Gram positive cocci (streptococci)
advertisement
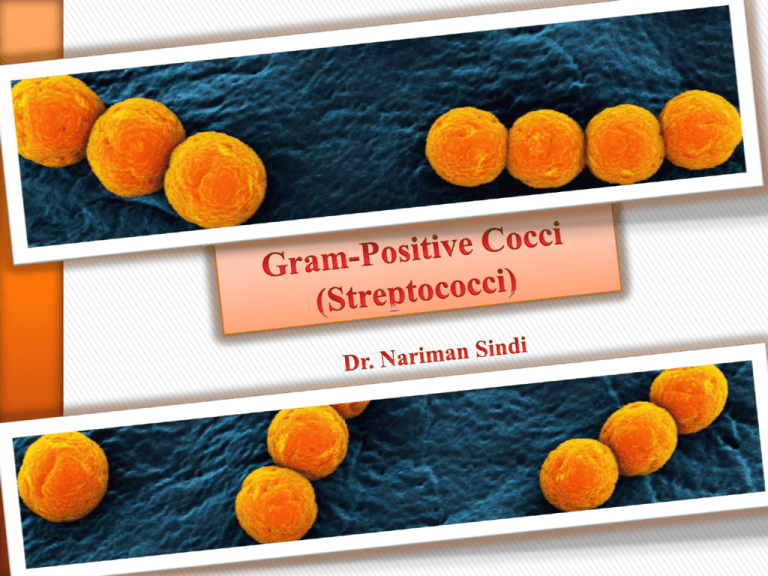
1 CLASSIFICATION The classification of streptococci is based on: 1) Hemolysis: A. Alpha-hemolytic streptococci (α-hemolytic): • Incomplete lysis (partial hemolysis) of red blood cells (RBCs) in the agar resulting in the formation of a greenish zone around their colonies. B. Beta-hemolytic streptoccoci (β-hemolytic): • Complete lysis of RBCs occurs resulting in the formation of a clear zone around their colonies. C. Gamma-hemolytic streptococci (γ-hemolytic): • Some streptococci are non-hemolytic on RBCs in an agar medium. Alpha, beta, and gamma hemolysis 2 CLASSIFICATION 2) Cell wall carbohydrates (group-specific carbohydrates): • The streptococci can be classified based on the antigenic characteristics of the carbohydrate found on the cell wall. These antigens are called Lancefield antigens and are given letter names (from A, B, C, D, E, through S). 1) S. pyogenes (group A) (β-hemolytic). 2) S. agalactiae (group B) (β-hemolytic). 3) S. pneumoniae (α-hemolytic). 4) E. faecalis (group D) (γ-hemolytic). 5) Viridans group streptococci (α-hemolytic). 3 Lancefield Group A Beta-hemolytic Streptococci (Streptococcus pyogenes) 4 PROPERTIES Characteristics: • Streptococcus pyogenes (which means pus producing). • Beta-hemolytic. • Gram positive cocci arranged in chains. • Catalase test-negative. Habitat and Transmission: • Main habitat: exist as a normal flora on skin and throat of human. • Transmission: is via respiratory droplets. 5 VIRULENCE FACTORS Beta-hemolysis group A streptococci have several virulence factors: 1) Streptolysin O: • This enzyme destroys RBCs and WBCs. 2) Streptolysin S: • Responsible for beta-hemolysis. 6 VIRULENCE FACTORS 3) M-protein: • Anti-phagocytic. 4) Lipoteichoic acid (LTA): • Mediates adherence to epithelial cells. 5) Pyrogenic exotoxin (also called erythrogenic toxin): • Produced only by group A streptococci. • Causes the rash of scarlet fever. 7 VIRULENCE FACTORS 6) Pyogenic exotoxin A: • This toxin is responsible for streptococcal toxic shock syndrome which is similar to toxic shock syndrome toxin (TSST) caused by S. aureus. 7) Streptokinase (fibrinolysin): • Breaks up fibrin blood clots. 8) Hyaluronidase: • facilitates the spread of the bacteria through tissues by breaking down hyaluronic acid, an important component of connective tissue. 8 Cell surface structure of Streptococcus pyogenes and secreted products involved in virulence 9 DISEASES AND PATHOGENESIS Beta-hemolytic group A streptococci cause two different forms of diseases; 1) Local Invasion and / or Exotoxin Release. 2) Antibody-Mediated Disease. Local Invasion and / or Exotoxin Release: 1) Streptococcal pharyngitis: A. Strep throat (red, swollen tonsils and pharynx). B. High temperature. C. Swollen lymph nodes. D. Lasts 5 days. E. Penicillin therapy speeds recovery. 10 DISEASES AND PATHOGENESIS 2) Skin infection: A. Skin infection can range from folliculitis ( infections of the hair follicles). B. cellulitis (a deep infection of the skin cells, producing red, swollen skin which is hot to touch). C. Impetigo (most common in children and is frequently found around the mouth). 11 DISEASES AND PATHOGENESIS D. Necrotizing fasciitis (streptococcal gangrene): • Certain strains have M proteins that block phagocytosis, allowing the bacteria to move rapidly through tissue. • Streptococci enter through a break in the skin. • Within a day the patients develops swelling, heat, and redness that move rapidly. A day later the skin color changes from red to purple to blue, and large blisters form. • Later the skin dies and muscle may also become infected. • Use high dose penicillin and clindamycin for treatment. 