Pacers, ablation, cardioversion, telemetry, Intro to ACLS
advertisement

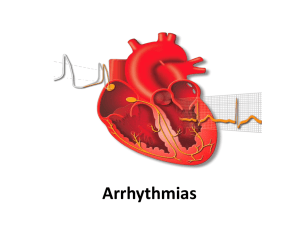
Nursing Interpretation of the Electrocardiogram (ECG), Telemetry By: Teresa Champion MCC NURS 2140 OBJECTIVES • Describe the configuration of the normal electrocardiogram (ECG). • Identify and calculate heart rate, rhythm, PR interval, QRS complex, and QT interval for normal and abnormal cardiac rhythms. • Discuss the etiology and significant ECG features of the following dysrhythmia classifications: sinus, atrial, junctional, block, ventricular, and asystole. • Interpret the significance of each of the dysrhythmias and formulate nursing responsibilities for each dysrhythmia. • Identify normal rhythms and dysrythmias. • Identify ECG complexes and artifact. • Perform ECG rhythm strips. • Identify correct dysrythmia terminology Cardiac Conduction System –3 Main Parts: • SA node (Sinoatrial node) • AV node (Atrialventricla node) • HIS-Perkinje System VIDEO OF CONDUCTION SYSTEM http://www.nhlbi.nih.gov/health/dci/Disease s/hhw/hhw_electrical.html Anatomy of the Heart - CARDIAC CELLS • Two types of cardiac cells – Myocardial & Pacemaker cells • • • • Automaticity Excitability Conductivity Contractility Anatomy of Heart – Cardiac Chemistry Function • Electrolytes Affecting Cardiac Function • Depolarization/Repolarization • Cardiac Output (CO): The amount of blood the heart pumps out to body in 1 min. NORMAL: 5 to 8 L • CO= HR x SV (CO can be changed by altering heart rate, stroke vol. or both) • Stroke Volume = the amount of blood that the • heart ejects in one beat which • depends on activity level, physical • condition, prior heart disease Cardiac Wave Form on Electrocardiogram (ECG) • • • • • • • • • P wave PR interval QRS complex J point ST Segment T wave QT Interval R to R Interval U wave (not always present) ECG Wave Form 8 ECG Lead Placement in Telemetry • 1. The white lead is placed on the right side of the chest. This is usually called the “right arm lead.” • 2. The black lead is placed on the left side of the chest. This is called the “left arm lead.” • 3. The green lead is placed on the right lower abdomen, it is called the “right leg lead.” • 4. The red lead is placed on the right lower abdomen, it is called the “left leg lead.” • 5. The brown lead is placed slightly to the right of the midsternum, it is called the “V lead or chest lead.” • 6. The grey lead is Lead Placement ECG Telemetry White lead Black Lead Brown Lead Green Lead Red Lead ECG Graph Paper Heart Rate on ECG • Heat Rate – Fastest count R waves in 6 second strip and times by 10. – Count R waves on a full minute strip for accurate HR for irregular rhythms. – Another way is to count the number of small boxes between R waves and divide the total by 1500. 1 2 3 4 5 6 7 8 big box (5 small boxes) is equal to a HR of 300 big boxes is hr of 150 (300/2) big boxes is hr of 100 (300/3) big boxes is hr of 75 (300/4) big boxes is hr of 60 (300/5) big boxes is hr of 50 (300/6) big boxes is hr of 43 (300/7) big boxes is hr of 38 (300/8) 13 Large box estimate of heart rate works with regular rhythms • A dysrhythmia is a disturbance of the rhythm of the heart caused by a problem in the conduction system. • Categorized by site of origin: atria , AV nodal, ventricular • Blocks are interruptions in impulse conduction: 1st, 2nd type 1&2, 3rd or complete heart block 15 P wave Measures: 0.12-0.20 16 QRS WAVE Measures: 0.06-0.10 17 QT Wave Measures approx 0.360.48 seconds 18 Heart rates • NSR: heart rate is 60-100bpm • ST: heart rate 101-180 bpm • SB: heart rate <60 bpm 19 Sinus rhythm • • • • PR interval- 0.12-0.20sec QRS-0.06-0.10sec QT segment 0.36-0.44 sec Heart rate 60-100 20 Atrial arrhythmias • • • • • • • Sinus tachycardia Atrial tachycardia Sinus bradycardia Premature atrial contraction (PAC) Supraventricular tachycardia Atrial fibrillation Atrial flutter 21 Sinus Tachycardia Atrial Tachycardia Sinus Bradycardia Premature Atrial Contraction (PAC) SupraVentricular Tachycardia (SVT) Atrial Fibrillation (Afib) Atrial Flutter Atrial fib/flutter 29 Other Atrial Dysrhymias • Wolf Parkingson-White Syndrome (WPW) • Wandering Atrial Pacemaker (WAP) • Sick Sinus Syndrome (SSS) Management of Atrial Dysrhymias • Assess pt response/Monitor Vital Signs • May cause drop in Cardiac Output (CO) • Notify MD (Health Care Practitioner) – Intervention to convert back to NSR • Increase rate – slow rates, Administer drugs (Atropine), Transcutaneous Pacing – Control rate – if fast Ventricular Response (ie: A-fib, SVT, Aflutter) – Anticoagulate – Cardioversion How to treat SVT • B-blockers ( to decrease conduction thru AV • node: • Calcium channel blockers ( to decrease conduction • thru AV node) • Radio frequency ablation • SVT converted with Adenosine given rapid IV Push stimulates vagal response. 