The contributors :- Robert Koch (1893
advertisement

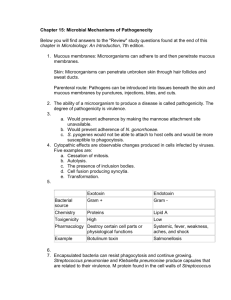
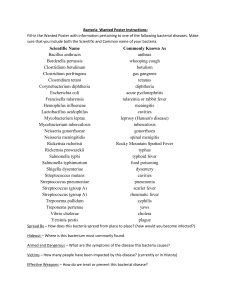
The contributors :Robert Koch (1893-1910): a German scientist, he isolated anthrax bacillus from infected cattle in pure culture. In 1884 he established scientific bases called: Koch’s postulates: a- The organisms should be present in all animals suffering from the disease & absent in all healthy animal. b- The organism must be grown in pure culture outside diseased animal host. c- When such culture is inoculated in susceptible animal, this animal must develop the symptom. d- The organism must be isolated from the experimentally infected animal & shown to be identically with the original isolate. The host parasite relationship:There are various types of interactions can occur between diverse microbial populations, or between microbial & plant or animals. These interactions include: Commensalisms: is a unidirectional relationship between populations in which one population benefits & the other one is unaffected; such as one species of organism uses the body of a larger species as its physical environment. Synergism: in which both populations benefit from the relationship but that the association is not obligatory. Both populations are capable of surviving independently, although they both gain advantage from the synergistic relationship. Mutualism (Symbiosis): is an obligatory interrelationship between two populations that benefits both of them. Competition: occurs when two populations are striving for the same resource; often it focuses on a nutrient present in limited concentrations. Amensalism Predation: involves the consumption of a prey species by (Antagonism): occurs when one population produces a substance inhibitory to another population. (Ex: production of antibiotic). a predatory population. The predatory populations derive nutrition from the prey species. Parasitism: the parasite population is benefited & the host population is harmed; parasitic relationships are characterized by a relatively long period of contact & the parasite is smaller than the host. Epidemiology of Infectious Disease: Epidemiology: This science examines factors involved in the incidence, spread, prevention & control of infectious & noninfectious disease. Disease outbreaks: A disease outbreak is considered to have occurred when several case are reported in a relatively short period of time in a geographically defined area. The study of outbreaks disease includes: 1) Source of disease outbreaks: pathogens are transmitted from one infected individual to another & pathogens can be transmitted directly from one individual to another or indirectly, by means of another living agent(vector), or from inanimate source such as food & water. 2) Reservoirs of pathogens: The source of an infectious agent is known as the reservoir. The transmission of infection agents involves the movement of pathogens from a source to the appropriate portal entry. * The reservoirs of human pathogens are nonliving sources such as soil & water *Animals are sometimes are the reservoirs of human pathogens & may also be involved in the transmission of pathogens. * people infected with a pathogen act as a source of contagion for others ( the term contagious disease indicates that a pathogen will move with ease from one individual to the next). *Infected individuals do not develop disease symptoms; called asymptomatic carriers Although they do not become sick themselves but regard important reservoirs of infectious agents. There are four types of carriers: a- Active carrier: person who has an overt clinical case of the disease. b-A convalescent carrier: a person who has recovered from the infectious disease. c- A healthy carrier: a person has harbors the infectious organisms but is not ill. d-An incubatory carrier: person who is incubating the organism in large number but is not yet ill. 3-The pattern of disease outbreak in community a- Sporadic disease: the disease which occurs occasionally at irregular intervals in a human population. b- Endemic disease: is the disease which maintains a relatively steady low level frequency at regular interval. c- Epidemic disease: is a sudden increase in the occurrence of disease above the expected level. d- Pandemic disease: it is an increase in disease occurrence within a large population over a very wide region (usually the world) e- Zoonoses: they are infectious disease occur in animals & occasionally transmitted to human, like brucellosis & rabies. Transmission of the infectious agent 1) Airborne transmission: the agent is truly suspended in the air & travels over a meter or more from the source to the host, like droplet nuclei or dust. 2) Contact transmission: which mean the coming together or touching of the source of the infectious disease agent & the host. Direct contact actual physical interaction with the infections source (person to person). Indirect contact transmission of the infectious organism from the source to the host via an intermediate & often an inanimately object. 