12 DISEASES AND PATHOGENESIS 3) Scarlet fever: A. Caused by pyrogenic exotoxin (erythrogenic toxin). B. Fever and scarlet red rash. The rash begins on the trunk and neck, and then spread to the extremities. C. Penicillin and clindamycin are the choice of treatment for skin infections. 13 DISEASES AND PATHOGENESIS 4) Streptococcal toxic shock syndrome: A. Group A streptococci can cause toxic shock syndrome like that cause by S. aureus. B. It can be treated by penicillin and clindamycin. 14 DISEASES AND PATHOGENESIS Antibody-Mediated Disease: 1) Rheumatoid fever: A. May follow untreated beta-hemolytic group A streptococcal pharyngitis. B. Fever. C. Myocarditis. D. Joint swelling (arthritis). E. Chorea (Sydenham’s chorea or St. Vitus dance). • uncontrolled dance-like movement of the extremities. Starts after 2-3 weeks. • Affect children 5-15 years of age. • Penicillin treatment reduces rheumatoid fever to become uncommon. F. Subcutaneous nodules. G. Rash called erythema marginatum. 15 DISEASES AND PATHOGENESIS Subcutaneous nodules Erythema marginatum is described as the presence of pink rings on the trunk and inner surfaces of the arms and legs 16 17 DISEASES AND PATHOGENESIS 2) Acute post-streptococcal glomerulonephritis: Tea colored urine A. Following streptococcal skin or pharynx infection after one week. B. Tea-colored urine. 18 LABORATORY DIAGNOSIS 1) Gram stain: • Gram positive cocci in chains. 2) Culture: • Beta-hemolytic colonies on blood agar. 3) Bacitracin antibiotic test: • S. pyogenes is the only streptococcus which is sensitive to bacitracin. Bacitracin sensitive-test 19 LABORATORY DIAGNOSIS 3) Streptococcal pharyngitis: • pharyngitis (pus on tonsils), a throat swab should be sent for a rapid antigen detection test (RADT). • This test can be completed within minutes and highly specific for Streptococcus pyogenes. Rapid, direct test kit for diagnosis of group A S. pyogenes. Throat swab introduces to latex beads and antibiotics. Positive result causes clumping. Negative-milky smooth reaction. 20 LABORATORY DIAGNOSIS 4) Rheumatoid fever: • ASO titer: A. the detection of patient’s anti-streptolysin O (ASO) antibodies in the blood to confirm whether previous exposure to S. pyogenes has occurred. B. The antibody levels begin to rise after 1 to 3 weeks of strep infection, peaks in 3 to 5 weeks. 21 TREATMENT AND PREVENTION 1) Penicillin G. 2) Penicillin V. 3) Erythromycin. 4) Skin infections: • Use penicillinase-resistant penicillin (oral), dicloxacillin which covers both S. pyogenes and Staphylococcus aureus. 5) Rheumatoid fever: • Penicillin. • To prevent further damage to the heart. 6) For permanent heart damage: • Antibiotics are required when certain procedures are performed (such as dental work), due to the high risk of bacterial endocarditis. • Amoxicillin (oral) is commonly given. 7) Streptococcal toxic shock syndrome or necrotizing fasciitis: • Add clindamycin (work rapidly to block toxin production). 22 Lancefield Group B: Beta-hemolytic Streptococcus agalactiae 23 PROPERTIES Characteristics: • Catalase test-negative • Beta-hemolytic. • Bacitracin-resistant. Habitat and Transmission: • Main habitat: exist as a normal flora in human vagina (25% of pregnant women carry Group B streptococci in their vagina). • A baby can acquire these bacteria during delivery. • Transmission: during birth (THINK OF GROUP B FOR BABY). 