Head and Neck Cancer - St. John Providence
advertisement
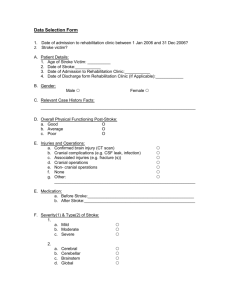
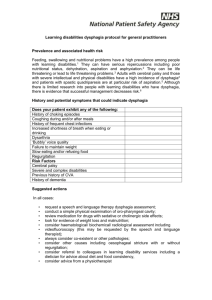
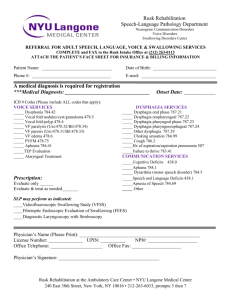
Head and Neck Cancer: The Impact of Speech Language Pathology on Quality of Life Presented by: Autumn Bjornstad, MA, CCC-SLP Learning Objectives • By the end of this presentation, the listener will: – Identify three quality of life (QOL) benefits to the involvement of speech language pathology in the care of patients with head and neck cancer. – Identify the most effective timing of dysphagia treatment in this population. Birthdays Graduations Promotions Weddings Anniversaries Holidays Quality of Life • Common themes: – Food – Drink – Words to celebrate – singing happy birthday, reciting vows, speeches, toasting the newlyweds, prayers at family meals Speech Language Pathology Role • American Speech Language Hearing Association’s (ASHA) Scope of Practice (2007) outlines the role of a speech pathologist as: – “the professional who engages in clinical services, prevention, advocacy, education, administration, and research in the areas of communication and swallowing across the life span from infancy through geriatrics” – Clinical services include the assessment, treatment and collaboration with other professionals in the areas of swallowing, speech, language and voice. Quality of Life Indicators • Major themes in the literature for measures of QOL after treatment for headneck cancer include: – Swallowing • Dysphagia – Speech Intelligibility/Communication • Dysarthria • Voice: Aphonia/Dysphonia/Alaryngeal speech Dysphagia • Standard of care: – Assessment of swallow function pre-treatment to determine baseline – Providing prophylactic treatment (Carroll, Locher, Canon, Bohannon, McColloch & Magnuson, 2008) – Ongoing assessment and treatment of dysphagia during and post radiation, chemoradiation or surgical intervention (Rosenthal, Lewin, & Eisbruch 2006) – Primary Goal: Keep the swallow moving and avoid any prolonged NPO periods for the best long term swallowing outcome (Gellespie, 2004) Dysphagia Assessment • Assessment of dysphagia is best completed with a combination of tools including objective measures (videoswallow or modified barium swallow) and more subjective QOL measures • Use of QOL tools that assess emotional and social aspects of dysphagia – M. D. Anderson Dysphagia Inventory (MDADI): was studied and found to be a reliable and validated questionnaire with the purpose to assess dysphagia effects on the QOL of patients with head and neck cancer. It includes global, emotional, functional, and physical subscales in relation to dysphagia. • • – (Chen, Frankowski, Bishop-Leone, Herbert, Leyk, Lwein, & Goepfert, 2001) (Gellespie, Brodsky, Day, Lee, & Martin-Harris, 2004) Gellespie (2004) states that diet texture alone is not an adequate measure of dysphagia severity and impact on QOL • Though 88% of patients in the study were on a normal or soft solid diet at least 1 year post treatment of stage III or IV squamous cell carcinoma of the oropharynx, larynx and hypopharynx, only 10% of these patients scored within the area of normal or mild impairment on the MDADI • Many of these patients were found to continue with a soft diet despite significant difficulties in effort needed to swallow, increased time to eat, s/s aspiration, avoidance of social situations involving eating, and weight loss due to dysphagia • These patients despite being on a reasonably normal textured diet may still benefit from dysphagia therapy to make eating more comfortable, enjoyable and safe Dysphagia Assessment • Rosenthal (2006) – Found that patients often have poor perception of dysphagia and under-report difficulty. This can contribute to more long term/chronic swallowing impairments and supports the importance of videofluoroscopic studies pre- and post- radiation and chemo/radiation to accurately document swallow function • Kendell, Kosek & Tanner (2014) – Also highlight the importance of objective measures of swallowing function in assessment and treatment – Study compared quality of life scores to objective measures of swallowing after chemo/radiation: Findings indicate that a combination of subjective measures (QOL tools, bedside swallow assessments) as well as objective studies (videoswallow, modified barium, FEES) , pre, during and post treatment is the most effective way to accurately evaluate and treat dysphagia and reduce long term swallowing deficits Prophylactic Treatment Swallow (Eat/Drink) Use it or lose it! Exercise (Hutchenson, 2012) Prophylactic Treatment • Kulbersh, Rosenthal, McGrew, Duncan, McColloch, Carroll & Magnuson (2006) – – – • State that post-tx (radiation or chemoradiation) dysphagia occurs in 50-60% of patients Dysphagia treatment in this study included swallowing education and initiation of a home exercise program 5x/day. Exercises began 2 wks pre-treatment (focusing on hylolaryngeal excursion, tongue base retraction, vocal fold closure, UES