Lectures 3 & 4
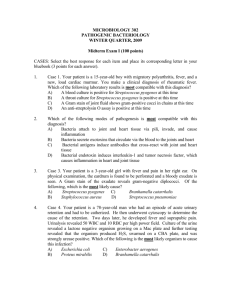
advertisement

STREPTOCOCCUS & ENTEROCOCCUS REVIEW Bacterial Cell Morphology • • • • Gram Stain Cytoplasmic (plasma) membrane Cell wall structure Bacterial cell shapes Common Cell Membrane Gram-Positive Cell Wall Peptidoglycan GramNegative GramPositive Gram-Positive Cell Wall Teichoic Acid Gram-Negative Cell Wall Gram-Negative Cell Wall Genus Streptococcus Commensals or Parasites of man & animals or Saprophytes of decaying matter Morphology Gram-Positive Cocci in Pairs or Chains Gram-Positive Streptococcus Genus Streptococcus Physiology & Metabolism Facultative Anaerobes Fastidious Growth Requirements Fermentative Metabolism of Carbohydrates: Lactic acid, ethanol, acetate endproducts produced; No gas Catalase Negative (2H2O2 ---> O2 + 2H2O) Separation of streptococci from staphylococci Oxidase Negative (oxidoreductase oxidizes substrate w/ O2) Beta, Alpha, or Gamma Hemolysis on blood agar Genus Streptococcus Rebecca Lancefield Developed useful serogrouping system Classification of beta-hemolytic streptococci by group-specific cell wall carbohydrate (CHO) antigen As of 1992, Serogroups A to H and K to V Groups A, B, C, D, and G are most comonly associated with human disease Viridans streptococci and Streptococcus pneumoniae have no group-specific antigen Antigenic Structure Streptococcus pyogenes (Group A) Lancefield Group-specific antigen (C polysaccharide) Complex polysaccharide in cell wall Proteins: Two major classes, M & T antigens Two minor classes, R & F M-Protein: Type-specific antigen Fimbriae-like, hairy extensions Resistant to heat and acid Trypsin Sensitive Specific adherence by lipoteichoic acid and M-protein • (LTA-M) complexes Antigenic Structure Streptococcus pyogenes (Group A) Lancefield Group-specific antigen (C polysaccharide) Complex polysaccharide in cell wall Proteins: Two major classes, M & T antigens Two minor classes, R & F M-Protein: Type-specific antigen Fimbriae-like, hairy extensions Resistant to heat and acid Trypsin Sensitive Specific adherence by lipoteichoic acid and M-protein (LTA-M) complexes T Antigens (not virulence factor) Resistant to trypsin, heat and acid; Adjunct to M-typing; Routine surveillance Others Antigenic Structure (cont.) Streptococcus pyogenes (Group A) Capsular Polysaccharide: Hyaluronic acid Not present in all strains Same as host hyaluronic acid (cartilage,skin etc) Nonimmunogenic Antiphagocytic Hyaluronidase (cell wall division) during late growth Lipoteichoic Acid Lancefield Serogroup Classification of Beta-Hemolytic Streptococci Important in Human Disease Group A Streptococci: Streptococcus pyogenes • One of Most Important Human Pathogens • Suppurative Diseases: Pharyngitis; Scarlet Fever; Cutaneous & Soft Tissue Infections Systemic Disease • Non-Suppurative Sequelae:ARF,RHD,AG Streptococcus pyogenes (Phase Contrast) Lancefield Serogroup Classification of Beta-Hemolytic Streptococci Important in Human Disease (cont.) Group B Streptococci: Streptococcus agalactiae •Neonatal disease & obstetric complications •Systemic, Cutaneous, UTI's Streptococcus agalactiae Lancefield Classification of BetaHemolytic Streptococci (cont.) Group C Streptococci: Pharyngitis Enterococcus & Group D Streptococci Genitourinary Tract Infections (UTIs) Endocarditis Group G Streptococci: S.anginosus-milleri grp; Streptococcus spp. Pharyngitis Non-Lancefield Group Streptococci Viridans Streptococci Dental Caries: Streptococcus mutans Streptococcus sanguis; Streptococcus salivarius; Streptococcus mitis Streptococcus