Drugs affecting GI function
advertisement

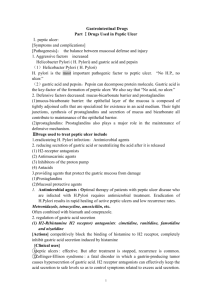
Drugs Affecting GI Functions (Summary) Assoc. Prof. Iv. Lambev E-mail: itlambev@mail.bg www.medpharm-sofia.eu I. Treatment of Peptic Ulcer Acid-peptic diseases include hyperacidity, GERD (gastro-esophageal reflux disease), stress induced mucosal erosions and peptic ulcers (gastric or duodenal). A localized loss of gastric or duodenal mucosa leads to the formation of peptic ulcer. Peptic ulcer arises when the mucosal protective factors are impaired and aggressive factors dominate. Ulcers occur five times more in the duodenum (predominantly in the duodenal bulb and pyloric channel). Benign gastric ulcers are located mainly in the antrum. The Nobel Prize in Physiology or Medicine (2005) was awarded jointly to Barry J. Marshall and J. Robin Warren "for their discovery of the bacterium Helicobacter pylori and its role in gastritis and peptic ulcer disease" J. Robin Warren (2005) Barry J. Marshall (2005) A. Antacids (Drugs Neutralizing Gastric Acid) Antacids are weak bases that neutralize gastric hydrochloric acid. They raise the pH of the stomach contents, decrease the acid load delivered to the duodenum and reduce the activity of pepsin. Antacids are given between meal and at bed time when symptoms of hyperacidity usually occur; the presence of food in the stomach can prolong their neutralizing capacity. 1.Systemic Antacids: Sodium bicarbonate acts rapidly, has a brief effect and raises the pH of gastric secretion to 7.4. On neutralizing gastric asid (HCl), it forms carbon dioxide (CO2) and sodium chloride (NaCl). Formation of CO2 results in gastric distention and belching that can be dangerous if ulcer is near perforation. Unreacted alkali is absorbed and can raise the pH of blood (systemic alkalosis) and the urine. Absorption of NaCl may increase sodium load and this may exacerbate fluid retention in patients with hypertension and CHF. The sudden release of CO2 can cause “rebound acidity”. 2. Non-systemic Antacids are poorly absorbed from GIT a) Buffer Type Non-systemic Antacids •Aluminium hydroxide •Magnesium trisilicate •Magaldrate These drugs have slow onset but longer effect and raise the gastric pH to 3.5–4. The pepsin activity is inhibited around pH 4. “Rebound acidity” is not a problem. Aluminium hydroxide and Magnesium trisilicate neutralize gastric hydrochloric acid to form aluminium chloride and magnesium chloride which further react with intestinal bicarbonates to form aluminium carbonate and magnesium carbonate. Sodium chloride formed in these reactions gets reabsorbed to compensate the loss of chlorides during gastric acid neutralization. Buffer type non-systemic antacids do not disturb the acid-based balance of the body. Aluminium hydroxide can cause constipation and Magnesium trisilicate – diarrhoea, as a side effect. Magaldrate is a hydrated complex of Aluminium and Magnesium hydroxide sulfate. b) Non-Buffer Type Antacids (Calcium carbonate and Magnesium hydroxide) are powerful drugs with fast onset of action, and raise gastric pH > 7. Like Sodium bicarbonate Calcium carbonate may cause belching due to liberation of carbon dioxide. It can cause constipation too, due to formation of calcium stearate. Magnesium hydroxide does not liberate carbon dioxide but can cause diarrhoea. c) Other Antacids Simethicone (dimethyl polysiloxane) is a silicone polymer and therefore has water-repellent properties. It acts as an antifoaming agents and reduces gastric flatulence. It is not absorbed from GIT. B. Drugs, Reducing Gastric Acid Secretion 1. Proton Pump Inhibitors (PPIs) •Esomeprazole •Lansoprazole •Pantoprazole •Omeprazole •Rabeprazole PPIs are the most widely used drugs for peptic ulcer and related disorders, because of their efficacy and safety. PPIs are prodrugs. In the parietal cells they undergo a molecular rearrangement to sulfenamide cation (active metabolite). This cation makes a covalent disulfide bond with –SH group of gastric proton pump H+/K+-ATPase. Thereby PPIs inactivate the proton pump irreversibly and shut off the acid secretion. PPIs also inhibit gastric mucosal carbonic anhydrase and reduce bicarbonate secretion to mucus. ADRs: diarrhoea, headacke, inhibition of vitamin B12, hypochlorhydria and risk of enteric infections. 