Gram positive cocci and respiratory tract
advertisement

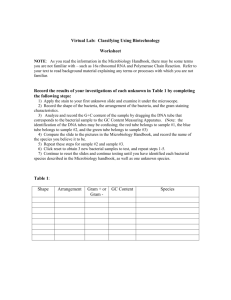
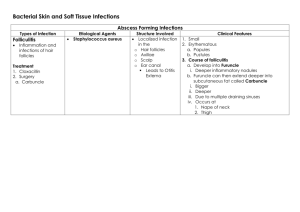
INFORMATIONAL HANDOUT
The respiratory tract can conveniently but artificially be divided into the upper and lower respiratory tracts. The
upper respiratory tract lies above the vocal cords: the lower respiratory tract is situated below the vocal cords. In
health, the lower respiratory tract is sterile. Sterility is maintained by the 'ciliary escalator.' The upper respiratory
tract, however, houses a wide variety of microbes.
UPPER RESPIRATORY TRACT:
LOWER RESPIRATORY TRACT:
THE THROAT
The throat is a warm moist environment allowing many kinds of bacteria to grow. Keep in mind that the normal
microbiota of the throat usually keeps pathogens in check (antagonism). STREPTOCOCCI are common
inhabitants of the throat and some can cause disease. Among the usually harmless commensal bacteria of the
upper respiratory tract are species of viridans STREPTOCOCCI, so named because they are alpha-hemolytic,
that is, upon culture on blood agar their colonies are surrounded by a greenish halo (viridans is Latin for green.)
Streptococci that don't hemolyze blood agar are usually harmless. An example of an alpha-hemolytic Strep is
Streptococcus pneumoniae. It is often part of normal flora, but can go awry and cause infection sometimes. If an
alpha-hemolytic streptococcus is causing infection - it is probably this species (pneumococcal pneumonia is
most common 'typical' kind of bacterial pneumonia). There are many other alpha-hemolytic strep in the throat
which almost never cause disease. S. pneumoniae is sensitive to OPTOCHIN, and this is a convenient test to
determine if an alpha-hemolytic bacterium is indeed S. pneumoniae. This bacterium can also cause pneumonia,
meningitis, and otitis media (earache).
Harmful members of this group are the major cause of sore throats (acute pharyngitis). About 90% of these
cases are caused by BETA-HEMOLYTIC Streptococci, usually Streptococcus pyogenes. This organism is
sensitive to BACITRACIN, an antibiotic - and almost all other Strep are resistant to it. So this is a nice test to
distinguish it. This is a very dangerous pathogen that can cause many kinds of infection in the body. Dangerous
as it is, 5-15% of us may harbor it as part of the normal bacterial community in our throats. Streptococcus
pyogenes produces a wide array of virulence factors and a very large number of diseases. Acute infections may
present as pharyngitis (strep throat), scarlet fever (rash), impetigo (infection of superficial
layers of skin) or cellulitis (infection of deep layers of skin). Its ability to break down skin
tissue has resulted in its famous designation as the 'flesh eating bacterium!' It can also cause
streptococcal toxic shock syndrome. Long term Streptococcus pyogenes infection can lead to
rheumatic fever. I think you get the idea - this is a 'bad bug!'
fingers lost because of flesh eating bacterial infection
There are some other important bacteria that can live as commensals in a minority of the population and that
can under appropriate circumstances go on to cause infection. These include:
Haemophilus influenzae (a gram-negative coccobacillus, a top killer around the world, causes
inflammation of the epiglottis, can lead to death if untreated.)
Neisseria meningitidis (causes meningitis, gram negative coccus, we've discussed this one.
Note that gram negative cocci are rare!)
Corynebacterium diphtheriae (from last unit, gram positive club-shaped rods, disease results in gray
Biology 215, Ruth A. Gyure
Western CT State University
pseudomembrane in throat)
THE SKIN
The skin is generally an inhospitable environment, since it is so dry. The outer keratinized layer of epidermis is
not easily colonized, and the salt from perspiration also inhibits most bacteria. Not surprisingly, most bacteria
that do live on the skin are tolerant of relatively high salt concentrations and are somewhat resistant to drying.
