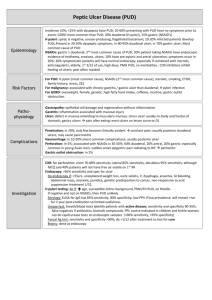
Epidemiology of gastric and duodenal ulcers
advertisement

Epidemiology of gastric and duodenal ulcers Sarah Bowman April 2008 What is an ulcer? • Acid breaks through protective substances on gut wall • Duodenum (1st part small intestine) – most common site • “Gastric” ulcers – in stomach Pain, bloating, nausea, “fullness”, weight loss, tiredness Complications: bleeding, perforation, obstruction Diagnosis • Endoscopy (>55yrs, first time). Capture all cases? • Faecal / breath tests for H. pylori • GI series (rare) False positive tests Missed cases? – risk of transmission / disease progression Why are they important? • HPA – “infectious disease” but main effects are from chronic burden • Potential “medical emergency” • Chronic symptoms – health and economic costs • H. pylori also linked to: – Functional dypepsia – Cancer (2-6x more likely, though still rare) • Differential clinical outcome - interaction between bacterial properties (phenotypic variation), genetics and environmental / behavioural factors Emergency admission for perforation Rates per million resident population. Threeyear moving averages Implications for care of older people (Bardhan et al. 2004, Digestive & Liver Disease 36(9), 577-588) Causes? Ulcers are only found in white people, usually in long thin types given to worry and irritability (Robinson & Bruce 1940) Causes & Risk Factors • Helicobacter pylori – 90% duodenal ulcers – 70-75% gastric ulcers • NSAIDs • Lifestyle factors increase risk – smoking, physical stress, salt (GU) • Genetic susceptibility / protection against H. pylori infection (twin studies, mouse models) • Rarely…Zollinger-Ellison syndrome & others Treatment & Outcome (NICE) • 10% cases fail treatment (HPA) • 1 course of combination therapy clears most cases (74% duodenal ulcers) • Relapse greater for gastric ulcers (affected by lifestyle factors). At 3-12 months: – Duodenal ulcers: 39% clear (acid suppression only); 91% (combination therapy) – Gastric ulcers: 45% clear (acid suppression only); 77% (combination therapy) Consequences • Primary care – GP consultations, drug costs (increasing resistance) • Secondary care – complications, surgery • Tertiary care – rarely needed • Socio-economic cost: Standardised average annual years of life lost (up to age 75) = 2.6 (per 10,000) (Females=1.8; Males=3.5) (1999 & 2001 pooled data, ONS) Consequences… • “Mass eradication of H pylori is impractical because of…generating antibiotic resistance, so we need to know how to target prophylaxis.” (Calam & Baron 2001) • Ulcers occurring in absence of H. pylori or NSAIDs / aspirin. Combination therapies less effective in absence of H. pylori – data needed • Screening? Cost-effective cost/LYS < £10,000 over 80yrs. But effects of eradication on morbidity / mortality? Time, Person, Place… UK Incidence & Prevalence (Time) Increases due to: • Increase in H.pylori? • Different strain of H. pylori? • Another concurrent gut infection? But what about differing temporal changes of CU and DU and between men and women? Barron & Sonnenberg (2002) UK Incidence & Prevalence (Time) Evidence of cohort effect 1970-1986: (Primatesta et al. 1994) • Decreased hospitalized morbidity and mortality • Related more to changes in risk factors (e.g. smoking) in different cohorts than new pharmacological treatments? implications for public health! OR: Genetic factors may be more important (Malaty et al. 1994) UK Incidence & Prevalence (Person) H. pylori infection • Incidence: 1-3% of adults p.a. (HPA) • Prevalence infection: 40% population (HPA: >50% of 50+yr olds) Ulceration •Incidence: –DU in 30-50yrs old; higher incidence in men –GU in >60yr olds; higher incidence in women •Low prevalence in younger age groups •Duodenal ulcer: up to 10% of population UK Incidence & Prevalence (Person) Current trends: • Annual age-standardized period prevalence decreased 1994-1998, particularly deprived areas (men 3.3/1000 1.5/1000; women 1.8/1000 - 0.9/1000) • Sex incidence evening out – decreasing incidence in young men; increasing in older women • But emergency admission rates for complications unchanged in last 30yrs • Kang et al. (2006) – increase in case fatality for DU. Due to concomitant comorbidity / increasing ulceration (NSAIDs) / H.pylori (i.e. changing natural history)? • Future decrease in prevalence? International prevalence (Place) Place • Worldwide. Prevalence 100% in developing countries • Potential for “re-spread” in UK through travel? • H. pylori - oral / faeco-oral transmission associated with poverty / overcrowding in childhood • Increased prevalence in children with history of ulcer in the mothers – due to common environmental factors? • Variation between ethnic groups even within countries Place – Regional variation (NCHOD) • 2004-06 pooled data from ONS • SMR All E&W 99 (97101) NE Males Females 100 (97103) 99 (96101) 111 (102- 124 (110121) 139) 100 (88113) –Lowest = E. Midlands (89). Highest = London (112) –Industrial areas = 114, London suburbs = 111, London cosmopolitain = 153 • Directly standardised age specific death rates (per 100,000 European standard population) - regional centres higher than national average • High rates affected by lifestyle factors & e.g. aspirin in deprived areas (raised CVD risk)? NCHOD data - critique • Based on original underlying cause of death (death certification) • Numerator - mortality data 1993-2006 (ONS) with codes assigned using postcode of usual residence • Changes to coding causes of death in England & Wales. Data based on new coding • Denominator data - latest revisions of ONS mid-year population estimates, current at Oct 2007 - quite accurate • NCHOD regularly updated Data sources Other potential sources: HES, primary care records, prescribing database Data source Valid? Reliable? Complete Timely ? ? Accessible ? Relevant ? Cochrane reviews √ (RCTs / metaanalyses) √ (RCTs / metaanalyses) Treatment √ focus √ Partial PubMed articles Some small studies Some small studies Epidemiol focus √ √ √ NEPHO √ ONS data √ ONS data Regional 1999 & life years 2001 lost data – London only √ √ Data sources Data source Valid? Reliable? Complete? Timely Accessibl ? e? NCHOD √ ONS data. Updated though based on death certification √ ONS data. Updated though based on death certification Age-specific √ √ NEPHO rates not Update website split by sex d 2007 (small numbers) HPA √ √ Based on reporting from primary care Testing & trend monitoring. No routine publications √ √ Relevant ? √ √ Data sources Data Valid? source Reliable? Complete Timely? ? Accessible ? Relevant ? Patient √ NICE UK guidance & review articles. Written by clinicians. Reviewed 18monthly √ NICE guidance & review articles. Written by clinicians. Reviewed 18monthly Patient info. √ Based on recent guidance & articles √ √ Patient √ Peer Plus reviewed. Based on NICE guidance & review articles. Written by clinicians. √ Peer reviewed. Based on NICE guidance & review articles. Written by clinicians. Clinical focus – diagnosis and managem ent √ Based on recent guidance & articles √ Partial Conclusion • • • • Disease mechanism / transmission poorly understood Risk factors multiple & interacting H. pylori is main cause but has changing natural history “Each generation has carried its own particular risk of bearing ulcers throughout adult life” (Susser & Stein 1962) • Current pattern = exposure to H. pylori + genetics + exposure to drugs + environmental / behavioural factors • DU / GU likely to continue causing significant chronic disease burden and personal / societal cost. Predicting future pattern difficult Questions? References Bardhan, K. D., Williamson, M., Royston, C., Lyon, C. (2004) Admission rates for peptic ulcer in the Trent Region UK, 1972-2000: Changing pattern, a changing disease? Digestive and Liver Disease, 36, 577-588 Barron & Sonnenberg, Gut (2002), 50(4), 568-570 Malaty, H., Engstrand, L., Pederson, N., Graham, D. (1994), "Helicobacter pylori infection genetic and environmental influences, a study of twins", Annals of Internal Medicine, Vol. 120 pp.982-6 Primatesta et al. (1994), Int. J. Epidemiol. 23(6), 1206-1217 Robinson, S.C., Bruce, R.M. (1940), "The body build of the ulcer patient", American Journal of Digestive Diseases, Vol. 7 Roderick P, Davies R, Raftery J, Crabbe D, Pearce R, Patel P. The cost-effectiveness of screening for Helicobacter pylori to reduce mortality and morbidity from gastric cancer and peptic ulcer disease: a discreteevent simulation model. Health Technol Assess, 2003;7(6). Available at: http://www.cinahl.com/cexpress/hta/summ/summ706.pdf Bardhan et al. 2004 Elective surgery. Rates per million resident population. Three-year moving averages. The number of elective anti-ulcer operations has declined, and more markedly so for DU. The greatest decline for both groups was in younger men, 35–64 years, in whom such operations were most commonly performed (Fig. 4). The rate of decline, however, was no greater in the era of modern medical treatment (Table 3).