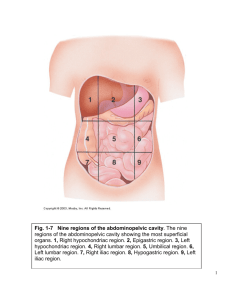
c h a p t e r 10 Body Cavities
advertisement

c h a p t e r 10 Body Cavities Formation of the Intraembryonic Cavity At the end of the third week, intraembryonic mesoderm on each side of the midline differentiates into a paraxial portion, an intermediate portion, and a lateral plate (Fig. 10.1A). When intercellular clefts appear in the lateral mesoderm, the plates are divided into two layers: the somatic mesoderm layer and the splanchnic mesoderm layer. The latter is continuous with mesoderm of the wall of the yolk sac (Fig. 10.1B). The space bordered by these layers forms the intraembryonic cavity (body cavity). At first the right and left sides of the intraembryonic cavity are in open connection with the extraembryonic cavity, but when the body of the embryo folds cephalocaudally and laterally, this connection is lost (Figs. 10.2, A–E). In this manner a large intraembryonic cavity extending from the thoracic to the pelvic region forms. CLINICAL CORRELATES Body Wall Defects Ventral body wall defects in the thorax or abdomen may involve the heart, abdominal viscera, and urogenital organs. They may be due to a failure of body folding, in which case one or more of the four folds 211 212 Part Two: Special Embryology Paraxial mesoderm Somatic mesoderm layer Intermediate mesoderm Intercellular clefts Lateral plate A Serous membrane Endoderm B Wall of amniotic cavity Splanchnic mesoderm layer Intraembryonic cavity Wall of yolk sac Figure 10.1 A. Transverse section through an embryo of approximately 19 days. Intercellular clefts are visible in the lateral plate mesoderm. B. Section through an embryo of approximately 20 days. The lateral plate is divided into somatic and splanchnic mesoderm layers that line the intraembryonic coelom. Tissue bordering the intraembryonic coelom differentiates into serous membranes. (cephalic, caudal, and two lateral) responsible for closing the ventral body wall at the umbilicus fail to progress to that region. Another cause of these defects is incomplete development of body wall structures, including muscle, bone, and skin. Cleft sternum is a ventral body wall defect that results from lack of fusion of the bilateral bars of mesoderm responsible for formation of this structure. In some cases the heart protrudes through a sternal defect (either cleft sternum or absence of the lower third of the sternum) and lies outside the body (ectopia cordis) (Fig. 10.3A). Sometimes the defect involves both the thorax and abdomen, creating a spectrum of abnormalities known as Cantrell pentalogy, which includes cleft sternum, ectopia cordis, omphalocele, diaphragmatic hernia (anterior portion), and congenital heart defects (ventricular septal defect, tetralogy of Fallot). Ectopia cordis defects appear to be due to a failure of progression of cephalic and lateral folds. Omphalocele (Fig. 10.3B) is herniation of abdominal viscera through an enlarged umbilical ring. The viscera, which may include liver, small and large intestines, stomach, spleen, or bladder, are covered by amnion. The origin of omphalocele is a failure of the bowel to return to the body cavity from its physiological herniation during the 6th to 10th weeks. Omphalocele, which occurs in 2.5/10,000 births, is associated with a high rate of mortality (25%) and severe malformations, such as cardiac anomalies (50%) and neural tube defects (40%). Chromosomal abnormalities are present in approximately 50% of liveborn infants with omphalocele. Gastroschisis (Fig. 10.3C ) is a herniation of abdominal contents through the body wall directly into the amniotic cavity. It occurs lateral to the umbilicus, Chapter 10: Body Cavities Amniotic cavity 213 Surface ectoderm Somatic mesoderm Splanchnic mesoderm Yolk sac A Connection between gut and yolk sac B Intraembryonic body cavity Dorsal Gut mesentery C Figure 10.2 Transverse sections through embryos at various stages of development. A. The intraembryonic cavity is in open communication with the extraembryonic cavity. B. The intraembryonic cavity is about to lose contact with the extraembryonic cavity. C. At the end of the fourth week, splanchnic mesoderm layers are continuous with somatic layers as a double-layered membrane, the dorsal mesentery. Dorsal mesentery extends from the caudal limit of the foregut to the end of the hindgut. D and E. Scanning electron micrographs of sections through mouse embryos showing details similar to those in B and C, respectively. G, Gut tube; arrowheads, splanchnic mesoderm; C, body cavity; arrow, dorsal mesentery; A, dorsal aorta; NT, neural tube. usually on the right, through a region weakened by regression of the right umbilical vein, which normally disappears. Viscera are not covered by peritoneum or amnion, and the bowel may be damaged by exposure to amniotic fluid. Both omphalocele and gastroschisis result in elevated levels of α-fetoprotein in the amniotic fluid, which can be detected prenatally. 