Condition - Vision 2020 UK
advertisement
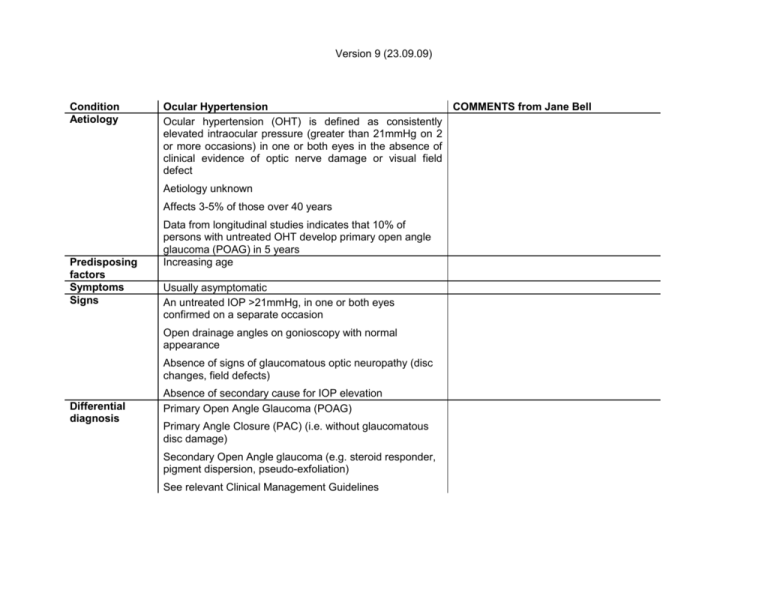
Version 9 (23.09.09) Condition Aetiology Ocular Hypertension COMMENTS from Jane Bell Ocular hypertension (OHT) is defined as consistently elevated intraocular pressure (greater than 21mmHg on 2 or more occasions) in one or both eyes in the absence of clinical evidence of optic nerve damage or visual field defect Aetiology unknown Affects 3-5% of those over 40 years Predisposing factors Symptoms Signs Data from longitudinal studies indicates that 10% of persons with untreated OHT develop primary open angle glaucoma (POAG) in 5 years Increasing age Usually asymptomatic An untreated IOP >21mmHg, in one or both eyes confirmed on a separate occasion Open drainage angles on gonioscopy with normal appearance Absence of signs of glaucomatous optic neuropathy (disc changes, field defects) Differential diagnosis Absence of secondary cause for IOP elevation Primary Open Angle Glaucoma (POAG) Primary Angle Closure (PAC) (i.e. without glaucomatous disc damage) Secondary Open Angle glaucoma (e.g. steroid responder, pigment dispersion, pseudo-exfoliation) See relevant Clinical Management Guidelines Version 9 (23.09.09) Management by Optometrist NonDiagnosis: diagnosis of OHT and formulation of a pharmacological management plan can be made by a suitable trained optometrist with a specialist qualification (when not working under the supervision of a consultant ophthalmologist) and relevant experience. Pharmacological Management category COMMENTS What specialist qualification will be required? All patients with OHT should be offered the following tests: IOP measurement using Goldmann applanation tonometry, gonioscopy, central corneal thickness measurement, visual field measurement using standard automatic perimetry and optic disc assessment (NICE recommendation) Gonioscopy and pachymetry are only required for diagnosis not monitoring Follow up management: people with confirmed OHT can be monitored by optometrists with a specialist qualification (when not working under the supervision of a consultant ophthalmologist) and relevant experience (NICE recommendation) Optometrists with a specialist qualification (when not working under the supervision of a consultant ophthalmologist) and relevant experience can manage OHT (including the prescription of ocular hypotensive drugs) (NICE recommendation) Diagnosed OHT can be monitored by all optometrists as this requires GOC core competencies For specific management of OHT refer to NICE guideline (see Evidence For Optometrists without a specialist qualification when not working under the supervision of a Consultant Ophthalmologist: B1 (modified): no intervention, routine referral to Consultant Ophthalmologist For Optometrists with a specialist qualification and relevant experience (or working under the supervision of a Or an optometrist with a specialist qualification Version 9 (23.09.09) Consultant Ophthalmologist): B2: alleviation or palliation, no referral Possible management by Ophthalmologist Confirmation of diagnosis Determination of the individual clinical management plan Reduction of IOP pharmacologically in patients at moderate or high risk of conversion to POAG Evidence base Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, Parrish RK 2nd, Wilson MR, Gordon MO. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary openangle glaucoma. Arch Ophthalmolol. 2002, 120:701-13. Authors’ conclusion: Topical ocular hypotensive medication was effective in delaying or preventing the onset of POAG in individuals with elevated IOP. Although this does not imply that all patients with borderline or elevated IOP should receive medication, clinicians should consider initiating treatment for individuals with ocular hypertension who are at moderate or high risk for developing POAG Centre for Evidence-based Medicine Level of Evidence = 1a For recommendations regarding OHT diagnosis and management, refer to the NICE Guideline. Glaucoma: diagnosis and management of chronic open angle glaucoma and ocular hypertension http://www.nice.org.uk/guidance/CG85 Or CRVO