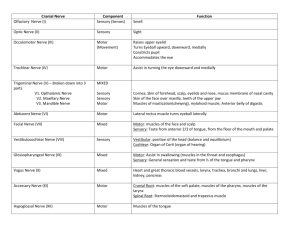
Cranial Nerve II
advertisement

Cranial Nerve II Cranial Nerve VII: Facial Nerve • CN-VIII is a mixed nerve. It sensory component serves the external ear and a small area behind the ear, and also transmits taste sensations from the anterior two-thirds of the tongue. It's motor component regulates the muscles of facial expression and the secretion of sublingual salivary gland and lacrimal gland. Brancial motor (special visceral efferent) Supplies the muscles of facial expression; posterior belly of digastric muscle; stylohyoid, and stapedius. Visceral motor (general visceral efferent) Parasympathetic innervation of the lacrimal, submandibular, and sublingual glands, as well as mucous membranes of nasopharynx, hard and soft palate. Special sensory (special afferent) Taste sensation from the anterior 2/3 of tongue; hard and soft palates. General sensory (general somatic afferent) General sensation from the skin of the concha of the auricle and from a small area behind the ear. General somatic afferent fibers carry sensory impulses to CNS from skin and skeletal muscles General somatic efferent fibers carry motor impulses from CNS to skeletal muscles General visceral afferent fibers carry sensory impulses to CNS from blood vessels and internal organs General visceral efferent fibers carry motor impulses away from CNS to smooth muscles and glands Special somatic efferent fibers carry motor impulses from brain to muscles used in chewing, swallowing, speaking, and forming facial expressions Special visceral afferent fibers carry sensory impulses to brain from olfactory and taste receptors Special somatic afferent fibers carry sensory impulses to brain from receptors of sight, hearing, and equilibrium Branchial Motor Component • The largest component of the facial nerve. • Provides voluntary control of the muscles of facial expression (including buccinator, occipitalis and platysma muscles), as well as the posterior belly of the digastric, stylohyoid and stapedius muscles. Motor • Facial motor nucleus also receives afferent fibers from other sources for reflexes. for instance, fibers from superior colliculus provides a pathway for closure of eyelids in the event of intense light or rapidly approaching objects. Fibers from trigeminal sensory nuclei completes corneal reflex, etc. • Descending innervations are provided by corticobulbar tract which is mainly crossed except fibers that innervate frontalis and orbicularis oculi muscles. Therefore, upper motor neuron lesion (i.e., corticobulbar tract) only affects lower facial muscles contralaterally (drooling, unsymmetrical smile, cannot whistle, OK frown). Control of the Muscles of Facial Expression • The portion of the nucleus that innervates the muscles of the forehead receives corticobulbar fibers from both the contralateral and ipsilateral motor cortex. The portion of the nucleus that innervates the lower muscles of facial expression receives corticobulbar fibers from only the contralateral motor cortex. Lower Motor Neuron (LMN) Lesion • Results from damage to the motor nucleus of CN VII or its axons. • A LMN lesion results in the paralysis of all muscles of facial expression (including those of the forehead) ipsilateral to the lesion. Upper Motor Neuron (UMN) Lesion • Results from damage to neuronal cell bodies in the cortex or their axons that project via the corticobulbar tract • Voluntary control of muscles of the forehead will be spared due to the bilateral innervation of the portion of the motor nucleus of CN VII that innervates the upper muscles of facial expression. • UMN lesions are usually the result of a stroke. Upper motor neuron lesions spare forehead; lower motor neuron lesions cause paralysis in upper and lower face. Gustatory fibers • Originate from taste receptors located on soft palate, epiglottis, and the tongue, enters brain by two branches. Taste receptors from soft palate together with preganglionic terminate into geniculate ganglion via greater petrosal nerve of facial nerve (A motor branch innervates stapedius muscle). Anterior two thirds of the taste buds on the tongue terminates in geniculate ganglion by the choda tympani branch of the facial nerve. These two nerves synapse at Geniculate Ganglion, axons from geniculate ganglion enter the brain stem in the nervus intermedius and then turn in the solitary tract. Other gustatory axons from glossopharyngeal and vagus nerves also join this fasciculus. Fibers from all three sources then terminate into the rostral part of the solitary nucleus, which is also referred as gustatory nucleus. Gustatory fibers • Fibers from gustatory nucleus becomes central tegmental tract and runs ipsilaterally and projects to the medial part of the ventral posterior nucleus of the thalamus. From there, fibers project to the cortical area for taste, which