214 Part Two: Special Embryology Heart A B C D Figure 10.3 Ventral body wall defects. A. Infant with ectopia cordis. Mesoderm of the sternum has failed to fuse, and the heart lies outside of the body. B. Omphalocele with failure of the intestinal loops to return to the body cavity following physiological herniation. The herniated loops are covered by amnion. C. Omphalocele in a newborn. D. A newborn with gastroschisis. Loops of bowel return to the body cavity but herniate again through the body wall, usually to the right of the umbilicus in the region of the regressing right umbilical vein. Unlike omphalocele, the defect is not covered by amnion. Chapter 10: Body Cavities 215 Lung bud Pleuropericardial fold Phrenic nerve C Heart Common cardinal vein Figure 10.4 A. Scanning electron micrograph showing the ventral view of a mouse embryo (equivalent to approximately the fourth week in human development). The gut tube is closing, the anterior and posterior intestinal portals are visible (arrowheads), and the heart (H) lies in the primitive pleuropericardial cavity (asterisks), which is partially separated from the abdominal cavity by the septum transversum (arrow). B. Portion of an embryo at approximately 5 weeks with parts of the body wall and septum transversum removed to show the pericardioperitoneal canals. Note the size and thickness of the septum transversum and liver cords penetrating the septum. C. Growth of the lung buds into the pericardioperitoneal canals. Note the pleuropericardial folds. 216 Part Two: Special Embryology Gastroschisis occurs in 1/10,000 births but is increasing in frequency, especially among young women, and this increase may be related to cocaine use. Unlike omphalocele, gastroschisis is not associated with chromosome abnormalities or other severe defects. Therefore the survival rate is excellent, although volvulus (rotation of the bowel) resulting in a compromised blood supply may kill large regions of the intestine and lead to fetal death. Serous Membranes Cells of the somatic mesoderm lining the intraembryonic cavity become mesothelial and form the parietal layer of the serous membranes lining the outside of the peritoneal, pleural, and pericardial cavities. In a similar manner, cells of the splanchnic mesoderm layer form the visceral layer of the serous membranes covering the abdominal organs, lungs, and heart (Fig. 10.1). Visceral and parietal layers are continuous with each other as the dorsal mesentery (Fig. 10.2, C and E ), which suspends the gut tube in the peritoneal cavity. Initially this dorsal mesentery is a thick band of mesoderm running continuously from the caudal limit of the foregut to the end of the hindgut. Ventral mesentery exists only from the caudal foregut to the upper portion of the duodenum and results from thinning of mesoderm of the septum transversum (see Chapter 13). These mesenteries are double layers of peritoneum that provide a pathway for blood vessels, nerves, and lymphatics to the organs. Diaphragm and Thoracic Cavity The septum transversum is a thick plate of mesodermal tissue occupying the space between the thoracic cavity and the stalk of the yolk sac (Fig. 10.4, A and B). This septum does not separate the thoracic and abdominal cavities completely but leaves large openings, the pericardioperitoneal canals, on each side of the foregut (Fig. 10.4B). When lung buds begin to grow, they expand caudolaterally within the pericardioperitoneal canals (Fig. 10.4C ). As a result of the rapid growth of the lungs, the pericardioperitoneal canals become too small, and the lungs begin to expand into the mesenchyme of the body wall dorsally, laterally, and ventrally (Fig. 10.4C ). Ventral and lateral expansion is posterior to the pleuropericardial folds. At first these folds appear as small ridges projecting into the primitive undivided thoracic cavity (Fig. 10.4C ). With expansion of the lungs, mesoderm of the body wall splits into two components (Fig. 10.5): (a) the definitive wall of the thorax and (b) the pleuropericardial membranes, which are extensions of the pleuropericardial folds that contain the common cardinal veins and phrenic nerves. Subsequently, descent of the heart and positional changes of Chapter 10: Body Cavities Primitive pleural cavity 217 Superior vena cava Parietal pleura Parietal pleura Lung Visceral pleura Pleural cavity Fibrous pericardium Pleuropericardial membrane Phrenic nerve Pericardial cavity A B Figure 10.5 A. Transformation of the pericardioperitoneal canals into the pleural cavities