24 DISEASES Group B streptococci causes neonatal infection (< 3 months of age) include: 1) Neonatal meningitis and sepsis. Group B streptococci causes infections in non-pregnant adults: 1) It has been an increase in the incidence of Group B streptococcal in elderly people > 65 years of age 2) In patient with diabetes, renal or liver failure and neurological disease: causes sepsis and pneumonia. 25 LABORATORY DIAGNOSIS 1) Gram stain: • Specimen (s) collection from cerebrospinal fluid (CSF) or urine. • Gram positive cocci arranged in chains. 2) Culture: • From CSF, urine, or blood. • Blood agar, incubated aerobically at 37°C. • Colonies usually large with narrow zone of beta-hemolysis. 26 LABORATORY DIAGNOSIS 3) Biochemical identification: • Catalase test-negative. • Bacitracin disc: resistant. • Hydrolysis of hippurate: positive. • CAMP test: positive. Detail of the positive CAMP test with Streptococcus agalactiae after 24 hours of cultivation in atmosphere at 37 °C. Positive test is characterized by an arrowhead-shaped zone of complete hemolysis. 27 LABORATORY DIAGNOSIS Group B (S. agalactiae) shows a positive reaction ‘Arrowhead’ shaped enhanced zone of βhemolysis Staphylococcus aureus Group A (S. pyogenes) shows a negative reaction 28 TREATMENT • Penicillin G PREVENTION • No vaccine available. • Ampicillin should be given to mother if she has fever, or if the neonate is premature. 29 Lancefield Group D: Gamma-hemolytic Enterococci: Streptococcus faecalis 30 PROPERTIES Characteristics: • Gram-positive ovoid cocci in chains. • Catalase test-negative. • Alpha-, beta-, or gamma-hemolytic. Habitat and Transmission: • Main habitat: Large intestine and female genital tract. • Transmission: During gastrointestinal (GI) or genitourinary tract procedure, enterococcus may enter the bloodstream. 31 VIRULENCE FACTOR • Extracellular polysaccharide (extracellular dextran) helps E. faecalis bind to heart valves. DISEASES 1) Endocarditis. 2) Urinary tract infections. 3) Wound infection. 4) Bacteremia and sepsis after infecting intravenous catheters. 32 LABORATORY DIAGNOSIS 1) Gram stain. 1) Culture: • α, β, or γ- hemolysis • Enterococcus can be cultured in: A. 6.5% sodium chloride (NaCl). B. 40% bile. 33 E. faecalis S. pyogenes Enterococcus faecalis, bile esculin agar (BEA) 34 TREATMENT AND PREVENTION • Ampicillin: sometimes combined with an aminoglycoside. • The treatment of multiple resistant enterococci is very difficult and complicated. Vancomycin resistant enterococci (VRE) are important causes of hospital-acquired infection. Other option for vancomycin-resistant E. faecalis is linezolid, ampicillin. • Gentamicin or streptomycin used in combination with ampicillin for the treatment of enterococcal endocarditis. 35 36 PROPERTIES Characteristics: • The pneumococcus does not have Lancefield antigen!, they appear as ‘lancet shaped’ gram positive cocci often in pairs (diplococci) are oval pointed end rather than being round. • Catalase test-negative • Alpha-hemolytic. Habitat and Transmission: • Main habitat: human upper respiratory tract of healthy individuals. • Transmission: respiratory droplets. Encapsulated pneumococci in sputum (indicated with arrows). In the right bottom is a detail of pneumococci arranged in a short chain of ovoid (lanceolate) cocci. Gram stain, magnification ×1000. 