2. Antagonist of H2-receptors (H2-blockers) – for treatment of peptic ulcer: •Cimetidine (? …) •Famotidine •Nizatidine •Ranitidine •Roxatidine 3. Prostaglandin analogues •Misoprostol (PGE1) and Enprostil (PGE2) 4. Anticholinergics (M1-blockers) •Pirenzepine and Telenzepine C. Mucosal Protective Drugs •Sucralfate (aluminium salt of sulfated sucrose) in acidic environment (pH < 4) polymerizes and forms a gel over ulcer crater which acts as acid resistant physical barrier. It also stimulates mucosal synthesis of PGE2 and secretion of bicarbonates. Sucralfate is administered orally. It is not effective in preventing or healing NSAIDs induced ulcer. •Colloidal Bismuth Subcitrate in gastric acidic media converts into bismuth oxychloride and bismuth citrate which chelate glucoproteins and amino acids at ulcer base to form an acid resistant coating. It stimulates PGE, mucus and bicarbonate secretion. It has also anti-H. pylori activity. D. Anti-Helicobacter Pylori Drugs Peptic ulcer, although a multifactorial disease, also occurs due to colonisation of mucosa by H. pylori: in 90% in cases with duodenal ulcers, 60 to 70% – with gastric ulcers and 50% in patients with non-ulcer dyspepsia. H. pylori is accepted as a cause of chronic atrophic gastritis too. It is a risk factor for gastric adenocarcinoma and to some extent for non-Hodgkin’s lymphoma affecting stomach. H. pylori produces urease which hydrolyses urea into ammonia. Ammonia neutralizes gastric acid to create a neutral protective cloud over the bacteria. H. pylori infection can be detected by a “urea breath test”, but the test is not used after the treatment with PPIs. Since H. pylori becomes less virulent in absence of acid, a combination of an antibiotic with PPIs (or H2-blockers) is more efficacious in eradicating this Gram (–) bacterium. Preferred anti-Helicobacter pylori Combinations •Dual therapy (7–10 days). Omeprazole (40 mg OD) + Amoxicillin (1000 mg BD) •Triple therapy (14 days) Omeparzole (or lanzoprazole), plus Clarithromycin, plus Amoxicilin (resp. Metronidazole, or Tetracycline) II. Antiemetic Drugs Vomiting means expulsion of gastric contents through mouth due to mass antiperistalsis. It is often preceded by nausea. Vomiting can be life saving, physiological response to the ingested toxic substances. It also can be an adverse reaction of radiation and antineoplastic agents. Vomiting also occurs in early pregnancy, during migraine attack, in motion sickness, etc. The CTZ at the base of the 4th ventricle has numerous receptors: D2-, 5-HT3-, M-, H1-, for SP etc. Stimulation of different receptors are involved in different pathways leading to emesis. Main Antiemetic Drugs (1) 5-HT3-receptor antagonists (setrons) •Dolasetron, Granisetron, Ondansetron (Zofran – tab. 8 mg), Tropisetron (2) Neurokinine-1 (NK1-, SP1-) receptor antagonists: Aprepitant, Fosaprepitant (prodrug) (3) D2-receptor antagonists Neuroleptics: Chlorpromazine, Prochlorperzine, Haloperidol Prokinetics: Domperidone, Metoclopramide (4) H1-blockers: Diphenhydramine, Doxylamine, Promethazine (5) M-cholinolytics: Scopolamine (Scopoderm TTS) (6) Miscellaneous Antiemetic Agents 5-HT3-receptor antagonists block 5-HT3-receptors both peripherally (on vagal nerve terminals) and centrally (CTZ). Granisetron is the most potent antiemetic compared to ondansetron and dolasetron. These drugs are most