is adjacent to the general sensory area for the tongue and extends onto the insula and forward to frontal operculum. Cutaneous fibers • Distributed to auricle, external area of external acoustic meatus and external surface of tympanic membrane. Axons from geniculate ganglion for cutaneous sensation continue into nervus intermedius and then get into spinal tract and terminate into spinal trigeminal nucleus. Parasympathetic nuclei • Superior salivatory: – Leave facial nerve in the chorda tympani branch and join the lingual branch of the mandibular nerve to the floor of oral cavity. Terminates in submandibular ganglion. Postganglionic fibers innervate salivary secretion of submandibular and sublingual glands. • Lacrimal nuclei: – Fibers leave facial nerve in the greater petrosal nerve and terminate the ptergopalatine ganglion located in pterygopalatine fossa. Postganglionic fibers innervate secretion and vasodilation of lacrimal secretion. Bell's palsy • Caused by the edema compressing facial nerve (viral infection?). Affected side: paralysis of facial muscles, loss of taste (ageusia) in the anterior two thirds of the tongue, impaired secretion of sublingual and submandibular glands, and hyperacusis (paralysis of stapedius muscle). • Most Bell's Palsy can be recovered fully without any complications. Recovery of severe case may rely on axonal regeneration. Sometimes the regeneration of the salivary fibers may tap into greater petrosal nerve and reach the pterygopalatine ganglion, which result in lacrimation (crocodile tears) instead of salivation when stimulated by aroma and taste onto superior salivatory nucleus. Cranial Nerve VIII: Vestibulocochlear Nerve • CN-VIII is a purely sensory nerve. Some refer to it as the acoustic or auditory nerve. The vestibulocochlear nerve carries two kinds of sensations: vestibular (balance) and audition (hearing) from receptors in the inner ear. Auditory information travels to the auditory cortex in the temporal lobes. Vestibulocochlear Nerve • Cochlear nerve originates from spiral ganglion. Once it gets inside the skull, it bifurcates. One branch ends in dorsal cochlear nucleus and the other ends in ventral cochlear nucleus. Fibers from ventral cochelear partly cross and terminate to the superior olivary nucleus. Axons from superior olivary nucleus then terminate to inferior colliculus via lateral lemniscus. Uncrossed fibers from ventral cochelear nucleus run ipsilaterally. Fibers from dorsal cochelear nucleus cross over and relay at superior olivary nucleus, joins the lateral lemniscus and to inferior colliculus. Auditory fibers that cross pons are referred as trapezoid body. Lateral lemniscus are the ascending auditory tract ending at inferior colliculus. Fibers from inferior colliculus project into medial geniculate body via inferior brachium and then project ipslaterally to the primary auditory cortex in the temporal lobe. Posterior to the primary auditory cortex lies the auditory association cortex (Wernicke’s area), essential for understanding spoken language. Vestibulocochlear Nerve • Above the cochlear level, the auditory pathway is both crossed and uncrossed. Not only nucleus projects fibers to both sides, there are also commissural fibers in between the nuclei of lateral lemniscus and inferior colliculi. • The ability to detect the direction and sources of sound are determined from the discrepancy in times of arrival of the stimulus in left and right ears. Deafness in one-ear can lose such abilities. • Along with ascending fibers, fibers from auditory and cortical area terminate in medial geniculate body (corticogeniclate fibers). Cortico-collicular fibers to inferior colliculi. Colliculo-olivary fibers, from inferior colliculi to olivary nucleus. Colliculo-cocheleonuclear, from inferior colliculus to dorsal and ventral cochlear nuclei. All above fibers run ipsilaetrally except cortico-collicular runs on both sides. Their functions involve with auditory reflexes. Vestibular portion • Vestibular nuclei: four groups have been found. Including lateral vestibular nucleus (Deiters' nucleus), superior. medial, and inferior vestibular nuclei. Connection to the cerebellum • The vestibulocerebellum, consisting the flocculonodular lobes, inferior vermis, and etc., receiving info from superior, medial and inferior vestibular nuclei, entering the cerebellum by inferior cerebellar peduncle. Connection to the spinal cord • Vestibulospinal tract, originate from lateral vestibular nucleus, uncrossed, terminates in the medial part of the ventral horn. Its major function is to maintain and regulate the tone of muscles involved with posture to maintain the balance. • Fibers from medial vestibular nucleus form the medial longitudinal fasciculus, mediate reflexes like vestibulo-ocular reflex (turning the head and the turning of eyes in opposite direction). Cranial