My Most Commonly Asked Questions Related to Glaucoma
advertisement

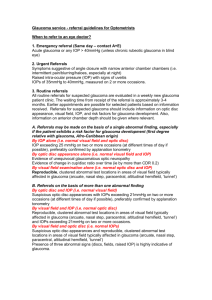
My Most Commonly Asked Questions Related to Glaucoma Murray Fingeret, OD Murray Fingeret, OD Clinical Professor, SUNY College of Optometry Chief, Optometry Section, Dept Veterans Affairs, NYHHCS, Brooklyn, NY 718-298-8498 murray.fingeret@va.gov This course will discuss the most common questions I receive. Examples are: should IOP be converted based upon corneal thickness, is there a need to treat if glaucomatous damage is not present, what should I do for therapy after using prostaglandins. These are other questions related to both diagnosis and therapy will be addressed. 1. Is the optic nerve the first site of glaucomatous damage? The structure-function relationship will be explored, illustrating examples where the optic nerve changes first, followed by selective field loss (SWAP, FDT) and then loss on standard automated perimetry. Still looking at Ocular Hypertension Treatment Study (OHTS) data, fields are often the initial way that glaucoma is diagnosed. 2. Is pachymetry a standard of care? The role of corneal thickness measurements will be discussed and why this test is crucial to better understand the intraocular pressure (IOP) within the eye. Is role as a surrogate for risk will be described based upon OHTS data. 3. Do you correct the IOP for corneal thickness? Clinicians have been besieged with conversion charts, often used by companies for marketing purposes, and are confused about their importance. The issue that there is no accepted algorithm will be described. Also, other biomechanical factors such as corneal rigidity play a role in IOP measurements and why a simple conversion chart often does not work well. 4. Is a person who has had refractive surgery at a greater risk for developing glaucoma? This common question relates to the naturally thin cornea offering greater risk for glaucoma development. A surgically thin cornea does not have this risk but rather will simply underestimate the IOP. 5. Are risk calculators useful in determining which individuals with ocular hypertension should be treated? Risk assessment is becoming a new tool useful to recognize which individuals with ocular hypertension are at risk of developing glaucoma and deserve therapy. Risk assessment as a tool will be discussed. Data from OHTS has shown that rather than 1% of inviduals with OHTN developing glaucoma per year, when we look at IOP, Cup/Disc ratio, visual fields, age and corneal thickness- the figure for some increase to 7% conversion per year. It is those individuals in which therapy is considered. 6. Is Diabetes a risk factor for Glaucoma? Recent work has shown that diabetes is neither protective or a risk factor for glaucoma when one has ocular hypertension and should not be used when deciding whether to initiate therapy. 1 7. What Harm will occur if we wait until glaucomatous damage is present? An important question is whether glaucoma is like cancer, requiring early therapy to prevent damage from accelerating over time. This assumption is one reason why ocular hypertension is often treated. There is no data to support the concept of early therapy or waiting at this time, and with the new tools for risk assessment we are aiming preventive therapy at those most at risk. 8. Is Goldmann tonometry outdated? Should we adopt one of the new tonometers? While Goldmann tonometry is 50 years old, we are comfortable with the data we receive and understand how to use it. While not perfect, it will take awhile before the newer instruments are adopted. 9. Is their a role for peripheral field testing in glaucoma? Peripheral fields were evaluated 25 years ago and never adopted due to a host of reasons including variability in the periphery. The peripheral threshold tests do not offer probability limits because of the overlap between normal and abnormal results, reducing its use to that of a screening test. 10. Is there a need for more sensitive perimetric tests such as FDT or SWAP? A twenty year quest has been to improve the ability of visual fields to discover visual field damage early on. SWAP and FDT are two tests meant to discover such change. While they have problems, they do offer another method to explore the field. 11. Can the Matrix perimeter replace my standard one currently in use in the management of my patients with glaucoma? Perimeters are evolving and while the Matrix perimeter uses a different stimulus, nonetheless it performs quite well and can be used in the management of glaucoma. The larger issue is whether the instrument stores the data as well as has tools to analyze the fields for change. 12. Have optic nerve imaging become a standard of care? Standard of care issues are difficult to address and in fact evolve over time as the instruments mature and become commonly used. Still imaging of any form is useful and important to aid clinicians in recognizing early change as well as detecting progressive loss. 13. What target IOP is needed to treat glaucoma? Target IOPs are an important goal, and provide direction to the clinician. The target IOP is related to the amount of damage present as well as the IOP level. Still no magic number exists and it is a floating number as each case is individualized. 2