opening), with follow up 2 wks into treatment, 6 wks into treatment and then 6+ months post tx A group of 37 patients were studied undergoing primary radiation or chemoradiation. The group receiving pre-treatement therapy for dysphagia showed a statistically significant improvement on dysphagia QOL measurements in areas of physical, emotional and global. This was in comparison to a control group which received dysphagia therapy after radiation or chemoradiation was initiated. Carroll (2008) – – Study showed improved swallow function 3 months after completion of chemoradiation in group receiving dysphagia therapy and exercises prior to initiation of tx for advanced squamous cell carcinoma of the oropharynx, hypopharynx, and larynx, compared to control group receiving only post treatment dysphagia therapy. Improved outcomes in areas of epiglottic inversion and tongue base retraction for the pretreatment swallowing therapy group Prophylactic Treatment • Rosenthal, Lewin & Eisbruch (2006) – – Reported that early speech therapy intervention (prior to radiation treatment) focusing on ROM maintenance, strength and precision of movement is the best indicator of safe, functional post treatment swallowing. Recovery of swallow function 6 months post tx most indicative of long term swallowing function • Barbon & Steele (2014) found that the temporary use of postural changes and thickened liquids can reduce aspiration during the course of treatment for head and neck cancer • The take home message in the literature is that the sooner the dysphagia treatment is initiated the better the overall outcome for swallowing both subjectively by the patients and objectively via videofluoroscopy. Passy Muir Speaking Valve (PMSV) • Even for temporary tracheostomy, PMSV can improve quality of life during hospital stay and in the home environment . – Facilitates better communication with family, staff and provides a sense of normalcy to be able to use “voice” to communicate. – Provides more functional/sustainable voice compared to a fenestrated trach tube alone – Other benefits include improved sensation for secretion management and swallowing, as well as reduction of aspiration (Dettelbach, Gross, Mahlmann, & Eibling, 1995) – Contraindicated if tumor or swelling is causing upper airway obstruction • These benefits, in turn, have a positive impact on QOL Dysarthria • Though it may seem like common sense to slow your speech rate, increase loudness, reduce background noises, use context, support speech with gestures; when speech is less intelligible, patients often need to be educated regarding these compensatory strategies, environment modifications, guided through a hierarchy, provided with feedback and supported to obtain the best possible results (Yorkston, Strand & Kennedy, 1996) • A study in 1998 found decreased tongue mobility and speech intelligibility post operatively after intraoral tumor resection with flap repair. The severity of speech deficit was directly related to the post-op quality of life reported by patients on the functional living cancer index. – – • If the speech was minimally effected, improved QOL was seen post op, while no improvement was reported for those with a substantial reduction in intelligibility. (Shliephake, Schmelzeisen, Schonweiler, Schneller, & Alternbernd, 1998) For patients s/p total glossectomy or with presence of other severe post-surgical dysarthria, text to speech apps on smartphones can be trained in addition to use of Alternative & Augmentative Communication (AAC) devices. Speech sound approximations can also be trained to increase intelligibility. – – – Furia, Kowalski, Latorre, Angelis, Martins, Barros, & Ribiero (2001) Rodriguez & Rowe (2010) Happ, Roesch, & Kagan (2005) Laryngectomy • Pre-Operative Counseling/Education: – – • Alaryngeal speech – – – • Meet and greet, provide general education regarding anatomy changes, post surgical alaryngeal speech options and expectations, as well as dysphagia Zeine & Larson (1999) found that up to 21% of patients/spouses surveyed reported they were unaware that the laryngectomy surgery would result in loss of voice Electrolarynx – immediate gratification post-op TEP – primary or secondary Esophageal Speech Dysphagia – – Compenstory strategies for dysphagia, xerostomia, lack of taste, etc Screen for dysphagia or strictures • • – Often need to ask the right questions: Instead of “Do you have any trouble swallowing?” ask other probing questions such as “Do foods stick or come back up after you eat or drink?”, “Do you avoid eating in public?”, “What types of food do you avoid?” Medical management of strictures, GERD, etc are going to be more successful if caught and treated early on Patient education Knowledge is Power • To improve quality of life in regards to speech and swallowing, education may be one of the most powerful tools we can provide to our patients with head and neck cancer. • It allows them to be proactive in their own care and be best prepared for inevitable