Urinary system
advertisement

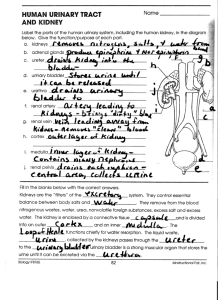
The Urinary System rev 4/11 • Excretion refers to the processes that remove wastes and excess materials from the body. • Urinary system has primary responsibility for – homeostasis of water and most solutes in blood and other body fluids. • Urine is essentially water and solutes. • Water is the most abundant molecule in our bodies. We excrete about 2 ½ liters of water per day, 1.5 liters per hour in urine. Urinary System 1 – Regulates nitrogenous and other solute waste (nitrogen from protein metabolism made into urea as waste) – Others: sodium, chloride, potassium, calcium, hydrogen ions, creatinine (waste product from muscle metabolism) toxic chemicals waste produced from liver and cellular metabolism, drugs, vitamins – Water is lost in urine, evaporation, feces. The urinary system is composed of the organs that produce, transport, store and excrete urine: – 2 kidneys, 2 ureters, one bladder and one urethra • The bladder stores urine (600–1000 ml) Urinary System 2 • The Kidneys – are bean shaped organs about the size of a clenched fist • Renal artery and renal vein connect each kidney to the aorta and inferior vena cava – are located in the abdominal cavity*, lateral to the 2nd lumbar vertebrae and close to our back. Urinary System 3 Kidney’s Role in Homeostasis Besides making urine, the kidney: • Maintains water balance: adjusts blood volume and blood pressure • Maintains acid–base balance and blood pH • Regulates red blood cell production (via the hormone erythropoietin) • Activates an inactive form of vitamin D Urinary System 4 Gross anatomy of the kidneys: • the capsule is the protective outer covering of the kidney • the interior of the kidney has 2 areas: the cortex and the medulla • the cortex is the outer portion. It has most of the capillary blood flow, and contains the nephrons (the functional unit of the kidney). Urinary System 5 • The kidney medulla is composed of cone shaped areas called pyramids. – The pyramids appear striped because they are formed of parallel bundles of microscopic urine collecting tubules, many loops of Henle and the collecting ducts. • The tips of the pyramids are called the papillae. These insert into the opening of the calyx. • Filtered urine is transported from the calyx to the kidney pelvis. • The pelvis empties into the ureters. Urinary System 6 • The smooth muscle of the ureters create peristaltic waves which move the urine into the bladder – The internal urethral sphincter and the external urethral sphincter prevent the bladder from emptying. – During urination, urine passes into the urethra. Urinary System 7 • The nephron is divided into several different areas: • a glomerular or Bowman’s capsule which surrounds the glomerulus • a proximal convoluted tubule • a loop of Henle, composed of a descending tubule, a loop, and an ascending tubule • a distal convoluted tubule • a collecting duct • blood vessels Urinary System 8 How a Nephron works to produce urine and also reclaim substances the body still needs: • The glomerular capsule surrounds the glomerulus which is a network of capillaries. • A tubule exits from the back of the glomerular capsule and continues as a long, thin tube with 4 areas: the proximal convoluted tubule The loop of Henle which is composed of Urinary System 9 • the descending limb • the actual loop • the ascending limb • the distal convoluted tubule • the collecting duct – • The collecting duct leads into the renal pelvis Urinary System 10 Blood vessels which supply the tubule • The renal artery supplies the kidney and branches many times. • Each nephron is supplied by a single afferent arteriole which enters a Bowman’s capsule and then divides to become the network of capillaries that makes up the glomerulus. • After filtering the blood, the capillaries rejoin to become the efferent arteriole. This divides again into the peritubular capillaries, another capillary network that surrounds the proximal and distal tubules in the cortex. Urinary System 11 • The peritubular capillaries remove water, ions and nutrients which are reabsorbed by the proximal and distal tubules. • Some efferent arterioles descend into the medulla and divide into capillaries called the vasa recta which supply the loop of Henle and the collecting duct. • After this, the efferent arterioles meet with efferent venules, flowing ultimately into the renal vein. Urinary System 12 Formation of Urine: Glomerular Filtration How do the kidneys select what to keep and what to excrete in urine? Urine formation involves 3 processes: 1. Glomerular filtration: filters fluid from glomerulus into Bowman’s capsule • Glomerular filtration is caused by the high blood pressure in the glomerulus, about