pneumoniae Major Human Diseases of Beta-Hemolytic Streptococci Group A Streptococcus (S. pyogenes): Diverse group of acute suppurative (pus-forming) & nonsuppurative diseases Suppurative Streptococcal Diseases Pharyngitis (& tonsilitis): Scarlet fever: Complication of streptococcal pharyngitis when infecting strain is lysogenized; Frequently develop scarletina rash on upper chest spreading to extremities Cutaneous & Soft Tissue Infxns. Pyoderma (Impetigo: contagious pyoderma with superficial yellow weeping lesions) Erysipelas: Acute superficial cellulitis of skin with lymphatic involvement; face and lower extremities, skin and subcutaneous tissues Erysipelas NOTE: erythema bullae Major Human Diseases of Beta-Hemolytic Streptococci (cont.) Group A Streptococcus (S. pyogenes) Suppurative Streptococcal Diseases Cutaneous & Soft Tissue Infxns(cont.) Cellulitis: Involvement of deeper subcutaneous tissues; Deeper invasion with systemic symptoms Necrotizing fasciitis: (a.k.a., “flesh-eating bacteria”): Infection deep in subcutaneous tissues that spreads along fascial planes, destroying muscle and fat; Initially cellulitis followed by bullae (fluid filled blisters; bulla is singular), gangrene, systemic toxicity, multiorgan failure and mortality in more than 50% of patients Wound Infections Suppurative Streptococcal Diseases Group A Streptococcus (cont.) Other Suppurative Diseases Puerperal & neonatal sepsis Lymphangitis: Inflammation of lymphatic vessel(s) Pneumonia Systemic Disease Streptococcal Toxic Shock Syndrome (TSS): Multisystem toxicity following soft tissue infection progressing to shock and organ failure (not to be confused with Staphylococcal Toxic Shock Syndrome where hyperabsorbent tampons have been identified as an important risk factor) Bacteremia Group A Streptococcal Diseases (cont.) Nonsuppurative Sequelae Post-infection complications of Group A streptococcal disease; Serious complications in pre-antibiotic era; still important in developing countries Acute rheumatic fever (ARF): Inflammation of heart, joints, blood vessels, subcutaneous tissues Rheumatic heart disease (RHD): Chronic, progressive heart valve damage Acute glomerulonephritis (AG): Acute inflammation of renal (kidney) glomeruli Foodborne Disease Epidemiology of Acute Streptococcal Infection • Predilection for upper respiratory tract or skin •Group A commonly colonize oropharynx of healthy children • M-types of strains colonizing throat differ from those on skin • Rapidly killed after phagocytosis, but cell walls not digested and may lead to chronic inflammatory lesions Pharyngitis transmitted by droplets from respiratory secretions • Crowding increases risk (e.g., classrooms, day care facilities) Pyoderma transmitted by direct contact with infectious lesions Nonsuppurative Sequelae of Acute Group A Streptococcal Infection Acute Rheumatic Fever (ARF) Inflammatory reaction characterized by arthritis, carditis, chorea (disorder of CNS with involuntary spastic movements), erythema marginatum (skin redness with defined margin), or subcutaneous nodules Within 2-3 weeks following pharyngitis • Epidemic pharyngitis: ARF in as many as 3% • Sporadic pharyngitis: ARF in 1 per 1000 Morbidity & mortality linked to subsequent disease of heart valve (Rheumatic Heart Disease) Poorly understood pathogenesis with several proposed theories including cross-reactivity of heart tissues & strep AGNs •?? (Type ?? II hypersensitivity, exotoxins, direct invasion) Nonsuppurative Sequelae of Acute Group A Streptococcal Infection (cont.) Acute Glomerulonephritis