Thorax and Lungs
advertisement
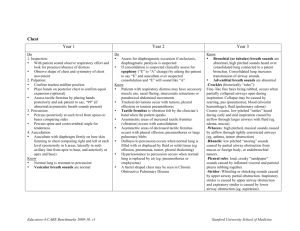
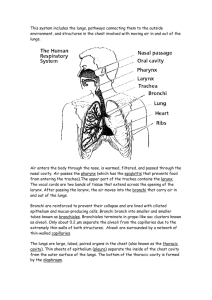
Thorax and Lungs Anterior Thorax (Suprasternal notch) Posterior Thorax Reference Lines Lobes of Lungs Lobes of Lungs Trachea and Pleurae Pleurae Visceral pleura – lines outside of lungs, dipping down into the fissures Parietal Pleura – lines inside of chest wall and diaphragm Lubricating fluid between the pleurae prevents friction Trachea and Bronchi Transport gasses between environment and lung Dead space is space filled with air (about 150 ml) but not available for gaseous exchange Goblet cells in bronchi secrete mucus that entraps particles Cilia in bronchi sweep particles upward Terms Developmental Considerations Infants and Children When cord is cut, blood is cut off from placenta and rushes into pulmonary circulation. Due to less resistance in pulmonary arteries, the foramen ovale closes, along with ductus arteriosus Lungs grow until about 300 million alveoli in adolescence Pregnancy The enlarging uterus elevates the diaphragm 4 cm during pregnancy, but the increased estrogen relaxes thoracic ligaments allowing compensation by increasing the transverse diameter Mother’s tidal volume increases to meet demands of fetus Aging kyphosis calcification of costal cartilage decreased vital capacity decreased number of alveoli decreased mucous production Health History Cough Onset? Gradual or sudden? Frequency? • • • • Continuous throughout day – acute illness (respiratory infection) Afternoon/evening – may reflect exposure to irritants at work Night – postnasal drip, sinusitis Early morning – chronic bronchial inflammation of smokers Sputum? How much? Characteristic? • Chronic bronchitis – productive cough for 3 months of the year for 2 years in a row • Characteristics • • • • White of clear mucoid – colds, viral infection, bronchitis Yellow or green – bacterial infection Rust colored – TB, pneumococcal pneumonia Pink, frothy – pulmonary edema, medications? Cough up blood? Description of cough – dry, hacking Associative and Alleviating factors Painful? Health History Shortness of Breath (SOB) Onset, associative factors • Determine how much activity precipitates SOB Affected by position? • Orthopnea – difficulty breathing when supine (heart failure?) Time of day/night • Paroxysmal nocturnal dyspnea – awakening from sleep with SOB and needing to be upright to achieve comfort Allergies? • Asthma attacks Alleviating factors Health History Chest pain with breathing? Past history of respiratory infections? Location, onset, duration, frequency, intensity, associative and alleviative factors Bronchitis, emphysema, asthma, pneumonia Smoking history Environmental exposure Self – care behaviors Immunizations, TB skin tests, chest X-rays Assessment - Inspection Inspect thorax Symmetry AP diameter • Normal 1:2 • AP diameter = transverse diameter, “barrel chest”. Occurs with normal aging, chronic emphysema, and asthma Symmetry and normal development of trapezius muscle • Hypertrophied in COPD Position person takes to breathe • COPD – tripod position Posterior Chest Symmetric chest expansion Place warmed hands on posterolateral chest wall with thumbs at level of T9 or T10 Slide hands medially to pinch up a small fold of skin between thumbs Ask person to take a deep breath As person inhales, the thumbs should move apart symmetrically • Unequal chest expansion occurs with atelectasis, pneumonia, thoracic trauma • Pain accompanies deep breathing when pleurae are inflamed Tactile Fremitus Fremitus is a palpable vibration transmitted through patent bronchi and lung parenchyma to the chest wall where they can be felt as vibrations Place either the palmar base of ulnar edge of one of the hands on the person’s back and ask to repeat “ninety-nine.” Start at lung apices and palpate from one side to another Symmetry is most important Normally, fremitus most prominent between scapulae and decreases as you progress down Abnormalities in Fremitus Decreased fremitus occurs when anything obstructs transmission of vibrations • • • • Obstructed bronchus Pleural effusion or thickening Pneumothorax Emphysema Increased fremitus occurs with compression or consolidation of lung tissue • Lobar pneumonia Rhonchal fremitus – palpable with thick secretions Crepitus – coarse crackling sensation palpable over skin surface. Occurs in subQ emphysema when air escapes from lung and enters subQ tissue Percussion Start at the apices and percuss across tops of both shoulders and down the lung region at approx. 