twice as high as other capillaries. • Rate of filtration: – Resting rate is under local chemical control – Stress causes sympathetic nervous system to reduce blood flow to kidneys Urinary System 13 Formation of Urine: Tubular Reabsorption 2. Tubular reabsorption: returns water and needed solutes back to blood capillaries – Process: • Sodium moved by active transport from tubule cells to interstitial fluid and diffuses to capillaries • Chloride passively accompanies sodium to maintain a balanced electrical charge • Water reabsorbed with salts • Movement of sodium creates energy to transport glucose and amino acids into renal tubule then diffuses to the interstitial fluid Urinary System 14 Formation of Urine: Tubular Secretion 3. Tubular secretion: removes other substances from blood into the tubule to be excreted; can be performed either by passive diffusion or active transport – Purpose: removing or regulating chemical levels in body; excretion of harmful chemicals – Substances which can be secreted: penicillin, cocaine, marijuana, pesticides, preservatives, hydrogen ions, ammonium, potassium Urinary System 15 Concentration or Dilution of Urine: ADH The ability to dilute or concentrate urine depends on a high concentration of solutes in the renal medulla along with the ability to change the collecting ducts’ permeability to water • Dilute urine: excreting excess water – If you drink a lot of liquids, they are absorbed by the digestive system, enter your blood, increasing blood volume and decreasing the concentration of ions in your blood and body fluids. Urinary System 16 • Most of the water enters your cells • To prevent osmotic swelling and damage to cells, the kidneys reasorb less water and produce dilute urine. – Mechanism: cycling of NaCl and urea create a concentration gradient in the medulla that allows water to diffuse from the renal tubules into the interstitial fluid and then into the blood capillaries Urinary System 17 Concentrated urine: conserving water • If we drink too little liquid or sweat a lot, we may lower our blood volume, decrease our blood pressure, and risk dehydrating our cells. The kidneys compensate by reabsorbing more water and making a more concentrated urine. – Mechanism: Countercurrent exchange mechanism allows us to produce a more concentrated urine Urinary System 18 • Because of the hairpin turn in the loops of Henle, fluid flows in opposite directions in the 2 sides of the loop. This is called a countercurrent flow. –This allows a small difference in composition between the tubular fluid and the interstitial fluid to trigger reabsorption of liquid. – Increased ADH causes increased permeability to the collecting tubules and increased conservation of water Urinary System 19 Urination • Depends on a neural reflex: Micturition reflex – Internal urethral sphincter – External urethral sphincter As the bladder fills, it starts to stretch. • This sends a message to the spinal cord • Spinal cord nerves begin an involuntary reflex – Stretch receptor input goes to the brain • The brain can voluntarily override the micturation reflex Urinary System 20 Disorders of the Urinary System • Kidney stones – Minerals in urine crystallize in the renal pelvis and form kidney stones • Most are excreted with no problems • Can be removed surgically Urinary System 21 • Urinary tract infections – Refers to the presence of microorganisms in urine or in any part of the urinary system – Symptoms include swelling and redness around the urethral opening, a burning sensation or pain while urinating, difficulty urinating, bed wetting, low back pain, visible blood or pus in urine – Most are caused by bacteria that make their way up the urethra and can travel up the ureters to the kidneys – Most can be cured with antibiotics Urinary System 22 • Acute and chronic renal failure: – Kidney function impairment that is short term (acute) or long term (chronic) – Acute causes: • Sustained decreases in BP, large stones in the renal pelvis, infections, transfusion reactions, burns, severe injuries and toxic drugs or chemicals – Chronic (may also be called end state renal disease—ESRD): • Long term irreversible damage leading to a reduction in functioning nephrons with failure of the kidneys to function properly Urinary System 23 – Therapies: • Dialysis tries to duplicate the kidney function – CAPD-continuous ambulatory peritoneal dialysis (fluid left in abdomen for several hours) – Hemodialysis: blood is circulated through an artificial kidney machine • Kidney transplant—originally, biggest challenge is to find a good immunological match so the person’s body will not reject the foreign kidney – Now not enough people have offered to donate their organs after death Urinary System 24