Follows either respiratory (pharyngitis) or cutaneous (pyoderma) streptococcal infection Associated with well-defined group of M-types Incidence varies from <1% to 10-15% Most often seen in children manifesting as dark, smoky urine with RBC's, RBC casts, white blood cells, depressed serum complement, decreased glomerular filtration rate Latent period: 1-2 weeks after skin infection and 2-3 weeks after pharyngitis Granular accumulations of immunoglobulin due to deposition of immune complexes within the kidney III Hypersensitivity) (Type ?? Determinants of Pathogenicity Cellular Virulence Factors Capsule Antiphagocytic; Nonspecific adherence Hyaluronic acid (polysaccharide) mimics animal tissue Lipoteichoic Acid Cytotoxic for wide variety of cells Adherence: Complexes with M protein (LTA-M) and binds to fibronectin on epithelial cells M-Protein LTA-M protein is adhesin Antiphagocytic Inhibits alternate C’ pathway and opsonization M-like Proteins: bind IgM and IgG F Protein: mediates adherence Extracellular Virulence Factors Exotoxins: Streptolysin O (SLO): Hemolytic and Cytolytic Prototype of oxygen-labile and thiol-activated cytolytic exotoxins (e.g., Streptococcus, Bacillus, Clostridium, Listeria) Lytic for variety of cells: bind to cholesterolcontaining membranes and form arc- or ring- shaped oligomers that make cell leaky (RBC's, WBC’s, PMN's, platelets, etc.) Causes sub-surface hemolysis on BAP Stimulate release of lysosomal enzymes SLO titer indicates recent infection (300-500 in pediatric populations) Extracellellular Virulence Factors (cont.) Exotoxins (cont.): Streptolysin S (SLS): Hemolytic and Cytolytic Oxygen stable, non-antigenic Lytic for red and white blood cells and wall-less forms (protoplast, L- forms) Causes surface hemolysis on BAP Lysogeny: Lysogenized bacteriophages play key role in directing synthesis of various Group A streptococcal enzymes and toxins • Pyrogenic Exotoxin (erythrogenic toxin) • Phage-associated muralysins (lyse cell walls) produced by both Groups A and C Extracellular Virulence Factors (cont.) Exotoxins (cont): Pyrogenic (Erythrogenic) Exotoxins (Types A, B &C) Produced by more than 90% of Grp A strep Lysogeny: Structural gene is carried by temperate bacteriophage, as is the case with diphtheria toxin Mediate pyrogenicity (fever) Causes scarlet fever (scarletiniform) rash Increase susceptibility to endotoxic shock Type C toxin increases permeability of blood-brain barrier Enhance DTH Mitogenic for T lymphocytes (cause cell division), myocardial and hepatic necrosis, decrease in antibody synthesis Immunomodulators (superantigens): stimulate T cells to release cytokines Cardiohepatic toxin Extracellular Virulence Factors (cont.) Enzymes: Nucleases: Four antigenic types (A,B,C,D) Facilitate liquefication of pus generating growth substrates Nucleases A, C have DNase activity Nucleases B, D also have RNase activity Streptokinases: Two different forms Lyse blood clots: catalyze conversion of plasminogen to plasmin, leading to digestion of fibrin C5a Peptidase: destroys C’ chemotactic signals (C5a) Hyaluronidase: hydrolyzes hyaluronic acid Others: Proteinase, NADase, ATPase, phosphatase, etc. Lab Identification of S. pyogenes (Group A) • Primary culture by pour or streak plate • Domed,grayish/opalescent colonies • Encapsulated cells produce mucoid colonies Beta-hemolytic • Zone several times greater than diameter of colony TSA S. pyogenes Lab Identification of S. pyogenes (Group A) (cont.) Catalase Negative: Differentiates from Staphylococcus Bacitracin test: presumptively