37 PATHOGENESIS A) Polysaccharide capsule: • is the major virulence factor of the pneumococcus (84 serotypes), which only provides immunity to 1 out of the 83 possible capsule type. B) IgA protease: • Enhances the ability of organism to colonize the mucosa of the upper respiratory tract (URT). C) Pneumolysin: • Produce toxic effect on erythrocytes (RBCs). DISEASES The major cause of respiratory diseases and bacterial meningitis worldwide. 1) Pneumonia (in adult). 2) Meningitis (particularly in elderly) . 3) Sepsis. 4) Sinusitis and otitis media (in children). 38 This figure shows the location of the lungs and airways in the body. This figure also shows pneumonia affecting the lower lobe of the left lung. Figure B shows normal alveoli. Figure C shows infected alveoli. 39 LABORATORY DIAGNOSIS 1) Specimen (s) collection: • Sputum, blood, CSF. 2) Gram stain: • Reveals gram positive diplococci Microscopy: Gram-positive, non-motile, encapsulated, oval diplococci(lancet shape) 40 LABORATORY DIAGNOSIS 3) Culture: • Blood agar, incubated at 37°C in the presence of 5-10% CO2 • It is alpha-hemolytic (partial hemolysis-greenish color). • Does not grow in presence of: A. Optochin. B. Bile. 4) Positive quellung test: • Swelling when tested against antiserum containing anti-capsular antibodies. • This technique allows for rapid identification of this organism. 41 Streptococcus pneumoniae growing around a HardyDisk™ Optochin disc on Blood Agar. Incubated in CO2 for 24 hours at 35 deg. C. Streptococcus pneumoniae cultivated on blood agar aerobically, 5% CO2, overnight. Zones of alpha-hemolysis around colonies. Streptococcus pneumoniae Quellung (capsular swelling) reaction 42 test Bile TREATMENT AND PREVENTION 1) Penicillin G. 2) Erythromycin. 3) Ceftriaxone. 1) Two vaccines are available: A. pneumococcal polysaccharide vaccine, or PPV: The one made against the 23 most common capsular antigens. • Vaccinate individuals who are susceptible such as elderly people (> 65 years of age). • 60%-70% protection. 43 TREATMENT AND PREVENTION B. Pneumococcal conjugate vaccine (PCV13): • effective in children at preventing otitis and pneumonia. 44 45 PROPERTIES Characteristics: • No lancefield antigens. • Gram positive cocci in chains. • Viridis is the Latin word for green. • Alpha-hemolytic. • Catalase-negative. • Optochin-resistant. • Bile-negative. Habitat and Transmission: • Main habitat: predominant in the oral cavity. • Transmission: procedures. enters bloodstream during dental 46 VIRULENCE FACTORS • Extracellular dextran, which helps this organism to adhere to heart valves. This mechanism underlies their ability to cause heart valves disease following their introduction into the bloodstream (e.g., following tooth extraction). DISEASES 1) Endocarditis. 2) Dental caries (cavities): caused by S. mutans. 3) Brain or liver abscesses: caused by S. intermedius group. 47 DISEASES Dental caries 48 LABORATORY DIAGNOSIS 1) Gram stain 2) Culture: • Alpha-hemolytic and produce a green color in culture. 3) Resistant to optochin. Optochin Disk- No on Zone of Inhibition Hemolysis- Alpha (Green) Colonies of viridans streptococci on blood agar surroundend by a wide zone of alpha-hemolysis. Cultivation 24 hours in an aerobic atmosphere enriched with 5% carbon dioxide, 49 37°C. TREATMENT • Penicillin G. • Treatment of bacterial endocarditis requires antibiotic combination, e. g., penicillin combined with gentamicin. 50 Gram positive cocci GPC Catalase-Test negative Streptococci Beta hemolysis Alpha hemolysis Optochin test Group A Bacitracin: S Group B Group D CAMP testpositive 6.5% NaCl positive S S. pneumoniae R Viridans streptococci 51 52 53