renal Calculi › Hard, generally small stones › Kidney stones Nephrolithiasis Urolithiasis most common cause of obstructed urine flow Calculi › Masses of crystals formed from materials normally excreted in urine › Most made from calcium Etiology › Heredity › Chronic dehydration › Infection › Immobility › Men > Women Kidney/Pelvis › May be asymptomatic › Dull, aching flank pain Ureter › Acute severe flank pain, may radiate › Nausea/vomiting › Pallor › Hematuria Bladder › May be asymptomatic › Dull suprapubic pain › Hematuria Diagnosis › Kidney-ureter-bladder x-ray › Intravenous Pyelogram (IVP) › Renal ultrasound › Urinalysis Small stones passed IV fluids Pain control Thiazide diuretics Allopurinol Lithotripsy Medications Dietary management Surgery › Lithotripsy › ESWL › Cystoscopy › Nephrolithotomy › Nephrectomy Prevention › Foods › Hydration › Exercise Complications › UTIs › Hydronephrosis Nursing Diagnosis › Acute pain › Risk for infection › Deficient knowledge Monitor symptoms Strain all urine Intake and output Pain control Hydration Teaching Abnormal dilation of renal pelvis and calyces Results from urinary tract obstructions or backflow of urine Manifestations depend on how rapidly it develops Diagnosis › Ultrasound › CT scan › Cystoscopy Treatment › Stents Signs and symptoms › Frequency › Urgency › Dysuria › Flank and back pain › Renal failure Treat cause Urinary catheter Stents Nephrostomy tube › Intake and output › No clamping Focuses on prevention and ensuring urinary drainage Most common urinary tract cancer Men > Women Ages 50-70 years Etiology › Smoking › Industrial pollution Signs and symptoms › Early Painless Hematuria Signs and symptoms (cont’d) › Late Pelvic pain Lower back pain Dysuria Inability to void Diagnosis › Urinalysis Telomerase › Urine for Cytology, Culture › Cystoscopy and Transurethral Biopsy › IVP Therapeutic Interventions › Chemotherapy › Bacille Calmette-Guérin Vaccine › Photodynamic Therapy Therapeutic Interventions › Surgery Cystoscopy & Pyelogram with Fulguration Laser Robotic Laparoscopic Radical Cystectomy Urinary diversion Therapeutic Interventions › Incontinent urinary diversion Ileal conduit › Continent urinary diversion Kock pouch › Othotopic bladder substitution Studer pouch Hemi-Kock pouch Ileal W-Neobladder Nursing Care › WOC Nurse › Monitor urine output › Education › Preop and postop care Uncommon Renal cell carcinoma most common primary tumor Risk factors › › › › › › › › Smoking Obesity Renal calculi Hypertension Long term kidney dialysis Radiation exposure Asbestos Industrial pollution Most arise from tubular epithelium Can occur anywhere Often metastasize Often silent Later signs and symptoms › Hematuria › Dull pain in flank area › Mass IVP Cystoscopy and Pyelogram Ultrasound CT scan MRI Renal biopsy Therapeutic Interventions › Radical Nephrectomy › Nephron-sparing surgery › Radiation therapy › Immunotherapy › Chemotherapy Nursing Management › Monitor urine output › Education › Preop and postop care Pain Ineffective breathing pattern Risk for impaired urinary elimination Anticipatory grieving Flank pain Hematuria Treat injury Nursing Care › I&O › Vital signs › IV fluids › Pain control Multiple cysts in the kidney Signs and symptoms › Dull heaviness in flank/back › Hematuria › Hypertension › UTI Progressive No treatment Long-term complication of diabetes Most common cause of renal failure Atherosclerotic changes decrease blood to kidney Smaller doses of insulin as progresses Chronic renal failure develops Inflammatory condition of glomerulus Acute or chronic Primary kidney disorder or secondary to systemic disease Affects structure and function of glomerulus Damages capillary membrane › Blood cells and proteins escape into filtrate › Hematuria, Proteinuria, Azotemia Usually follows infection of group A betahemolytic Streptococcus Manifestations develop abruptly Hematuria, proteinuria, edema, hypertension, fatigue Anorexia, nausea, vomiting, headache Elevated BUN and serum creatinine Older adults may show less characteristic manifestations Symptoms may subside spontaneously Some may develop chronic glomerulonephritis Usually end-stage kidney damage Slow, progressive destruction of glomeruli Gradual loss of nephrons Kidneys decrease in size Symptoms develop slowly ASO titer ESR BUN Serum creatinine Serum electrolytes Urinalysis KUB x-ray Kidney scan or biopsy Signs and symptoms › Oliguria › Hypertension › Electrolyte imbalances › Edema › Flank pain Focus is on identifying and treating underlying disease process and preserving kidney