effective when given i.v. 30 min prior to anticancer chemotherapy (granisetron – 10 mcg/kg). These doses may be repeated every 24 h. Neurokinine-1 (NK1-, SP1-) receptor antagonists (Aprepitant etc.) have the similar indications. D2-receptor antagonists Phenothiazines (prochlorperazine, thiethylperazine) and butyrophenone group of antipsychotics (droperidol) can be used to treat postoperative nausea and vomiting. Emetogenic activity Cisplatin Carmustine Cyclophosphamide Mitomycin C L-Asparginase Fluorouracil Methotrexate Etoposide Vincristine Antiemetic activity 5-HT3-blockers D2-blockers Glucocorticoids H1-blockers Prokinetic antemetic Metoclopramide is D2-receptor antagonists but in high doses it also blocks 5-HT3-receptors. It crosses BBB. Its prokinetic action (stimulation of GI motility) is connected with stimulation of 5-HT4-receptors, present on excitatory interneurons, which enhances ACh release from primary cholinergic neurons in myenteric plexus. Metoclopramide is used as antiemetic and as gastrokinetic agent to accelerate gastric empting prior to giving emergency general anaesthesia in case the patient has taken food less than 4 h before. This drug may also be successful in stopping persistent hiccups. Being a central and peripheral D2-blocker it produces sedation, muscle dystonia, in high doses – extrapyramidal effects, galactorrhoea in females and gynecomastia in males. Domperidone has a similar mechanism of action as metoclopramide, but it is a peripheral D2-blocker. Its antiemetic efficacy is lower than metoclopramide. It is also used to prevent the emetic side effect of levodopa or bromocriptine without affecting their antiparkinsonian effect. H1-blockers with anticholinergic properties (Cyclizine, Diphenhydramine) are useful for prevention or treatment of motion sickness and vertigo due to labirinth dysfunction. Doxylamine can be used in morning sickness (vomiting during the first trimester of pregnancy, due to the effect of increased oestrogen level on CTZ. Pyridoxine serves as a cofactor for the glutamate decarboxylase and thus increases the synthesis of GABA which acts as inhibitory neurotransmitter at CTZ. Anticholinergic drugs: Hyoscine (Scopolamine) is used in motion sickness as TTS. Miscellaneous Antiemetic Agents •GCS: Dexamethasone, Methylprednisolone •Canabinoides: Nabilone and Dronabinol stimulate CB1receptors present on neurons around the vomiting center and are used in oncology. Their hallucinogenic activity is weak. •Anxiolytics: Aprazolam, Diazepam, Lorazepam •Others: Benzocaine, Sodium citrate, T-ra Menthae III. Laxative and Purgative Drugs Laxatives provide elimination of soft semisolid stool and Purgatives provide more watery evacuation. Laxatives are used: to treat constipation; to avoid undue straining at defecation in cases of hernia, haemorrhoids or CVD; before or after surgery of any anorectal disease; in bedridden patients. Lactulose is an osmotic laxative drug. It is nonabsorbleindigestible disaccharide (sugar), which increases fecal bulk by hydrophilic and osmotic action. It is given in dose of 10 g orally. Latency period is 1 to 3 days. Lactulose is also used for treatment of hepatic encephalopathy. Liquid paraffin is an inert mineral oil. Liquid pararaffin is a fecal lubricant and stool softner as it retards water absorption from the stool. It is given 15 to 30 ml per day at bed time. Latency period is 1 to 3 days. Purgatives are used for complete colonic cleansing prior to GI endoscopic procedures or before intestinal operation. Purgatives may also be needed to flush out warms after the use of anthelmintic drugs. In low doses purgatives can be used as laxatives too. Osmotic Purgatives include: Saline purgatives (Magnesium sulfate) and Electrolyte purgatives (PEG – PolyEthylene Glycol, which is a nonabsorbable sugar). They