5cm intervals Make a side to side comparison Avoid damping effect of scapulae and ribs Resonance predominates in healthy lungs Hyperresonance is found when too much air is present (emphysema or pneumothorax) Dullness signals abnormal density (pneumonia, pleural effusion, atelectasis, tumor) Expected Percussion Notes Percussion Notes Auscultating Posterior Chest Breath sounds Instruct the person to breathe through the mouth a little deeper than usual, but to stop if they feel dizzy. Hyperventilation may lead to fainting! Use the flat diaphragm endpiece of the stethoscope and listen for at least one full respiration in each location Continue to think: • What am I hearing? • What should I expect to be hearing? • Bronchial • Bronchovesicular • Vesicular Do not confuse background noise with lung sounds • • • • Stethoscope tubing bumping together Shivering Hairy chest Rustling of gown Characteristics of Normal Breath Sounds Location of Normal Breath Sounds Auscultation Abnormal Findings Decreased breath sounds • Obstruction of bronchial tree (by secretions, mucous plug, foreign body) • In emphysema due to loss of elasticity in the lung fibers and decreased force of inspired air. The lungs are already hyperinflated so not much air will be coming in. • Obstruction of sound by pleural thickening • Silent chest – no air moving in or out Increased breath sounds – louder than normal • Bronchial sounds • Heard in abnormal location, such as periphery • High pitched, with prolonged expiratory phase • Occur in consolidation (pneumonia) or compression (fluid in intrapleural space). Dense lung tissue enhances transmission of sound. Auscultating Adventitious Sounds Adventitious sounds Sounds not normally heard in the lungs Caused by moving air colliding with secretions in trachea or bronchi, or from popping open of previously deflated airways Crackles (fine) Description: popping sounds heard during inspiration. May be stimulated by rolling a strand of hair between fingers near the ear Mechanism: Inhaled air collides with previously deflated airways. Airways suddenly pop open creating a crackling sound Clinical example: • Early inspiratory – COPD • Late inspiratory – Pneumonia, heart failure, interstitial fibrosis Crackles (coarse) Description: • loud, low-pitched, bubbling and gurgling sounds early in inspiration. Sound like Velcro Mechanism: • Inhaled air collides with secretions in trachea and large bronchi Clinical example: • Pulmonary edema, pneumonia, pulmonary fibrosis, depressed cough reflex Pleural friction rub Description: • Coarse and low pitched superficial sound. Both inspiratory and expiratory. Mechanism: • Caused when pleurae become inflamed and lose normal lubricating fluid. Pleural surfaces rub together during respiration. Heard best in anterolateral wall. Clinical example: • Pleuritis Wheeze Description • High pitched musical squeaking sound predominantly during expiration Mechanism • Air squeezed or compressed through narrowed airways (collapsing, swelling, secretions, tumors) Clinical example • Acute asthma or chronic emphysema Rhonchi (sonorous) a.k.a. Wheeze Description • Low-pitched, musical snoring Mechanism • Airflow obstruction Clinical example • Bronchitis, obstruction of bronchus from obstruction or tumor Stridor Description • High pitched, inspiratory, crowing sound, louder in neck than over chest wall Mechanism • Originates in larynx or trachea. Upper airway obstruction from inflamed tissue or obstruction Clinical example • Croup and acute epiglottitis. Obstructed airway. Consolidation or compression of voice sounds will enhance the voice sounds Assessing the Anterior Chest Symmetric chest expansion Abnormally wide costal angle occurs with emphysema Tactile and vocal fremitus Percussing and Auscultating Anterior Chest Begin percussing the apices in supraclavicular ares, continuing down in intercostal spaces Note cardiac and liver dullness and stomach tympany Chronic emphysema leads to hyperinflation of lungs, resulting in hyperresonance where you would expect cardiac dullness Auscultate lung fields down to the 6th rib. Progress from side to side moving downward and listen for one full respiration at each location Pulmonary Function Test Forced expiration of 6 seconds or more occurs with obstructive lung disease Developmental Considerations Infants While infant is sleeping, can inspect and auscultate the lungs • Infants normally have a rounded thorax, reaching a 1:2 (anteroposterior to transverse) diameter by age 6 • If a barrel shape persists after age 6, possible chronic asthma or cystic fibrosis If baby begins to cry, it actually enhances the palpation of tactile fremitus Pregnancy Wider thoracic cage Aging Kyphosis – outward curvature of thoracic spine Calcification of costal cartilages leading to less mobility