changes and fluctuations in speech/swallowing, as well as understand the importance of early intervention and compensation to achieve the best possible outcomes. In Closing • Speech Language Pathology services can improve the QOL of patients with head and neck cancer through proper evaluation and treatment of dysphagia, dysarthria, voice impairments, use of speaking valves, training alaryngeal speech and educating and empowering the patient and family. Thank You! References • • • • • • • • • • American Speech-Language-Hearing Association. (2007). Scope of practice in speech-language pathology [Scope of Practice]. http://www.asha.org/policy/SP2007-00283/, Retrieved on March 19th 2015 Barbon, C. E., & Steele, C. M. (2014). Efficacy of thickened liquids for eliminating aspiration in head and neck cancer a systematic review. Otolaryngology--Head and Neck Surgery, 0194599814556239. Carroll, W. R., Locher, J. L., Canon, C. L., Bohannon, I. A., McColloch, N. L., & Magnuson, J. S. (2008). Pretreatment swallowing exercises improve swallow function after chemoradiation. The Laryngoscope, 118(1), 39-43. Chen, A. Y., Frankowski, R., Bishop-Leone, J., Hebert, T., Leyk, S., Lewin, J., & Goepfert, H. (2001). The development and validation of a dysphagia-specific quality-of-life questionnaire for patients with head and neck cancer: the MD Anderson dysphagia inventory. Archives of Otolaryngology–Head & Neck Surgery, 127(7), 870-876. Dettelbach, M. A., Gross, R. D., Mahlmann, J., & Eibling, D. E. (1995). Effect of the passy‐muir valve on aspiration in patients with tracheostomy. Head & Neck, 17(4), 297-302. Furia, C. L., Kowalski, L. P., Latorre, M. R., Angelis, E. C., Martins, N. M., Barros, A. P., & Ribeiro, K. C. (2001). Speech intelligibility after glossectomy and speech rehabilitation. Archives of Otolaryngology–Head & Neck Surgery, 127(7), 877-883 Gillespie, M. B., Brodsky, M. B., Day, T. A., Lee, F. S., & Martin‐Harris, B. (2004). Swallowing‐related quality of life after head and neck cancer treatment. The Laryngoscope, 114(8), 1362-1367. Happ, M. B., Roesch, T. K., & Kagan, S. H. (2005, November). Patient communication following head and neck cancer surgery: A pilot study using electronic speech-generating devices. In Oncology Nursing Forum (Vol. 32, No. 6, pp. 1179-1187). Oncology Nursing Society. Hutcheson, K. (2012, Sept). Introduction to normal swallow & application to H&N cancer radiotherapy. Powerpoint. American Assoc Medical Dosimetrists Region Meeting. Retrieved March 19th, 2015. http://www.medicaldosimetry.org/pub/39816b99-2354-d714-5159-a6ab9f5085d1 Kendall, K. A., Kosek, S. R., & Tanner, K. (2014). Quality‐of‐life scores compared to objective measures of swallowing after oropharyngeal chemoradiation. The Laryngoscope, 124(3), 682-687 References Continued • • • • • • • • • Kulbersh, B. D., Rosenthal, E. L., McGrew, B. M., Duncan, R. D., McColloch, N. L., Carroll, W. R., & Magnuson, J. S. (2006). Pretreatment, preoperative swallowing exercises may improve dysphagia quality of life. The Laryngoscope, 116(6), 883-886. Markkanen‐Leppänen, M., Mäkitie, A. A., Haapanen, M. L., Suominen, E., & Asko‐Seljavaara, S. (2006). Quality of life after free‐flap reconstruction in patients with oral and pharyngeal cancer. Head & Neck, 28(3), 210-216. McDonough, E. M., Varvares, M. A., Dunphy, F. R., Dunleavy, T., Dunphy, C. H., & Boyd, J. H. (1996). Changes in quality‐of‐life scores in a population of patients treated for squamous cell carcinoma of the head and neck. Head & Neck, 18(6), 487-493. Rodriguez, C., & Rowe, M. (2010, March). Use of a speech-generating device for hospitalized postoperative patients with head and neck cancer experiencing speechlessness. In Oncology Nursing Forum (Vol. 37, No. 2, pp. 199-205). Oncology Nursing Society. Rosenthal, D. I., Lewin, J. S., & Eisbruch, A. (2006). Prevention and treatment of dysphagia and aspiration after chemoradiation for head and neck cancer. Journal of Clinical Oncology, 24(17), 26362643 Schliephake, H., Schmelzeisen, R., Schönweiler, R., Schneller, T., & Altenbernd, C. (1998). Speech, deglutition and life quality after intraoral tumour resection: A prospective study. International Journal of Oral and Maxillofacial Surgery, 27(2), 99-105. Sullivan, M., Gaebler, C., Ball, L.. (November 11, 2007). Supporting Persons with Chronic Communication Limitations: Head & Neck Cancer ASHA Convention, Boston 11/17/2007 © Retrieved March 23, 2015, from www.asha.org/Events/convention/handouts/2007/2011_Sullivan_Marsha. Yorkston, K. M., Strand, E. A., & Kennedy, M. R. (1996). Comprehensibility of dysarthric speech implications for assessment and treatment planning. American Journal of Speech-Language Pathology, 5(1), 55-66 Zeine, L., & Larson, M. (1999). Pre-and post-operative counseling for laryngectomees and their spouses: an update. Journal of Communication Disorders, 32(1), 51-71.


![Dysphagia Webinar, May, 2013[2]](http://s2.studylib.net/store/data/005382560_1-ff5244e89815170fde8b3f907df8b381-300x300.png)