act on small and on large intestine. Saline purgatives are soluble inorganic salts which increase the fecal bulk by retaining water by osmotic effect, thus increasing peristalsis. These agents also release CCK which further helps in increasing intestinal secretion and peristalsis. Saline purgatives should be ingested with enough water to protect vomiting. These drugs can cause electrolyte disturbances and must be avoided in patients with CVD as well as during pregnancy. Irritant purgatives •Antraquinone group: Senna, Cascara and Aloë •Organic agents: Bisacodyl, Sodium picosulfate •Oils: Castor oils Aloë vera All irritant purgatives stimulate peristalsis by irritant action of intestinal mucosa. They also stimulate colonic electrolyte and fluid secretion by altering the absorptive and secretory activity of the mucosal cells. Senna, Cascara and Aloë occur naturally in plants. Senna is more commonly used. These plant agents contain anthraquinone glycosides with purgative action. The organic irritants are prodrugs. The primary site of action of their active metabolites is in the colon. Bisacodyl is activated in the intestine by deacetylation. In the colon Sodium picosulfate is converted to the active metabolite. Castor oil is hydrolyzed in the intestine by pancreatic lipase to ricinolic acid which increases the intestinal motility. IV. Antidiarrhoeal Agents Diarrhoea is an abnormal increase in the frequency and the liquidity of stool. Increased motility of GIT and the decreased ability of intestine to absorb water from the stool are the major factors, causing diarrhoea. Osmotic diarrhoea may cause by ingestion of some type of meal, use of some osmotic substances, lactulose or magnesium containing antacids, lactase enzyme deficiency. Secretory diarrhoea occurs when the intestinal wall loses its functional integrity or gets damaged resulting in an increased secretion of electrolyte in the intestinal tract. This may be due to some bacterial infection (Schigella, Salmonella), bacterial endotoxins (from E. coli, V. cholerae, S. aureus), viral infections (rotavirus etc.), protozoal infections (Lamblia intestinalis, E. histolytica), underlying pathology (inflammatory bowel disease) or due to side effects of drugs (antibiotics, anticancer agents, colchicine, prostaglandins, orlistat, acarbose). Excess of bile also causes diarrhoea. Motility disorder diarrhoea. Increased motility reduces the contact time of the stool with the intestinal wall, so that lesser amount of water is absorbed back from the faces. Motility disorders include IBS, scleroderma, diabetic neuropathy, vagotomy etc. Some drugs can increase intestinal motility: prokinetic antiemetics, bethanechol, digitalis, quinidine, ampicillin (causes disbiosis); neurosis, etc. Treatment of infective diarrhoeas needs proper diagnosis and suitable antibiotic and/or antiprotozoal drug. For symptomatic relief of non-specific diarrhoes are used: (1) Antimotility and Antisecretory Agents a) Opioid agonists which does not cross BBB • Loperamide (Imodium®) and Racecadotril (Hidrasec®) These drugs stimulate mu- and delta-receptors, present in the small and large intestines. Activation of mu-receptors decreases peristaltic movements. Activation of deltareceptors contributes to their antisecretory effects. Although all opioids such as morphine and codeine have antidiarrhoeal effects, their CNS effects and dependence liability limit their usefulness. Loperamide directly stimulates mu- and delta-receptors. Racecadotril blocks enzyme encephalinase and increases local concentration of enkephalins in intestinal mucosa which then stimulate mu- and delta-receptors. This drug can be used orally from children under 5 years old (including babies), but Loperamide is contraindicated in children < 5 years old. b) Miscellaneous Agents •Carbo activatus (absorbent drug) •Bismuth subsalicylate reduces stool frequency and liquidity in acute diarrhoea due to inhibition of PG synthesis. Bismuth has some antimicrobial and mucosal protective effect too. (2) Fluid and Electrolyte Replacement During diarrhoea, a glucose-coupled transport continues in the intestines which causes water and electrolyte losses through the stools. V. Treatment of Inflammatory Bowel Disease Ulcerative colitis and Crohn’s disease are two important inflammatory bowel diseases. The pathogenesis of these diseases involves autoimmune mechanism and imbalance between proinflammatory and anti-inflammatory cytokines. The main drugs, used in the treatment of these diseases are aminosalicylates, GCS and some immunosuppressants. Antidiarrhoeal agents must be avoided in active and severe ulcerative colitis as they can lead to dilatation of the colon and its perforation. Aminosalicylates (sulfasalazine, olsalazine) contain a 5-aminosalicylic acid (5-ASA) moiety bound by an azo (N=N) bond to an inert moiety or by another 5-ASA molecule. 5-ASA inhibits the synthesis of PGs by inhibiting COX, like salicylates, as well as inhibiting the production of cytokines. 5-ASA also inhibits the activity of nuclear factor-kB, which is an important transcription factor for pro-inflammatory cytokines. It suppresses the generation of superoxide free radicals. Aminosalicylates induce and maintain remission in patients with ulcerative colitis. GCS (Prednisone, Prednisolone) have been the mainstay of the treatment for acute/severe exacerbations of irritable bowel disease. Moderately severe attacks of ulcerative colitis should be treated orally with systemic GCS. Immunosuppressive Agents •Cyclosporine may induce remissions in case of severe ulcerative colitis unresponsive to GCS. •Azathioprine, mercaptopurine •Methotrexate is useful in controlling relapse of Crohn’s diseases unresponsive to GCS or azathioprine •Infliximab is a chimeric (25% mouse and 75% human) anti-TNF-alpha-monoclonal antibody, which inhibits T-cells and macrophage functions. Consequently, the release of other proinflammatory cytokines (IL-1, 2, 8; collagenase and metaloproteinases) is prevented. It is administered by i.v. infusion. A single dose of infliximab (5 to 10 mg/kg) induces remission in approximately 40% of patients with Crohn’s disease. An additional dose after 8 weeks produces long-lasting remission. •Adalimumab is a recombinant human anti-TNF-alphamonoclonal antibody. It is given s.c. and has a longer plasma half life. It has lesser side effects compared to infliximab. VI. Drugs used in Pancreatic Insufficiency Pancreatic enzyme agents contain a mixture of amylase, lipase and proteases. They are the mainstay of the treatment of the pancreatic enzyme insufficiency which is most commonly caused by cystic fibrosis, chronic pancreatitis or pancreatic resection. Exocrine pancreatic enzyme insufficiency leads to fat and protein indigestion which in turn causes steatorrhoea, azotorrhoea, vitamin deficiency and weight loss. •Festal, Kreon, •Mezym forte, Panzytrat VII. Hepatoprotectors Drugs which stimulate regenerative processes •Acidum oroticum, Essentiale, Silymarin Drugs which stimulate fat infiltration •Thioctic acid (Acidum aphfa-lipoicum) Derivatives of Methionine: Ademethionine Interferons (in viral hepatitis) •Interferon alfa-2a •Peginterferon alfa-2a •Interferon alfa-2b Antiviral vaccines: Hepatitis A and B vaccine, •Hepatitis A vaccine, Hepatitis B vaccine VIII. Drugs Acting on Biliary tract Choleretic Drugs: Cholagol, Cholamin, Febichol Cholekinetic Drugs: Oleum olivarum, Rowachol Drugs which improve the solubility of cholesterol gallstones: Ursodeoxycholic acid IX. Probiotics – regulators of intestinal or other bacterial flora BioGaia, Linex, Lactoflor, Lactagyn® (vaginal flora), Normoflor, Probien®