strept.doc
advertisement

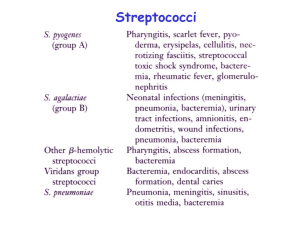
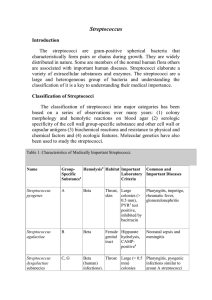
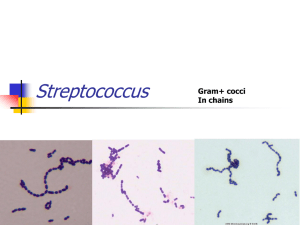
Streptococci Streptococci are G+ve, non motile, & catalase-negative. Clinically important genera include Streptococcus & Enterococcus. They are ovoid to spherical in shape, & occur as pairs or chains. Because of their complex nutritional requirements, blood-enriched medium is generally used for their isolation. Streptococcus forms part of the normal flora of man & animals. Some species (S.pyogenes) are important human pathogens causing pyogenic infections. Classification 1-Hemolytic classification α- hemolytic streptococci cause a chemical change in the hemoglobin of red cells in blood agar, resulting in the appearance of green pigment that forms a ring around the colony. β - hemolytic streptococci cause gross lysis of red blood cells, resulting in a clear ring around the colony. Two types of β – hemolysins are released. Streptolysin O (inactivated by atmospheric oxygen) is demonstrable only in deep colonies while Streptolysin S ( oxygen stable) is responsible for surface colony haemolysis. γ- hemolytic is a term applied to streptococci that cause no color change or lysis of red blood cells. There are two important antigens of beta-hemolytic streptococci: a) C- carbohydrate determines the group of β - hemolytic streptococci. It is located in the cell wall, & its specificity is determined by an amino sugar. b) M protein is the most important virulence factor & determines the type of group A β - hemolytic streptococci. It protrudes from the outer surface of the cell & interferes with ingestion by phagocytes (antiphagocytic). There are approximately 80 Grifith serotypes based on the M protein, which explains why multiple infections with S.pyogenes that produce certain M protein types are rheumatogenic ( cause primarily rheumatic fever ), whereas strains of S.pyogenes that produce other M protein types are nephritogenic (cause primarily acute glomerulonephritis). Although M protein is the main antiphagocytic component of S.pyogenes, the org also has a polysaccharide capsule that play a role in retarding phagocytosis. 2-Serological classification (Lancefield) Many species of streptococci have a polysaccharide in their cell walls known as C- carbohydrate. The Lancefield scheme classifies primarily β - hemolytic streptococci into groups A-U on the basis of their Ccarbohydrate. The clinically most important groups of β - hemolytic streptococci are types A & B. 3-Classification based on Schleifer & Kilpper-Balz This classification depend on the basis of structure of the cell wall peptidoglycan together with the G+C content of the DNA & the results of DNA pairing. They have divided the genus Streptococcus into sex groups. a) b) c) d) e) f) Pyogenic streptococci – S.pyogenes Pneumococci – S.pneumoniae Oral streptococci – S.mutans Enterococci – S. faecalis Lactic streptococci – S.lactice Other streptococci – S.bovis Group A β-hemolytic streptococci S.pyogenes, the most clinically important member of this group of gram positive cocci, is one of the most frequently encountered bacterial pathogens of humans worldwide. It can invade apparently intact skin or mucous membranes, causing some of the most rapidly progressive infections known. A low inoculum suffices for infection. The growth of S.pyogenes is inhibited by antibiotic bacitracin, an important diagnostic criterion. Structure 1-Capsule (antiphagocytic) 2-Cell wall a)Fimbriae: the fimbriae contain the major S.pyogenes virulence factor, M protein. b)Group A-specific C-carbohydrate c)Protein F ( fibronectin- binding protein) 3-Extracellular products Epidemiology The only reservoir for S.pyogenes in nature is the skin & mucous membranes of the human host. Respiratory droplets or skin contact spread Group A streptococcal infection from person to person, especially in crowded environments such as classrooms or children's play area. Pathology S.pyogenes cells, perhaps in an