32 Atrial Fibrillation • • • • • • • - - 5 to 6 times more likely to have stroke - - atrial rate: 300 to 600 times/minute --prolonged A-Fib may stretch & weaken heart muscle - - symptoms: lightheaded, very tired, SOB, diaphoretic, chest pain, 33 A Fib electrical cardioversion: • High risk of forming clots & causing stroke • Anticoagulants taken before treatment and 34 weeks post treatment • If life-threatening, may need Heparin IV before cardioversion • Best time: recent A fib 34 Ventricular arrythmias • • • • • • • • Junctional rhythms AV blocks Premature ventricular contraction (PVC) Ventricular Tachycardia (V-tach) Ventricular Fibrillation (V-Fib) Torsade de Pointes (TdP) Pulseless electrical activity (PEA) Asystole 35 Junctional Escape Rhythm Accelerated Junctional Rhythm AV Blocks • • • • • First degree block Second degree block Type I (Wenchebach) Second degree block Type II (Mobitz II) Third degree block Bundle branch block 38 Rate is usually WNL Rhythm is regular Pwaves are normal in size and shape The PR interval is prolonged (>0.20 sec) but constant 39 Pwaves are normal in size and shape; Some pwaves are not followed by QRS PR interval: lengthens with each cycle until it appears without QRS Complex then the cycle starts over QRS is usually narrow 40 http://www.youtube.com/watch?v=GVxJJ2 DBPiQ&feature=related •Ventricular rate is usually slow •Rhythm is irregular •Pwaves are normal in size and shape (more pwaves than QRS) •PR interval is within normal limits •QRS is usually wide 42 •Ventricular rate is regular but there is no correlation between p-waves and QRS •P waves are normal in size and shape •No true PR interval 43 44 PVC Unifocal Multifocal 45 PVC: ventricular origin • Complex is wide followed by compensatory pause • An irritable focus in ventricle initiates a contraction before normally expected beat. • Acute MI most common cause • QRS is wide and bizarre • Risks: increasing myocardial irritability, leading to increased freq. of PVCs • Can occur as bigeminy (every other beat) • or short runs 46 Ventricular tachycardia Monomorphic: beats are same size and shape Polymorphic: different size and shape 47 This is a polymorphic VT Usually electrical imbalance in r/t NA+ or K+ 48 49 V-tach • Advanced irritability of ventricles due to ASHD, CHF, acute MI electrolyte imbalance. Hypoxia, acidosis, occasionally drugs • RISKS: low to no Cardiac output • Nursing Interventions: monitor, if pt unconscious, immediately defibrillate 50 Torsade de pointes • Will see prolonged QT interval when in sinus rhythm • Will see prominent U wave • If lasts >10 seconds pt will progress to unconsciousness, life threatening with ineffective cardiac output • TREATMENT: IV magnesium 51 Ventricular Fibrillation (Course) 52 Ventricular Fibrillation (Fine) Vtach/Vfib • • • • • Both can be life threatening VT= V HR 100-250 bpm Causes: AMI, CAD, hypokalemia, dig toxic S/S: palpitations, dizzy, angina, <LOC Treatment: assess for pulse, if none, defibrillate • VF=Rate undeterminable Cause: same • Treatment: CPR, Defibrillate 54 V-fib • • • • • • • • • • May occur after MI Extensive ventricular irritability Very little or no cardiac output (No Pulse) Death within 4 to 8 minutes TREATMENT: immediate defibrillation immediate defibrillation at 200 J (100J) if unsuccessful, repeat at 300 J (150J) If unsuccessful, repeat at 360 J (200J) CPR If do not know type of defibrillator start at 200J 55 Asystole 56 Pulsless Electrical Activity (PEA) Asystole and PEA • CPR Oxygen • Epinephrine 1 mg IV/IO (repeat 3-5 minutes) • May give Vasopressin 40U IV/IO to replace • 1st or 2nd dose of epinephrine • Consider Atropine 1 mg IV/IO Repeat every 3 to 5 min (up to 3 doses) 58 Pacer spike should fall before the P wave unless a dual Chamber pacemaker; if it does not there could be a problem 59 ARTIFACT 61 http://www.campaignfornursing.com/events/WINNERS/pennsylvania/ 62