and formation of the pleuropericardial membranes. Note the pleuropericardial folds containing the common cardinal vein and phrenic nerve. Mesenchyme of the body wall splits into the pleuropericardial membranes and definitive body wall. B. The thorax after fusion of the pleuropericardial folds with each other and with the root of the lungs. Note the position of the phrenic nerve, now in the fibrous pericardium. The right common cardinal vein has developed into the superior vena cava. the sinus venosus shift the common cardinal veins toward the midline, and the pleuropericardial membranes are drawn out in mesentery-like fashion (Fig. 10.5A). Finally, they fuse with each other and with the root of the lungs, and the thoracic cavity is divided into the definitive pericardial cavity and two pleural cavities (Fig. 10.5B). In the adult, the pleuropericardial membranes form the fibrous pericardium. Formation of the Diaphragm Although the pleural cavities are separate from the pericardial cavity, they remain in open communication with the abdominal (peritoneal) cavity, since the diaphragm is incomplete. During further development, the opening between the prospective pleural and peritoneal cavities is closed by crescent-shaped folds, the pleuroperitoneal folds, which project into the caudal end of the pericardioperitoneal canals (Fig. 10.6A). Gradually the folds extend medially and ventrally so that by the seventh week they fuse with the mesentery of the esophagus and with the septum transversum (Fig. 10.6B). Hence the connection between the pleural and peritoneal portions of the body cavity is closed by the pleuroperitoneal membranes. Further expansion of the pleural cavities relative to mesenchyme of the body wall adds a peripheral rim to the pleuroperitoneal membranes (Fig. 10.6C ). Once this rim is established, myoblasts 218 Part Two: Special Embryology Pericardioperitoneal Pleuroperitoneal fold Esophagus mesentery Aorta Pleuroperitoneal membrane Esophagus canal A B Septum transversum Inferior vena cava C Muscular ingrowth from body wall Septum transversum Figure 10.6 Development of the diaphragm. A. Pleuroperitoneal folds appear at the beginning of the fifth week. B. Pleuroperitoneal folds fuse with the septum transversum and mesentery of the esophagus in the seventh week, separating the thoracic cavity from the abdominal cavity. C. Transverse section at the fourth month of development. An additional rim derived from the body wall forms the most peripheral part of the diaphragm. originating in the body wall penetrate the membranes to form the muscular part of the diaphragm. Thus the diaphragm is derived from the following structures: (a) the septum transversum, which forms the central tendon of the diaphragm; (b) the two pleuroperitoneal membranes; (c) muscular components from the lateral and dorsal body walls; and (d) the mesentery of the esophagus, in which the crura of the diaphragm develop (Fig. 10.6C ). Initially the septum transversum lies opposite cervical somites, and nerve components of the third, fourth, and fifth cervical segments of the spinal cord grow into the septum. At first the nerves, known as phrenic nerves, pass into the septum through the pleuropericardial folds (Fig. 10.4B). This explains why further expansion of the lungs and descent of the septum shift the phrenic nerves that innervate the diaphragm into the fibrous pericardium (Fig. 10.5). Although the septum transversum lies opposite cervical segments during the fourth week, by the sixth week the developing diaphragm is at the level of thoracic somites. The repositioning of the diaphragm is caused by rapid growth of the dorsal part of the embryo (vertebral column), compared with that of the ventral part. By the beginning of the third month some of the dorsal bands of the diaphragm originate at the level of the first lumbar vertebra. The phrenic nerves supply the diaphragm with its motor and sensory innervation. Since the most peripheral part of the diaphragm is derived from mesenchyme of the thoracic wall, it is generally accepted that some of the lower intercostal (thoracic) nerves contribute sensory fibers to the peripheral part of the diaphragm. Chapter 10: Body Cavities 219 CLINICAL CORRELATES Diaphragmatic Hernias A congenital diaphragmatic hernia, one of the more common malformations in the newborn (1/2000), is most frequently caused by failure of one or both of the pleuroperitoneal membranes to close the pericardioperitoneal canals. In that case the peritoneal and pleural cavities are continuous with one another along the posterior body wall. This hernia allows abdominal viscera to enter the pleural cavity. In 85 to 90% of cases the hernia is on the left side, and intestinal loops, stomach, spleen, and