3) Vehicle transmission: inanimate object involved in the transmission of an infectious organism are called vehicles. In this case a single inanimate vehicle serves to spread the organism to many hosts but does not support its multiplication. Ex: surgical instruments, bedding & eating outside. 4) Vector-borne transmission: living transmitter of an infectious organisms are called Vector; like insects, ticks, mite, fleas, dogs, cats, bats,…etc. Disease:Is an abnormal condition of living pathology that is a branch of biology that involves the study of living things in their abnormal forms & conditions. Clinical stages of a disease in host: A) Acute disease: Is characterized by symptoms that usually appears quickly & become very intense & then subsides when the host immune system has overwhelmed the pathogen or its toxic products. Ex: measles, and mumps. These acute diseases have 3 stages: Incubation period: the period between entrance of pathogen & appearance of the first symptoms of a disease. Acute period: symptoms of the disease are at their peak. Ex: fever, cough in resp, diarrhea & vomiting in intestinal tract. Convalescent period: a period characterized by a sharp decline in symptoms. Latent period decline Agent enters healthy body prodromal stag First symptoms of disease highly clinical stage Characterist ic symptoms (peak) Incubation stage B) Chronic disease & persistence: symptoms are expressed over a long period of time; infectious agent here is an intracellular parasite like brucellosis & tuberculosis. Some microorganisms that persist in host, give rise to a mild symptoms or no symptoms & it’s actively shed from the host & the M.O may persist in the host for days, months or even year; like bacteria of cholera, typhoid & diphtheria. Types of disease 1)Local: a disease that restricted to a certain area in the body. 2)Focal: localized site of disease from which bacteria & their products can spread to other body parts. 3)Primary: disease caused by one microbial species. 4)Secondary: a primary disease complicated with second pathogen. 5)Mixed: disease caused by two or more microorganisms. 6)Sub clinical: that does not give rise to any detectable manifestation. 7)Latent: disease that persists in the tissue in dormant state & later becomes manifested usually when the host resistance is lowered. Pathogenicity:- First sign of recovery (disease end) The ability of M.O to cause disease. Multiple mechanisms may contribute to pathogenicity, including production of toxin stimulation of host inflammatory responses. Pathogenesis of bacterial infection includes initiation of the infections process & the mechanisms that lead to the development of signs & symptoms of disease and the Characteristics of bacteria that are pathogen include: Transmissibility Adherence to host cell Invasion of host cell Toxigenicity Ability to evade the host’s immune system Properties that is essential for pathogenicity:1. Transmissibility: The ability to grow or to be shed in body fluids or secretion. The mode & site of transmission to the new host include the following : Inhalation Ingestion Injection Sexual transmission Presence of vector 2. Infectivity: Is the ability of pathogenic M.O to initiate infection by penetrating the healthy body & overcome the first lines of defense mechanism. Therefore the infection is the process by which the parasite enters into a relationship with the host & this process depended on: a. b. c. The entrance of the parasite in the host The establishment & multiplication within the body The infection process is related to : Dosage of pathogen Phase of growth the log phase are more likely to over come host resistance than those in latent phase. 3. Virulence: Is the pathogen capacity to harm the host & its manifestation of complex host parasite relationship. Virulent organisms exhibit pathogenisity when introduce in very small number. Virulence is measured in term of the numbers of M.O or Mgm’s of toxin necessary to kill a given host. Virulence might be lost by the following: Attenuation Loss of capsule Colony variation Heat & desiccation Virulence may be enhanced by: Successive passage in lab animals Presence with other bacteria ex: C. diphtheria & St. pyogenes Conserving of virulence: Lyophilization Using enrichment culture media containing blood, store in dark at low temperature Spore forming bacteria The microbial factors contributing to infection (Virulence factors): 1. Extra cellular enzymes: Collagenase Protase Hyaloranidase Streptokinase 2. Invasiveness: It’s the ability of microorganism to enter host tissues, multiply & spread. 3. Adherence factors: If the bacteria did not adhere to the cells of tissue surface, they would be swept away by mucous & other fluids that bath the tissue surface. There for several factors play roles in adherence such as : Surface hydrophobicity & net surface charge Binding molecules on bacteria & host receptor interaction Pilli, hair like appendages 4. Antiphagocytic Factors: Some pathogens evade phagocytosis or leukocytes microbicidal mechanisms by absorbing normal host components to their surfaces. Ex.: S. aureus has surface protein A, which bind to the Fc portion of IgG. 5. Intracellular pathogenicity: Some bacteria (e.g.: M. tuberculosis) live & grow in the hostile environment within poly–morphonuclear cells, macrophages or monocytes. 