distinguishing between Group A beta-hemolytic streptococci (bacitracin POS) and other betahemolytic streptococci that are isolated from pharyngeal swabs (95% sensitivity for Grp A strep) Rapid Identification Tests: Based on extraction of Group A carbohydrate directly from throat swabs • ELISA, Coagglutination, Fluorescent Antibody Group B Streptococcus Streptococcus agalactiae Group B Streptococcal Infections Grp B Streptococcal Infections (cont.) Age-Specific Attack Rates of Group B Streptococcal Disease Epidemiology of Neonatal Group B Streptococcal Disease Group B Streptococcus S. agalactiae Diagnostic Laboratory Tests • CAMP factor positive • Hippurase positive CAMP Factor Test Group B Streptococcus S. aureus (Spingomyelinase C) (CAMP Factor) Group A Streptococcus Enhanced Zone of Hemolysis Hippurase NEG Grp B Streptococci and Campylobacter Hippurase POS Streptococcus pneumoniae • Commonly referred to as pneumococcus • Formerly Diplococcus pneumoniae Streptococcus pneumoniae Infections Pneumococcal Infections (cont.) Epidemiology (cont.) S. pneumoniae • Diplococcus S. pneumoniae: lancet-shaped diplococcus S. pneumoniae Virulence Factors S. pneumoniae Seasonal Incidence Comparison of Morbidity & Mortality for Bacterial Meningitis Genetic Variation (Mutation) Beginning of Molecular Genetics Transformation (In vivo) (Griffith) Streptococcus pneumoniae Diagnostic Laboratory Tests • Optochin sensitivity (Taxo P disc) Optochin Sensitivity Taxo P Streptococcus pneumoniae Enterococcus faecalis Enterococcus faecium • GI tract of humans and animals • Group D carbohydrate cell wall antigen • Formerly Streptococcus Enterococcal Infections Enterococcal Infections (cont.) Important nosocomial pathogen Vancomycin resistant Enterococcus (VRE) Enterococcus Diagnostic Laboratory Tests • Resistant to bile • Esculin hydrolysis • BEA media Enterococcus Group D Streptococcus Bile Esculin Agar Bile Esculin Agar NEG POS Esculin Bile Assay REVIEW Lancefield Serogroup Classification of Beta-Hemolytic Streptococci Important in Human Disease Group A Streptococci: Streptococcus pyogenes One of Most Important Human Pathogens Suppurative Diseases: Pharyngitis; Scarlet Fever; Cutaneous & Soft Tissue Infections; Systemic Disease Non-Suppurative Sequelae:ARF,RHD,AG Group B Streptococci: Streptococcus agalactiae Systemic, Cutaneous, UTI's Neonatal disease Obstetric Complications REVIEW Nonsuppurative Sequelae of Acute Group A Streptococcal Infection Acute Rheumatic Fever (ARF) Inflammatory reaction characterized by arthritis, carditis, chorea (disorder of CNS with involuntary spastic movements), erythema marginatum (skin redness with defined margin), or subcutaneous nodules Within 2-3 weeks following pharyngitis • Epidemic pharyngitis: ARF in as many as 3% • Sporadic pharyngitis: ARF in 1 per 1000 Morbidity & mortality linked to subsequent disease of heart valve (Rheumatic Heart Disease) Poorly understood pathogenesis with several proposed theories including cross-reactivity of heart tissues & strep AGNs •?? (Type ?? II hypersensitivity, exotoxins, direct invasion) REVIEW Nonsuppurative Sequelae of Acute Group A Streptococcal Infection (cont.) Acute Glomerulonephritis Follows either respiratory (pharyngitis) or cutaneous (pyoderma) streptococcal infection Associated with well-defined group of M-types Incidence varies from <1% to 10-15% Most often seen in children manifesting as dark, smoky urine with RBC's, RBC casts, white blood cells, depressed serum complement, decreased glomerular filtration rate Latent period: 1-2 weeks after