PowerPoint 演示文稿
advertisement

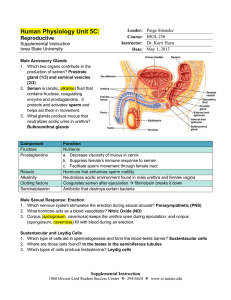
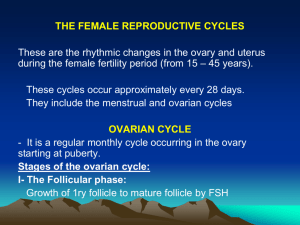
Physiology of the female reproductive system 1. Different periods of Female Neonatal period : 4 weeks childhood: 4 weeks to age of 12 adolescence: menarche, age of 12-17 sexual maturity: begain 18, maintains for 30 years peri-menopausal period:begain 40, maintains for 10-20 years pre-menopause, menopause(last time of menorrhae), post-menopause senility 2.The definition of menstruation Menarche: the onset of the first menses occurs about two years after the onset of pubert occurs between 13 and 15 years of age anovulatory for first two years The first day of menstrual bleeding is considered day 1 of the menstrual cycle The length of menstrual cycle is 28 –30 days The duration of flow is 2-7 days The volume of menstrual blood loss is 30ml-50mL(<80mL),darkness and nonclotting. The Founction of ovary Produce oocyte Endocrine: produce female hormone 3.Reproductive cycle Devided into 3 phases Menstruation: 1-4days the follicular phase:5-14 days a number of follicles developing, only one dominant follicle others become atretic ovulation:14th, releasing oocyte luteal phase: 15-28 days unless pregnancy occurs 1) Development of ovary Ovarian cycle is divided into four phases Development of follicles primitive folliclesprimary follicles secondary follicles antrun/ developing follicles maturity follicles ovulation corpus luteum corpus albican 2)Ovarian steroid hormones Estrogens rise in plasma by 4th day of cycle from granulosa cells and theca cells negative feedback to FSH positve feedback to LH Progesterone: from corpus luteum maximal production occurs 3-4 days after ovulation and maintained for 11 days negative feedback on FSH and LH 4.Clinical manifestations of hormone changes 1)Endometrium be sloughed to a basal level in menstruation proliferative phase: 5-14 days (stroma thickens,gland elongated) in follicular phase, a maximal thickness in ovulation Secretory phase :15-28 days (stroma loose, edematous, vesseltwisted, gland tortous) in corpus luteum Menstrual phase:1-4 days Endomitrium is sloughed and bleeding onset 2)endocervix Cervical also changes in response to the reproductive cycle Cervical gland secrete thin,clear,watery,mucus in follicular phase maximal in ovulation Mucus becomes thick,opaque,tenacious in corpus luteum phase 3)vagina Thickening and maturation of the surface epithelial cells responed to E2 in follicular phase thickening and secretory changes of vaginal epithelium in corpus luteum phase 4)Hypothalamic thermoregulating center Progesterone shifts the Basal body temperature upward(BBT) BBT record is a useful tool to evaluate the reproductive cycle 5.H-P-O axis The control of menstruation is based on a feedback loop of H-P-O axis Hypothalamus Producing GnRH(gonadotropin-releasing hormone) be secreted in a pulsatile manner be a pulse generator of cycle be influenced by E and neurotransmitters Pituitary Producing Gonadotropins follicle-stimulating hormone(FSH) luteinizing hormone(LH) be protein hormones secreted by the anterior pituitary gland be pulsatile manner be influenced by E,P, and other factors Ovaries ovarian sex steroid hormones estradiol (E), progesterone(P) Feedback of H-P-O axis Concept of feedback the magnitude and the rate of GnRH, FSH, LH are determined by E, P, negative feedback : resulting in decreased secretion ofGnRH FSH,LH positive feedback: resulting in increased secretion of LH,which triggers ovulation Key words reproductive cycle menstruation ovarian cycle H-P-O axis feedback