inhaled droplet, attach to the pharyngeal mucosa via actions of protein F, lipoteichoic acid, & M protein. The bacteria may simply colonize; the patient is then considered colonized. Alternatively, bacteria may grow & secrete toxins, causing damage to surrounding cells, invading the mucosa, and eliciting an inflammatory response with attendant influx of white cells, fluid leakage, & pus formation. The patient then has streptococcal pharyngitis. Occasionally, there is sufficient spread that the blood stream is significantly invaded, possibly resulting in septicemia &/or seeding of distant sites, where cellulitis (acute inflammation of subcutaneous tissue), fasciitis (inflammation of the tissue under the skin that covers a surface of underlying tissue), or myonecrosis (death of muscle cells) may develop rapidly or insidiously. Clinical findings 1-Pyogenic diseases a-Sore throat ( acute tonsillitis/ & pharyngitis) is the commonest of streptococcal diseases. The org may spread to surrounding tissue causing complication like otitis media, mastoiditis,sinusitis, meningitis, peritonitis & pneumonia. b-Skin infection Local infections in superficial layers of skin due to S.pyogenes include impetigo & erysipelas. c-Other pyogenic diseases * puerperial sepsis ( postpartum infection of uterus). *Sepsis: Infection of wounds, burns, chronic skin lesion (eczema, psoriasis). *Lymphadenitis, septicaemia, acute endocarditis, abscess in internal organs (brain, liver, lung, & kidney). 2- Toxigenic diseases a-Scarlet fever Scarlet fever occurs as a complication of streptococcal infection (sore throat) when the infecting strain produces erythrogenic toxin & the patient has got no antitoxic immunity. b- Streptococcal toxic shock syndrome This syndrome is mediated by pyrogenic exotoxins that function as superantigens causing massive, nonspecific T- cell activation & cytokines release. It is similar to staphylococcal toxic shock syndrome. . 3-Immunogenic diseases ( non suppurative infection) a- Acute glomerulonephritis(AGN): This rare, postinfectious sequela occur as soon as one week after impetigo or pharyngitis ensues, due to a few nephritogenic strains of group A streptococci. Antigen-antibody complexes on the basement membrane of the glomerulus initiate the disease. The most clinical features are hypertension, edema of the face and ankles, & smoky urine (due to red cells in the urine). b-Acute rheumatic fever: this autoimmune disease occurs two to three weeks after the initiation of pharyngitis. It is caused by cross reactions between antigens of the heart & joint tissues, & the streptococcal antigen (especially the M protein epitopes). It is characterized by fever, rash, carditis, & arthritis. Lab. Diagnosis 1-Specimen: Throat swab, pus& lesion samples, sputum, blood , spinal fluid 2-Smear: G+ve cocci in chains or pairs are found association with pus cells. 3-culture: Specimen should be inoculated immediately. Specimen is inoculated in the blood agar medium & incubated at 37C ْ for overnight. Hemolysis develops better under anaerobic conditions or under 5-10% CO2. The bacterial colonies are small, dry & surrounded by β-hemolysis. A simple technique of detection of S.pyogenes ( group A) is done by agar plate test using paper discs impregnated with bacitracin. S.pyogenes is more sensitive to bacitracin than other streptococci. S.pyogenes can be rapidly identified by fluoruesent antibody technique. 4-Antigen detecting tests: ELISA, agglutination tests 5-Serological tests: test for streptococcal antibodies is not helpful in diagnosing acute infection which may be used to identify & confirm primary infection. They are more commonly used to diagnose non suppurative complications. Treatment S.pyogenes has not acquired resistance to penicillin G, which remains the antibiotic of choice for acute streptococcal disease. In a pencillin allergic patient , Macrolide such as clarithromycin is the preferred drug. Pencillin G plus clindamycin are used in treating streptococcal toxic shock syndrome.