6. Antigenic Heterogenecity: such as antigenic shift and drift in influenza factors. 7. Toxins: The ability of a M.O to produce toxin that contributes to the development of disease. There are two groups of toxin: EXOTOXIN ENDOTOXIN Excreted by living cell found in high concentration in fluid media Polypeptide with M.W 10000-900000 Relatively unstable toxicity often destroyed rapidly by heating over 60 °C Highly antigenic, stimulate the formation of titer of antitoxin Convert to antigenic non toxic by using heat, formalin, acid Fatal to lab animal in 1 Mg or less Integral part of M.O cell wall in G –ve bacteria L.P.S, lipid A is responsible to toxicity Relatively stable with stand heating over 60 °C for hours Do not stimulate the formation of antitoxin Do not convert Weakly toxic fatal to animals in 100 Mg/ml Do not produce fever Produce fever A. Gram + cocci Staphylococcus : The genus staphylococcus has at least 30 species. The three main species of clinical importance are: S. aureus, S. epidermidis, and S. saprophyticus. The S. aureus synthesis of the enzyme coagulase & yellow pigments & cause sever chronic infections but coagulase –ve such as S. epidermidis are non pigmented & less invasive. Morphology & Identification: Staphylococci are spherical cells about 1Mm in diameter irregular clusters. Single cocci, pairs, tetrads & chains are also seen in liquid culture. Culture of staphylococci : This bacteria grow readily on most bacteriological media under aerobic condition & at 37 C° but form pigment best at room temperature (2025°C).Colonies on solid media are round, smooth, raised & glistering. (S. aureus forms gray to deep golden yellow colonies. S. epidermidis colonies usually are gray to white on primary isolation; many colonies develop pigment only upon prolonged incubation). *Growth characteristics: Staphylococcus slowly ferments producing lactic acid but no gas. many carbohydrates, *Antigenic structure:Staphylococcus contains antigenic polysaccharides & protein as well as other substances important in cell wall structure. Peptidoglycan & polysaccharide polymer containing linked subunits provides the rigid exoskeleton of the cell wall. Teichoic acids, which are polymer of glycerol or ribitol phosphate, are linked to the peptidoglycan & can be antigenic. Toxins & Enzymes:Staphylococci can produce disease both through their ability to multiply & spread widely in tissues & through their production of many extra cellular substances; such as: Catalase : converts hydrogen peroxide into water & oxygen. Coagulase : clots oxalated or citrated plasma in the presence of a factor contained in sera. The serum factor reacts with coagulase to generate both esterrase & clotting activities in a manner similar to the activation of prothrombin to thrombin. Other enzymes : such as hyaluronidase, staphylokinase, proteinases, lipases & - lactomase. Exotoxins : - toxin degrades sphingomyelin. Leukocidin : kill exposed white blood cells. Toxic shock syndrome toxin Enterotoxin Pathology of S.aureus: The staphylococci produce disease through their ability to multiply & spread widely in tissues & also through their production of many extra cellular substances such as Exotoxins & other enzymes involved in staphylococcal invasiveness. Staphylococcal lesion is the furuncle or other localized abscess. Groups of S. aureus established in a hair follicle lead to tissue necrosis & then the formation of abscess. S. aureus also causes disease through the elaboration of toxins, without apparent invasive infection. Diagnostic laboratory tests: Culture S. aureus ferment mannitol & if the specimens contaminated with a mixed flora can be cultured on media containing 7-5% Nacl. Catalase test Coagulase test Susceptibility testing Serologic & typing tests. Staphylococcus aureus Streptococci Streptococci are a heterogenous group of bacteria & classify into 1)Streptococcus Pyogenes 2)Streptococcus agalactiae 3) Enterococcus faecalis 4) Streptococcus bovis 5) Streptococcus anginosus 6) Streptococcus pneumonia 7)Viridans Streptococcus Morphology & Identification Typical organisms: individual cocci are spherical or ovoid & are arranged in chains. The lengths of the chains vary widely & are conditioned by environmental factors. Some streptococci elaborate a capsular polysaccharide comparable to that of pneumococci; most group A, B & C strains produce capsules composed of hyaluronic acid. The cell wall contains proteins (M, T, R, antigen carbohydrates (group specific) & peptidoglycan. Culture: grow in solid media as discoid colonies & produce capsular material often give rise to mucoid colonies. Streptococcus pyogenes colony on Columbia agar with 5% sheep blood in an aerobic atmosphere enriched with 5% carbon dioxide are