skin infection and 2-3 weeks after pharyngitis Granular accumulations of immunoglobulin due to deposition of immune complexes within the kidney III Hypersensitivity) (Type ?? REVIEW Determinants of Pathogenicity Cellular Virulence Factors Capsule Antiphagocytic; Nonspecific adherence Hyaluronic acid (polysaccharide) mimics animal tissue Lipoteichoic Acid Cytotoxic for wide variety of cells Adherence: Complexes with M protein (LTA-M) and binds to fibronectin on epithelial cells M-Protein LTA-M protein is adhesin Antiphagocytic Inhibits alternate C’ pathway and opsonization M-like Proteins: bind IgM and IgG F Protein: mediates adherence REVIEW Extracellular Virulence Factors Exotoxins: Streptolysin O (SLO): Hemolytic and Cytolytic Prototype of oxygen-labile and thiol-activated cytolytic exotoxins (e.g., Streptococcus, Bacillus, Clostridium, Listeria) Lytic for variety of cells: bind to cholesterolcontaining membranes and form arc- or ring- shaped oligomers that make cell leaky (RBC's, WBC’s, PMN's, platelets, etc.) Causes sub-surface hemolysis on BAP Stimulate release of lysosomal enzymes SLO titer indicates recent infection (300-500 in pediatric populations) REVIEW Extracellellular Virulence Factors (cont.) Exotoxins (cont.): Streptolysin S (SLS): Hemolytic and Cytolytic Oxygen stable, non-antigenic Lytic for red and white blood cells and wall-less forms (protoplast, L- forms) Causes surface hemolysis on BAP REVIEW Extracellular Virulence Factors (cont.) Exotoxins (cont): Pyrogenic (Erythrogenic) Exotoxins (Types A, B &C) Produced by more than 90% of Grp A strep Lysogeny: Structural gene is carried by temperate bacteriophage, as is the case with diphtheria toxin Mediate pyrogenicity (fever) Causes scarlet fever (scarletiniform) rash Increase susceptibility to endotoxic shock Type C toxin increases permeability of blood-brain barrier Enhance DTH Mitogenic for T lymphocytes (cause cell division), myocardial and hepatic necrosis, decrease in antibody synthesis Immunomodulators (superantigens): stimulate T cells to release cytokines Cardiohepatic toxin REVIEW Extracellular Virulence Factors (cont.) Enzymes: Nucleases: Four antigenic types (A,B,C,D) Facilitate liquefication of pus generating growth substrates Nucleases A, C have DNase activity Nucleases B, D also have RNase activity Streptokinases: Two different forms Lyse blood clots: catalyze conversion of plasminogen to plasmin, leading to digestion of fibrin C5a Peptidase: destroys C’ chemotactic signals (C5a) Hyaluronidase: hydrolyzes hyaluronic acid Others: Proteinase, NADase, ATPase, phosphatase, etc. REVIEW Epidemiology of Neonatal Group B Streptococcal Disease REVIEW REVIEW Streptococcus pneumoniae Infections Infections from endogenous spread from naso- or orapharynx Pneumonia; sinusitis; otitis media; bacteremia; meningitis Colonization highest in children Antecedent viral respiratory tract disease increases risk Most common in cold months Polyvalent vaccine available (newly available for children) REVIEW S.pneumoniae Virulence Factors REVIEW Comparison of Morbidity & Mortality for Bacterial Meningitis REVIEW Genetic Variation (Mutation) REVIEW Beginning of Molecular Genetics REVIEW Transformation (In vivo) (Griffith) REVIEW Enterococcal Infections Group D cell wall antigen Enterococcus faecalis; Enterococcus faecium GI tract of humans and animals UTI most common; wound infections; bacteremia; endocarditis Most infections from endogenous source Prolonged hospitalization and broad-spectrum antibiotics increase risk Antibiotic resistance (VRE) REVIEW