Nerve IX: Glossopharyngeal Nerve • CN-IX is a mixed nerve. The sensory component provides general sensation and taste from the posterior one-third of the tongue, and part of the skin of the external ear. The motor component serves to control the stylopharyngeas muscle, which elevates the pharynx during swallowing and speech. Also, part of the motor component serves to innervate the parotid gland, an important salivary gland. Afferent fibers • Taste information collected from posterior one third of the tongue joins the solitary tract along with the few taste buds on the epiglottis collected by vagus nerve. • Carotid sinus functions as baroreceptors which monitor arterial blood pressure and the carotid body, located in the bifurcation of internal and external carotid artery, contains chemoreceptors which monitor the level of oxygen in the blood. Similar structures like aortic bodies (chemoreceptors) and aortic arch (barorecetors) are innervated by vagus nerve. Somatic afferent fibers • General sensations of pain, temperature, touch from posterior one third of the tongue Efferent fibers • Innervate stylopharyngeus muscle Parasympathetic fibers • Parasympathetic innervation of the smooth muscle and glands of the pharynx, larynx, parotid gland Brancial motor (special visceral efferent) Supplies the stylopharyngeus muscle. Visceral motor (general visceral efferent) Parasympathetic innervation of the smooth muscle and glands of the pharynx, larynx, parotid gland, and viscera of the thorax and abdomen. Visceral sensory (general visceral afferent) Carries visceral sensory information from the carotid sinus and body. General sensory (general somatic afferent) Provides general sensory information from the skin of the external ear, internal surface of the tympanic membrane, upper pharynx, and the posterior onethird of the tongue. Special sensory (special afferent) Provides taste sensation from the posterior one-third of the tongue. Cranial Nerve X: Vagus Nerve • The vagus nerve is a mixed nerve and is the only cranial nerve that regulates the functions of organs in the thoracic and abdominal cavities. It is called the vagus ("wandering") nerve because its branches wander throughout the body. Its sensory component includes sensory fibers from the larynx, pharynx, esophagus, and parts of the external ear. Its motor component serves muscles in the larynx and pharynx, and parasympathetic innervation of the smooth muscles and glands of the same areas, and thoracic and abdominal areas. Brancial motor (special visceral efferent) Supplies the voluntary muscles of the pharynx and most of the larynx, as well as one extrinsic muscle of the tongue. Visceral motor (general visceral efferent) Parasympathetic innervation of the smooth muscle and glands of the pharynx, larynx, and viscera of the thorax and abdomen. Visceral sensory (general visceral afferent) Provides visceral sensory information from the larynx, esophagus, trachea, and abdominal and thoracic viscera, as well as the stretch receptors of the aortic arch and chemoreceptors of the aortic bodies . General sensory (general somatic afferent) Provides general sensory information from the skin of the back of the ear and external auditory meatus, parts of the external surface of the tympanic membrane, and the pharynx. Special sensory (special afferent) A very minor component of CN X. Provides taste sensation from the epiglottic region. Lower Motor Neuron (LMN) Lesion • Hoarseness (due to paralysis of the intrinsic muscles of the larynx on the affected side). • Difficulty in swallowing due to the inability to elevate the soft palate on the affected side (due to paralysis of the levator palatini muscle). Lower Motor Neuron (LMN) Lesion • Unilateral damage to the recurrent laryngeal nerve can occur during surgical procedures in the neck (Grave’s Disease), resulting in hoarseness due to unilateral weakness or paralysis of the muscles controlling the vocal fold on the affected side. • Enlargement of the paratrachial lymph nodes, as can be seen in metastatic lung cancer, can lead to compression of one of the recurrent laryngeal nerves with similar results. Cranial Nerve XI: Accessory Nerve • CN-XI is a purely motor nerve serving the sternomastoid and trapezius muscles in the neck and back • The accessory nerve has a cranial root and a spinal root, both of which consist of branchial motor fibers. Branchial motor cranial root (special visceral efferent) Innervates muscles of larynx and pharynx. Branchial motor spinal root (special visceral efferent) Innervates the trapezius and sternocleidomastoid muscles. Cranial Nerve XII: Hypoglossal Nerve • CN-XII is a purely motor nerve supplying most of the muscles of the tongue (three of the four extrinsic muscles of the tongue including genioglossus, styloglossus, and hyoglossus except Palatoglossus by Vagus nerve)