surrounded by a wide zone of beta-hemolysis but both Streptococcus pneumonia & Viridans Streptococcus are surrounded by a wide zone of alph-hemolysis. Growth characteristics: growth & hemolysis are aided by incubation in 10% CO2 ; grow best at 37°C but enterococci also grow in high (6.5%) NaCl in (0.1%) methylene blue & in bile esculin agar. Antigenic structure: Several antigenic substances are found, such as: Group specific cell wall antigen: this carbohydrate is contained in the cell wall of many streptococci & forms the basis of serologic grouping (Lancefield groups A-H, K-U). M protein: this substance is a major virulence factor of group A S. pyogenes & appears as hair like projections of the cell wall. T substance: this antigen has no relationship to virulence of streptococci. Unlike M protein, T substance is acid labile & heat labile. Toxins & Enzymes: More than 20 extra cellular products that are antigenic are elaborated by group A streptococci including the following : a) Streptokinase: transforms plasminogen of human plasma into plasmin. b) Streptodornase: depolymerizes DNA. c) Hyaluronidase: hyaluronidase splits hyaluronic acid & aids in spreading infecting M.O (spreading factor). d) Pyrogenic exotoxins (erythrogenic toxin) e) Diphosphopyridine nucleotidase: this protein related to the ability to kill leukocytes. f) Hemolysins: hemolyze red blood cells in vitro. The most important member of streptococcus group are. 1.St. pyogenes (group A, B hemolytic streptococci) is one of the most important bacterial pathogens & widely distributed among humans and causes many disease such as a) Scarlet fever : these disease results from a throat infection with a strain of St .pyogenes that produces an erythrogenic or rash, inducing toxin that causes shedding of the skin. Symptom after two days of incubation period, ascarlational rash appears on the upper chest & then spreads to the remainder of body. b) Streptococcal pharyngitis : it is one of the most common bacterial infections in human & usually called, strep throat. This disease is spread via droplets of saliva or nasal secretions. The incubation period in humans 2 to 4 days. The action of the strep. bacteria in the throat stimulates an inflammatory response & inflammatory exudates consisting of cells & fluid deposited in the surrounding tissue, with discomfort, fever, headache, redness, edema & enlargement of the lymph node in the throat, in the absence of complications, the disease is self-limited & disappears within a week. c) Post streptococcal disease: Rheumatic fever: is an auto immune disease characterized by inflammatory lesions involving the heart valves, joints, subcutaneous tissues & CNS. Usually occur after streptococcal sore throat infections & usually infect children of age 6-15 years age. Glomerulonephritis : is an inflammatory disease of renal glomeruli & membranous structure within the kidney when the blood is filtered. Damage probably results from the deposition of Ag-Ab complex in the glomeruli. The effected person exhibits edema, fever, hypertension & hematuria, occur after streptococcal infection. No specific therapy once kidney damage has occurred. Diagnostic laboratory tests: Culture: blood cultures will grow hemolytic group A streptococci within hours or a few days. Incubation in 10% CO2 often speeds hemolysis because oxygen that inactivates streptolysin O. Antigen detection tests: by using several commercial kits are available for rapid detection of group A streptococcal Ag from throat swabs. Serological tests: arise in the titer of Ab to group A streptococcal Ag can be estimated. 2) Str. pneumonia Form a small round colony & are ــhemolytic on blood agar growth is enhanced by 5-10% CO2 & it is G+ve diploid found in the upper respiratory tract. The disease usually occurs only in the individuals with predisposing factors such as viral infections of the respiratory tract, physical injury to the tract, alcholism and diabetis. The pathogenesity is due to the rapid multiplication of the bacteria in alveolar spaces. The alveoli fill with blood cells, fluid & become inflamed. The sputum is often rust colored because the blood is coughed. Laboratory tests Culture: on culture media form a small round colony at first dome-shaped & later developing a central plateau with an elevated rim. On blood agar incubation in 10% CO 2 often speeds ــhemolysis. Smears: give single cocci or pairs rather than definite chains or lancet-shaped diplococci. Quelling Reaction: when pneumonococci of a certain type are mixed with specific antipolysaccharide serum or with polyvalent antiserum on a microscope slide, the capsule swells markedly. Biochemical reaction: on solid media the growth of pneumococci is inhibited around a disk of optochin while St. viridans is not inhibited by optochin. The pnemococci lyses in a few minutes when exposure to bile (10%) or sodium deoxycholate (2%) is added to a broth culture or suspension of organisms at neutral PH. With age, the organisms rapidly become G -ve & tend to lyses spontaneously. capsule G+ve diploid