function Medications Plasma exchange therapy Dietary management Renal failure treatment Vital signs Symptom support Rest Fluid, sodium, protein restrictions Renal failure care Education Preventing acute renal failure is goal of care Diagnostic tests › Serum creatinine, BUN › Creatinine clearance › Serum electrolytes, ABGs, CBC › Urinalysis › Kidney biopsy Kidneys unable to remove waste products from blood Acute or chronic Azotemia › Waste products accumulate Fluid, electrolyte, acid-base imbalances › Oliguric Rapid decline in function Abrupt onset Often reversible with treatment Risk factors › Major trauma, surgery, infection, hemorrhage, severe heart failure, lower urinary tract obstruction › Older adults at risk Prerenal Failure › Decreased blood supply to kidneys Intrarenal Failure › Damage to nephrons Postrenal Failure › Obstruction Nephrotoxins › Diagnostic Contrast Media (Dyes) › Medications IV Aminoglycosides, Tobramycin (Tobrex), Amikacin (Amikin), Cisplatin (Platinol) › Chemicals Prevention › Check serum BUN and creatinine prior to dyes or meds › Hydrate before/after contrast media › Monitor peak/trough levels of nephrotoxic drugs per institutional policy Phases › Oliguric › Diuretic › Recovery Therapeutic Interventions › Treat cause › Supportive treatment › Dialysis › Continuous renal replacement therapy Removes fluid continuously along with Hemodialysis Remove fluid/solutes in controlled, continuous manner in unstable patients Blood flows through Hemofilter, excess fluids/solutes move into collection bag Gradual decrease in kidney function Irreversible Slow, insidious process Final stage is end-stage renal disease Increasing in incidence Diabetic nephropathy and hypertension leading causes in U.S. Etiology › Diabetic Nephropathy › Nephrosclerosis › Glomerulonephritis › Autoimmune diseases Nephrons destroyed by disease process Remaining nephrons hypertrophy and have increased workload › Can compensate for a while Renal insufficiency develops – 75% of nephrons lost Further insult leads to ESRD › Uremia develops End-stage: 90% of nephrons lost Uremia: urea in the blood Affects all body systems Often not identified until uremia develops › Nausea › Apathy › Weakness › Fatigue › Confusion Fluid accumulation Electrolyte imbalance Waste products retained Acid-base imbalance Anemia Diet › High calorie › Low protein (unless dialysis) › Low sodium, potassium, phosphorus › Increased calcium › Vitamins Fluid restrictions Medications › Diuretics › Antihypertensives › Phosphate binders › Calcium/Vitamin D supplements › Kayexalate prn Dialysis › Symptoms of fluid overload › High potassium › Neurological signs › Uremia Hemodialysis › Artificial kidney removes waste products and excess water from blood Vascular Access › Temporary › LifeSite Hemodialysis Access System › A-V Graft › A-V Fistula Vascular Access Care › Thrill, Bruit › Protect › Postop NV checks, pain Elevate extremity Continuous dialysis done by patient Peritoneal membrane is semipermeable membrane, across which excess wastes/fluids move from blood Peritoneal catheter Exchange process: fill, dwell time, drain Excess fluid volume Imbalanced nutrition: less than body requirements Risk for infection Disturbed body image Activity intolerance Impaired skin integrity Risk for injury Excess fluid volume › Monitor weight › I&O › Fluid restriction › Monitor for fluid retention Electrolyte imbalance › Monitor levels › Dietary restriction › Monitor dysrhythmias Waste products › Oral care, skin care › Lotion › Protect from injury Impaired hematological function › Protect from injury/infection BPH tends to occur in men over 40 years of age Intervention is required when symptoms of obstruction occur The most common treatment is transuretheral resection (TURP) PSA › False high levels can be present for up to 12 days after a rectal examination or instrumentation around the prostate gland especially after a cystoscopy Signs and symptoms › Increased frequency with a decrease in › › › › › › amount of each voiding Nocturia Hesitancy Terminal dribbling Decrease in size and force of stream Acute urinary retention Bladder distention TURP › Preop teaching › Monitor urinary drainage system › Provide pain relief › Monitor urinary drainage system for clots › Irrigate bladder as prescribed › Monitor H &H › Monitor v/s Hematuria generally is present for at least 23 hours following a TURP Monitor color & content of urinary output Care post catheter removal › Monitor # of voids and amount › Have client collect urine in specimen cups Force fluids