Document
advertisement

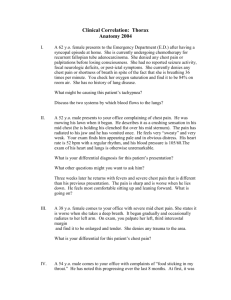
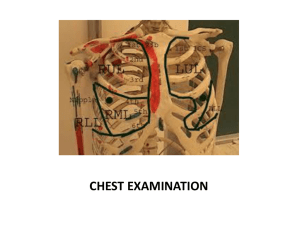
Respiratory assessment DR---Noha Elsayed 2015--2016 Respiratory assessment Inspection of respiratory system • Inspection (visual examination of chest)includes:1. Mental status. 2. Skin color and temperature , evidence of trauma &congenital anomalies . 3. Shape of chest wall …..barrel chest (↑A.P diameter). 4. Presence of an artificial airway (end tracheal or tracheostomy tube). 5. Breathing spontaneously or need for mechanical ventilation. 6. Equal chest expansion with each breath. 7. Use of accessory muscles such as scalene, sternocleidomastoid , intercostals and nasal flaring . 8. Work of breathing (labored or unlabored) 9. Presence of chest tubes, central lines and dressings 10.Presence of signs of injury (such as bruising, laceration and penetrating wounds) palpation 1. Give information about skin and subcutaneous tissues • Is there crackling???(Presence of S.C emphysema → Escaping air from pleural space from ruptured bleb dissecting through S.C tissues) ↙ Small amount in normal variant (Insertion of chest tube) ↘ Critically ill patients (Requires mechanical ventilation) 2. Palpation of trachea for alignment: Deviated trachea indicates the presence of a solid tumor (Trachea moves away from the tumor) or pneumothorax (Trachea moves towards affected lung in simple pneumothorax but away in tension pneumothorax) N.B.Remember: Trachea deviates to the area of least resistance 3. Palpation of chest wall for bilateral chest expansion Should be equal, symmetrical, bilateral A good method of determining this is to look at the patient while standing at the patient’s feet rather than at the side Palpation • Subcutaneous emphysema – “Snap, crackle, pop” sensation – Benign, but cause may be life threatening • Vocal fremitus – Assessed when performing tactile fremitus – Increase indicates underlying lung tissue more solid, contains less air than normal Percussion of chest • The technique of percussion is performed using one or two hands • One handed technique involves using index and middle fingers to strike the skin over the lung fields • Two handed technique strike skin with index finger of free hand as it sits over the lung field to be examined Compare the percussion notes in the same intercostal space in both sides. Percussion is performed from the apex to the base of both lungs. Normal lung is resonant Dullness )consolidation (as pneumonia &solid tissue (tumor) or fluid in the lung. Hyper resonance with pneumothorax. Auscultation (Assessing Breath Sounds) During the physical exam, auscultation of breath sounds may provide additional evidence of breathing difficulty. It can be auscultated across the anterior &posterior chest walls and medially at mid axillary line with a stethoscope. We must compare one side of chest wall with the opposite side Assessing the adventitious breath sounds Expiration normally twice as long as inspiration; I:E ratio is 1:2 Adventitious )Added) breath sounds abnormal sounds that are heard over a patient's lungs and airways 1. Crackles …. ) discontinuous sounds (Indicates air passing over fluid in small airways (Atelectasis or fluid congestion) 2. Rhonchi …. ) low-pitched (Air moving through large air ways containing secretions 3. Wheezing …. ) high-pitched (Air moving through narrowed airway ↙ ↘ Inspiratory Expiratory (In upper air way obstruction) (In asthma) 4. Stridor) seal bark( loud, high-pitched, heard during inspiration 5. Pleural friction rub: surfaces of visceral and parietal pleura rub together http://www.easyauscultation.com/adventitious-breath-sounds http://www.easyauscultation.com/lung-sounds 1. Current ventilator settings & parameters. 2. Baseline arterial blood gas measurements)ABG). 3. Adjustment of inspired O2 levels to maintain saturation between 94% & 98%. Pulse-oximeter Noninvasive way to measure the hemoglobin with oxygen attached Oxygen saturation over 95% = normal percentage of Pulse Oximetry • Used for: – Monitoring oxygenation status during intubation attempt or suctioning – Identifying deterioration in a patient with trauma or cardiac disease – Identifying high-risk patients – Assessing vascular status in orthopedic trauma