Body Cavities by Dr Zahra Haider Bokhari
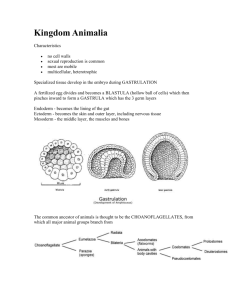
advertisement

3RD WEEK AXIAL › Prechordal mesenchyme › Cardiogenic › Septum transversum PARAXIAL INTERMEDIATE LATERAL PLATE 4th wk. Inverted U shaped cavity in: › Cardiogenic area › Lateral plate mesoderm Bend –cranial to prochordal plate – primitive pericardial cavity Limbs of U – lateral half of disc Limbs : › Pleural cavity › Peritoneal cavity Initial part of limbs – flank foregut Caudal part of limbs – communicate with extraembryonic coelom The two limbs are called pericarioperitoneal canals 4th week Pericardial cavity – ventral below foregut Pericardial cavity bend at right angle – communicate with pericardioperitoneal canal Pericardioperitoneal canal › Dorsal to septum transversum › Lateral to foregut Pleuroperitoneal canals – Ventral aspect Merge – single peritoneal cavity The coelome lined by mesothelium Derived from: Somatic mesoderm (parietal layer) Splanchnic mesoderm (visceral layer) Into: › Pericardial cavity › Pleural cavity › Peritoneal cavity Division achieved by: › Septum transversum › Paired pleuropericardial folds – superior to lungs › Paired pleuroperitoneal folds – inferior to lungs 4th week Bronchial budspericardioperitoneal canal – future pericardial cavity Pleural cavity expand – grow ventrally Common cardinal vein & Phrenic nerve raise ridge in lateral thoracic wall Pleural cavity grow in angle between body wall & ridge Result: › Mesenchyme of body wall split Outer layer – thoracic wall Inner layer – pleuropericardial membrane 7th week membrane – grow medially Pleuropericardial – fuse with › Each other › Mesenchyme ventral to oesophagus Separate pericardial from pleural cavity Right pleuropericardial opening close earlier › Right common cardinal vein larger – raise bigger fold Fused pleuropericardial membrane form FIBROUS PERICARDIUM Separate pleural from peritoneal cavity Lung & pleura invade body wall – strip mesoderm Ridge formed – caudal end of pericardioperitoneal canal Ridge- fold –cresentic free edgeproject into pericardioperitoneal canal Liver develop Fold become membranous 6th week Pleuroperitoneal membrane grow ventro – medially - fuse with: › Dorsal mesentry of oesophagus › Septum transversum Double layer of peritoneum enclosing a mass of mesoderm Connects the organ to the body wall Carries vessels, nerves & lymphatics for the organ Is the site where the visceral peritoneum continues as parietal peritoneum Transverse folding –medial walls of intra-embryonic coelon come together – mesentry Between layers – mesenchyme – B.V. & nerves Transiently divide I.E.Coelom into two halves Contain gut in them Transitory structure Limited to stomach & duodenum Gut suspended by it – mid plane Not in pharynx & upper oesophagus Given names– mesoesophagus…. Further development › Some parts specialized › Some – secondary attachment › Some disappear Heart tube invaginate pericardium from dorsal aspect Parietal & fibrous pericardium derived from somatopleuric mesoderm lining ventral side of pericardial cavity Visceral pericardium derived from splanchnopleuric mesoderm lining dorsal side of pericardium Heart tube suspended in pericardial cavity by dorsal mesocardium - disappears Communication – right & left side of pericardium – transverse pericardial sinus Four sources 1. Septum transversum 2. Pleuroperitoneal membranes 3. Dorsal mesentery of esophagus 4. Muscular ingrowth from lateral body walls 3rd week › Unsplit mesoderm › Cranial to cardiogenic mesoderm 4th week › Folding Septum transversum Caudal to pericardium Ventral to pericardioperitoneal canal Cranial part - diaphragm Caudal part › Liver › Ventral Mesentry Expand & fuse with pleuroperitoneal membrane Form central tendon 5th week Develop at caudal end of pericardioperitoneal canal Crescent fold - medially Fuse with: › Septum transversum › Dorsal mesentry oesophagus Myoblast from S.T. – pleuroperitoneal membrane Bulk of muscle form here Initially – median part Finally mesoesophagus condenses – L1 – L3 Two muscle bands › Myoblast grow in dorsal mesentry of esophagus Develop into Right & left crura 9th – 12th week Lungs & pleural cavity enlarge Burrow into body wall Mesenchyme split › External – abdominal wall › Internal – peripheral part of diaphragm Pleura extend further › Costodiapharagmatic recess › Dome shaped configuration 6th week : Three basic components: 1. Pleuroperitoneal membranes 2. Mesoesphagus 3. Septum transversum Fuse - form a complete partition between thoracic and abdominal cavities Septum transversum: Central tendon Pleuroperitoneal membranes: Form large portion of fetal diaphragm represent a smaller portion in infants Dorsal mesentery of esophagus: Crura Body wall: Peripheral muscular part • 4th week • Septum transversum opposite 3rd – 5th cervical somites • 5th week • Myoblasts from somites - developing diaphragm bringing their nerve fibers with them • Rapid growth of the body descent of diaphragm • 6th week the diaphragm level of the thoracic somites • End of 8th week diaphragm - level of first lumbar vertebra 4 parts of the diaphragm fuse Mesenchymal cells from the septum transversum - other three parts, Change into myoblasts -muscles of the diaphragm. Phrenic nerve supplies all the muscles of diaphragm Phrenic nerve - sensory to diaphram except peripheral region derived from the body wall and brings its nerve supply (lower intercostal nerves) with it Only common anomaly 1 in 2200 newborns Associated with CDH Inhibition of development & inflation of lung- breathing difficulties Lung hypoplasia – infant may die Severe lung hypoplasia – alveoli rupture – pneumothorax Polyhydramnios maybe present Cause: › Defective formation / fusion of pleuroperitoneal membrane with... Large opening in posterolateral part of diaphragm Peritoneal & pleural cavities communicate 85-90% on left side – foramen of Bochdalek Foramen closes at 6th wk. If open –viscera in thorax – lying Lungs & heart pushed anteriorly Most defects on left side – heart pushed to right Severity of lung development – extent of viscera in thorax – no room for development Treatment › Repair of defect – post natally › Lung achieve normal size Half of diaphragm – defective musculature – diaphragmatic pouch Superior displacement of viscera Cause: › Failure of muscular tissue from body wall to extend into pleuroperitoneal membrane Clinical manifestation – CDH Treatment: › Surgical repair Latissimus dorsi flap Prosthetic patch Herina – between xiphoid process & umbilicus Cause: › Failure of lateral body folds to fuse completely when forming anterior abdominal wall during folding Herniation of part of fetal stomach through excessively large esophageal hiatus May be a predisposing factor in adult acquired hiatal hernia Herniation through the sternocostal hiatus (foramen of Morgagni) – opening for superior epigastric B.V. Hiatus – between sternal & costal parts of diaphragm Herniation of: › Intestines into pericardial sac › Heart into peritoneal cavity Large defects associated with body wall defects Most often on right side Associated with lung hypoplasia & respiratory comlications Diagnosis: › MRI Treatment: › Surgical excision Double layer of peritoneum enclosing a mass of mesoderm Connects the organ to the body wall Carries vessels, nerves & lymphatics for the organ Is the site where the visceral peritoneum continues as parietal peritoneum