part of the liver may enter the thoracic cavity (Fig. 10.7). The abdominal viscera in the chest push the heart anteriorly and compress the lungs, which are commonly hypoplastic. A large defect is associated with a high rate of mortality (75%) from pulmonary hypoplasia and dysfunction. Occasionally a small part of the muscular fibers of the diaphragm fails to develop, and a hernia may remain undiscovered until the child is several years old. Such a defect, frequently seen in the anterior portion of the diaphragm, is a parasternal hernia. A small peritoneal sac containing intestinal loops may enter the chest between the sternal and costal portions of the diaphragm (Fig. 10.7A). Another type of diaphragmatic hernia, esophageal hernia, is thought to be due to congenital shortness of the esophagus. Upper portions of the stomach are retained in the thorax, and the stomach is constricted at the level of the diaphragm. SUMMARY At the end of the third week, intercellular clefts appear in the mesoderm on each side of the midline. When these spaces fuse, the intraembryonic cavity (body cavity), bordered by a somatic mesoderm and a splanchnic mesoderm layer, is formed (Figs. 10.1 and 10.2). With cephalocaudal and lateral folding of the embryo, the intraembryonic cavity extends from the thoracic to the pelvic region. Somatic mesoderm will form the parietal layer of the serous membranes lining the outside of the peritoneal, pleural, and pericardial cavities. The splanchnic layer will form the visceral layer of the serous membranes covering the lungs, heart, and abdominal organs. These layers are continuous at the root of these organs in their cavities (as if a finger were stuck into a balloon, with the layer surrounding the finger being the splanchnic or visceral layer and the rest of the balloon, the somatic or parietal layer surrounding the body cavity). The serous membranes in the abdomen are called peritoneum. The diaphragm divides the body cavity into the thoracic and peritoneal cavities. It develops from four components: (a) septum transversum (central tendon); (b) pleuroperitoneal membranes; (c) dorsal mesentery of the esophagus; and (d) muscular components of the body wall (Fig. 10.6). Congenital 220 Part Two: Special Embryology Opening between sternal and costal heads Inferior vena cava Central tendon Opening for esophagus Left lung Colon Aortic hiatus A Absence of pleuroperitoneal membrane Diaphragm Stomach B C Figure 10.7 Congenital diaphragmatic hernia. A. Abdominal surface of the diaphragm showing a large defect of the pleuroperitoneal membrane. B. Hernia of the intestinal loops and part of the stomach into the left pleural cavity. The heart and mediastinum are frequently pushed to the right and the left lung compressed. C. Radiograph of a newborn with a large defect in the left side of the diaphragm. Abdominal viscera have entered the thorax through the defect. Chapter 10: Body Cavities 221 diaphragmatic hernias involving a defect of the pleuroperitoneal membrane on the left side occur frequently. The thoracic cavity is divided into the pericardial cavity and two pleural cavities for the lungs by the pleuropericardial membranes (Fig. 10.5). Double layers of peritoneum form mesenteries that suspend the gut tube and provide a pathway for vessels, nerves, and lymphatics to the organs. Initially, the gut tube from the caudal end of the foregut to the end of the hindgut is suspended from the dorsal body wall by dorsal mesentery (Fig. 10.2, C and E ). Ventral mesentery derived from the septum transversum exists only in the region of the terminal part of the esophagus, the stomach, and upper portion of the duodenum (see Chapter 13). Problems to Solve 1. A newborn infant cannot breathe and soon dies. An autopsy reveals a large diaphragmatic defect on the left side, with the stomach and intestines occupying the left side of the thorax. Both lungs are severely hypoplastic. What is the embryological basis for this defect? 2. A child is born with a large defect lateral to the umbilicus. Most of the large and the small bowel protrude through the defect and are not covered by amnion. What is the embryological basis for this abnormality, and should you be concerned that other malformations may be present? SUGGESTED READING Cunniff C, Jones KL, Jones MC: Patterns of malformations in children with congenital diaphragmatic defects. J Pediatr 116:258, 1990. Puri P, Gormak F: Lethal nonpulmonary anomalies associated with congenital diaphragmatic hernia: implications for early intrauterine surgery. J Pediatr Surg 35:29, 1984. Skandalakis JE, Gray SW: Embryology for Surgeons: The Embryological Basis for the Treatment of Congenital Anomalies. 2nd ed. Baltimore, Williams & Wilkins, 1994.