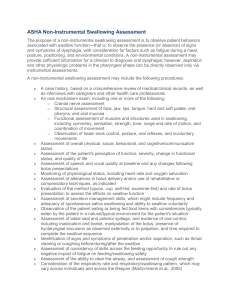
Dysphagia Webinar, May, 2013[2]
advertisement
![Dysphagia Webinar, May, 2013[2]](http://s2.studylib.net/store/data/005382560_1-ff5244e89815170fde8b3f907df8b381-768x994.png)
Dysphagia and Diet for People with Traumatic Brain Injury Robert Trombley, Registered Dietitian Barbara Goodman, Speech/Language Pathologist It can happen on any given day From this: To this: Objective Define basic dysphagia terms and diagnostic tests Understand dysphagia recommendations and diet modifications Identify best-practices Recognize potential pitfalls Strategies for compliance 3 Unique and Lifelong Experience 4 5 How often does dysphagia occur and who does it affect? Statistics in the incidence of dysphagia in the traumatic brain injury individual vary widely; one study reporting 80% effected and 16% needing assistance with eating one year post injury (Duong, Englaneder, Wright, Cifi, Greenwald and Brown, 2004) Dysphagia prevalence increases with age, therefore, people with a TBI may acquire dysphagia as they age. 61% of adults admitted to acute trauma centers 41% of individuals in rehab settings 30% - 75% of patients in nursing homes 10 million Americans (adults and children) are evaluated each year with swallowing difficulties ASHA, Communication Facts: Special Populations: Dysphagia- 2008 Edition, compiled by Andrea Castrogiovannirder 6 Definition: Dysphagia is defined as a difficulty in swallowing. This includes any difficulty in the process of: biting, chewing, handling and/or swallowing of food and/or liquid. One example of a swallowing problem that we can all relate to is when food or drink “goes down the wrong way”, which we all have experienced at one time or another. For people with dysphagia, this problem is occurring more frequently. 7 Swallowing: The Delicate Ballet 8 9 The Normal Swallow 10 http://www.radionz.co.nz/national/programm es/ourchangingworld 11 People with traumatic brain injury may have damaged the cranial nerves and/or have structural abnormalities (to their jaw, neck, throat) affecting swallowing. Symptoms: Coughing Throat clearing Hunching of shoulders Sensation of food getting caught Reddening in the face and/or facial grimacing Pain with swallowing Vomiting Wet voice Slow eating - fatigue Holding food in mouth Refusal to eat Weight loss, dehydration Heartburn or Reflux Upper respiratory infections and/or pneumonia Choking 12 Stages of Swallowing: Stage One: Oral Phase Includes oral preparatory phase Mastication (chewing) of the food Forms a bolus (mass of soft chewed food) Bolus moves to the back of the oral cavity into the oropharynx (throat) Takes approx. one second Common problems: difficulty in chewing, forming a bolus, controlling the bolus, propelling the bolus to pharynx 13 Stage Two: Pharyngeal Tongue pushes food to pharynx, which triggers swallowing response. Larynx and epiglottis move to close off the airway for protection, breathing stops. Reflexive, lasting one second or less. Common problems: delayed swallow, nasal regurgitation, inadequate protection of the airway, pharyngeal stasis 14 Stage Three: Esophageal The bolus enters the esophagus and travels to the stomach Reflexive, takes approx. 3 seconds, may take longer for pill (medication) Common problems: poor peristalsis, obstructions Diagnostic Tools Flexible Endoscopic Evaluation of Swallowing (FEES) 15 Modified Barium Swallow Study (MBS) or Videofluoroscopic Swallow Study (VDSS) Modified Barium Swallow (MBS) 16 Recommendations: Diet modifications Compensatory and/or Facilitation Strategies 17 18 19 1. Prepare for the MBS (if possible attend)- how is the person eating and drinking nowWhat is working for them and what seems to be causing problems: Symptoms Types of food or drink that work best or worse Positioning Pace of eating and drinking Bring to the MBS small sample of a simple favorite food (sandwich, pizza) 2. After the speech pathologist makes the diet recommendations: Ask, ask, ask questions What is a thickened liquid? Where do I get these thickening agents? What is a soft mechanical food? What is the best position for the person to eat? To drink? What does a chin tuck look like? How much food is a normal bite? A normal sip of a drink? How do I give medications? Will direct speech therapy help? 20 A Modified and Thickened WHAT???? Published 2002 NDDTF ‒ Academy of Nutrition and Dietetics ‒ American Speech-Language and Hearing Association Thickened liquids Dietary textures Standard of treatment Great guide for general recommendations for food at the different levels 21 22 Primary Food Consistencies Regular – Level 4 Chopped – Level 3 Mechanical Soft – Level 2 Puree – Level 1 Primary Liquid Consistencies Thin Nectar Honey Pudding Nectar Thick Honey Thick Denial and Confusion “There is no problem.” “Who says I have trouble eating and drinking?” “Why am I eating this?” Provide clear, simple and consistent language Make sure that everyone is on the same page Do not argue, accept that this is their perspective, but do follow diet recommendations Provide praise for any positive action Be patient 25 Judgement and Memory Taking excessively large bites or sips Eating very quickly Unable to remember strategies Precut food Pre-teach Verbal reminders Visual/auditory reminders- pictures, clock Special cups, silverware, plates 26 Adverse health outcomes Weight loss Dehydration Malnutrition Respiratory illness Pneumonia Upper respiratory infection Bronchitis The yuck factor or Lost passion for food 28 Gaining Acceptance Increasing Compliance What was that! RIGHT ON! Gaining Acceptance Increasing Compliance • • • • • Aroma Seasoning Layering/Swirling Piping Molds TASTE IT Kitchen Essentials Appliances and small wares Kitchen Essentials Food thickeners Kitchen Essentials Liquid thickeners Powders Gells Preparation Tips Proteins Marinating Acid-based marinades Braised Stewed Easier to prepare cold Proteins molecules tighten when heated Braising and stewing tenderizes the connective tissue Never use water Stocks, Gravies Fats/oils, Mayonnaise Milk/Cream Preparation Tips Starches Rice Pasta, Noodles, Macaroni Potatoes Beans Preparation Tips Fruits & Vegetables Skins Stringy Woody Seeds Dried fruits Apples Grapes Pineapple Asparagus Broccoli stalks Carrots Celery Raisins Go from fear and confusion…. To confidence and success Successful Functional Outcomes: Compliance Satisfaction Limited level of distress-both the caregiver and the TBI individual Good health 40