The genus STAPHYLOCOCCUS is an important one in the skin microbiota. Staphylococcus epidermidis is
harmless, as are many others. One - Staphylococcus aureus, may or may not be part of the normal bacteria, but
it certainly can be a pathogen if it begins to grow unchecked. It has many pathogenic characteristics and can be
quite dangerous. This organism produces an enzyme called coagulase - which other Staph don't make. So, it is
a nice diagnostic test to decide if you have Staphylococcus aureus - once you know you have a Staphylococcus
infection. S. aureus has been found to be the causative agent in such ailments as pneumonia, meningitis, boils,
arthritis, and osteomyelitis (chronic bone infection). The main danger of this organism (among many) is the
potent exotoxin it produces.
The oil excreted at hair follicles inhibits most bacteria - though a few organisms actually like to eat it and grow
there quite well! One group, the Propionibacterium, live in the hair follicles. They secrete acid as they ferment,
and the acid conditions help inhibit other bacteria from growing there.
Bacteria on the skin can get into the mouth, and they can get into wounds. Once in the mouth - they have to
compete with the commensals. In a wound, your immune system will put up a good fight. Nevertheless,
Staphlococci have been known to cause some nasty wound infections. Strains that are antibiotic resistant,
especially S. aureus, can be very dangerous - especially for compromised individuals. S. aureus is also a known
cause of food poisoning, since infected food will have exotoxin in it. Even Staph epidermidis, harmless as it is,
can cause infection if an IV drug user gets it deep into the body with a needle. Catheters too may carry this
normally harmless bacterium into places where it should never go...and in the compromised, elderly or a
neonate, this could be disastrous.
A genus closely related to Staphylococcus and present on the skin is MICROCOCCUS. M. luteus in particular is
very common ( and usually harmless). It is very noticeable since it makes yellow colonies on nutrient agar, and
in the gram satin, the gram positive cocci are in clusters. Micrococcus is not facultative like Staph - it is aerobic.
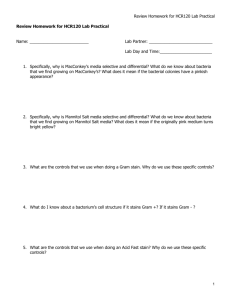
REVIEW OF CHARACTERISTICS OF STREPTOCOCCUS AND STAPHYLOCOCCUS
Please see your gram positive flow chart!
All are gram positive cocci, as revealed by the gram stain which is always the first test. Also, STAPHYLOCOCCI
form clusters, whereas STREPTOCOCCI from chains:
Streptococcus gram stain
A CATALASE test is a very important next step - since Staphylococci are catalase positive, and Streptococci are
catalase negative
_________________________________________________________________________________________
Biology 215, Ruth A. Gyure
Western CT State University
STAPHYLOCOCCI:
gram positive cocci in clusters
tolerate higher salt, 7.5% (will grow on mannitol salt agar)
catalase positive
only Staphylococcus aureus is coagulase positive; it also ferments mannitol, it
also is beta-hemolytic on blood agar.
Normal microbiota: Staphylococcus epidermidis, S. saprophyticus, S. aureus, S. capitis, and more
Usual pathogen: S. aureus; others possible.
Closely related: Micrococcus luteus - strict aerobe, no fermentation, yellow colonies, cells tetrads
Diseases caused by Staphlococcus (usually aureus)? pneumonia, meningitis, skin infection and boils,
arthritis, chronic bone infection, food poisoning, septicemia, toxic shock syndrome.
STREPTOCOCCI:
gram positive cells in chains
facultative, prefer lower oxygen conditions and higher CO2
catalase negative
Streptococcus pyogenes is beta-hemolytic, sensitive to Bacitracin
Of the alpha-hemolytic strep, only S. pneumoniae is sensitive to Optochin
Normal microbiota: Streptococcus pneumoniae, pyogenes!
Streptococcus pneumoniae causes 'typical' pneumonia (pneumococcal pneumonia)
Streptococcus pyogenes causes strep throat, scarlet fever (rash), impetigo, cellulitis ('flesh eating
bacterium), streptococcal toxic shock syndrome.
TEXT REFERENCES: Chapter 24 - entire chapter will be covered between lab and lecture, Chapter 21, pp.
582-586.
ACKNOWLEDGEMENTS
RESPIRATORY TRACT DIAGRAMS: http://www.ntu.ac.uk/life/sh/modules/hlf349/Lectures/349-7.htm
STAPH GRAM STAIN: http://www.health.auckland.ac.nz/courses/Humanbio306
STREP GRAM STAIN: http://www.buddycom.com/bacteria
FLESH EATING BACTERIA PHOTO: http://nnff.org/
Biology 215, Ruth A. Gyure
Western CT State University