Amino acid metabolism
advertisement
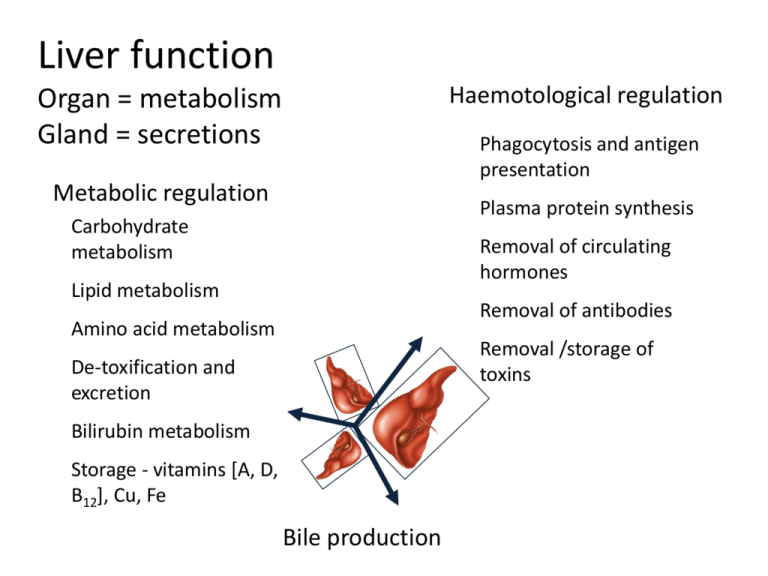
Liver function Haemotological regulation Organ = metabolism Gland = secretions Phagocytosis and antigen presentation Metabolic regulation Plasma protein synthesis Carbohydrate metabolism Removal of circulating hormones Lipid metabolism Removal of antibodies Amino acid metabolism Removal /storage of toxins De-toxification and excretion Bilirubin metabolism Storage - vitamins [A, D, B12], Cu, Fe Bile production Carbohydrate metabolism Glycogenesis Glycogenolysis Gluconeogenesis IMPAIRMENT Hypoglycaemia Glucose Intolerance http://static.howstuffworks.com/gif/diabetes-glucose-regulation.gif Lipid Metabolism •Lipoprotein synthesis •Oxidation of fats •Synthesis of cholesterol, phospholipids •Catabolism of steroids IMPAIRMENT Altered lipid profiles 2O Hyperaldosteronism →↑BP ↓K ↑pH 2O Hypercorticolism = Cushing’s disease Gonadal dysfunction → ∆ oestrogen:testestorone http://www.medscape.com/pi/editorial/clinupdates/2001/608/art-cu02.fig04.gif Amino acid metabolism • Deamination and transamination of amino acids • Removal of ammonia • Synthesis of amino acids Hepatic encephalopathy IMPAIRMENT Hypoproteinaemia Source: seqcore.brcf.med.umich.edu/ mcb500/aametov.gif Synthesis of hormones and plasma proteins……. • • • • • • Insulin-like growth factor (IGF-1) → stimulated by pituitary growth hormone Thrombopoietin → platelet production Angiotensinogen (α-2-globulin) → hydrolysed by renin to angiotensin [reninangiotensin-aldosterone system (RAAS)] Heparin Albumin Extrinsic pathway clotting factors →I (fibrinogen), II (Prothrombin), IV, V, VI, and VII http://www.biosbcc.net/doohan/sample/images/blood%2520cells/clottingcascade IMPAIRMENT Clotting disorders, ↓ osmotic pressure Bile production …. Water Bile Acids e.g. taurocholic and glycocholic acid Electrolytes Cholesterol Phospholipids Bilirubin IMPAIRMENT • Malabsorption of fats and fat soluble vitamins • Jaundice http://sbsweb.bangor.ac.uk/images/bsx1016/sm_liver_position Detoxification – refer to Biochemistry and PK done in years 2/3. Phase I = modify Phase II = conjugate IMPAIRMENT Reduced drug metabolism, reduced protein binding of drugs http://www.aspartame-detox.info/images/brain-01.jpg Filtration – Reticuloendothelial system Blood filtration, phagocytosis of bacteria and other particulate matter IMPAIRMENT Exposure to bacteria and other particles Source :www.bu.edu/histology/ i/15204loa.jpg Symptoms of liver disease • Most symptoms non specific - anorexia, malaise, fatigue, fever • ↓ general health • cirrhotic habitus = wasted extremities plus protuberant abdomen with ascites • Generalised pruritus (itchiness) – due to retention of bile salts • Xanthelasma (fat build up under skin surface), xanthomas • Pale stools – lack of bile • Which of these is most specific? akimichi.homeunix.netXanthom a disappearance Document 272 x 324 pixels - 55k - gif Disorders of coagulation/circulation • ↑ bleeding and bruising • ↑ prothrombin time (PT) → extrinsic clotting pathway (Prothrombin ratio (PR) and international normalized ratio (INR) are derived measures of PT). • Thrombocytopaenia (↓platelets) • Dysfibrinogenaemia (altered fibrinogen function) • Portal hypertension → endothelial stretching and shear stress → ↑ NO → systemic vasodilation = hyperdynamic circulation • Hepatopulmonary syndrome = pulmonary vasodilation → ↑blood flow (ventilation-perfusion mismatch) → arterial desaturation • Cyanosis and clubbing → enlargement of distal fingers and toes. Due to vasodilation? http://www.nlm.nih.gov/medlineplus/ency/images/ency/fullsize/18127.jpg Liver disease? http://upload.wikimedia.org/wikipedia/en/thumb/e/e0/Gollum.PNG/220px-Gollum.PNG Other changes • ↑ parotid salivary gland → fatty infiltation • Gynecomastia (mammary gland development in males), testicular atrophy, impotence • Amenorrhoea (absence of menstrual period) • Erythema (redness of skin) – build up of unmetabolised wastes in body http://www.sciencephoto.com/images/download_lo_res.html?id=771500153 Jaundice • Icterus (icteric) • Accumulation of bilirubin = hyperbilirubinaemia • Skin, conjuctiva, mucous membranes • Dark urine from renal excretion of bilirubin http://www.modulomedico.com/fotos/imgJaundiceBig.jpg Serum chemistry/diagnostic testing Bilirubin •Breakdown product of haemoglobin •Globin = protein •Heme = iron containing → biliverdin (green bruising) → bilirubin → yellow (bruising/bile) •Bilirubin → conjugated with glucuronides in liver •Excreted in bile •Can be measured in the unconjugated (indirect) or conjugated (direct) form •Relatively insensitive indicator of liver disease Source:web.indstate.edu/thcme/ mwking/hemedegradation.jpg From Beckett - Lecture Notes : Clinical Biochemistry 7th ed 2005 From Swaminathan – Handbook of Clinical Biochemistry 2004 Aminotransferases (ALT and AST) Transaminase enzymes (aminotransferases) → reversible transfer of an amino group between two a-keto acids. • Alanine aminotransferase = liver cytosol (ALT) • Aspartate aminotransferase = liver and other tissues (AST) • Reasonably sensitive indicators of liver disease, ALT >> AST Source: http://www.np.edu.sg/~dept-bio/biochemistry/aab/topics/asptrans.gif Alterations in ALT and AST Mild elevations(<100U/L) • Fatty liver/non-alcoholic steatohepatitis (fatty degeneration) • Chronic viral hepatitis Moderate elevations(100-300 U/L) • Acute or chronic hepatitis • Alcoholic hepatitis • Mild/moderate inflammation High elevated(>300 U/L) • Acute viral hepatitis • Hepatic necrosis → drugs or toxins • Ischemic hepatitis /circulatory shock. VALUES CAN BE 500-1500 U/L • Values >3000 U/L- toxic necrosis, or severe hypoxia AST/ALT ratio • • • Significant overlap between different conditions BUT > 2 suggestive alcoholic liver disease (if ALT < 500 U/L) < 1 viral hepatitis can ↑ratio as fibrosis and cirrhosis develop Alkaline phosphatases (ALP) •ALP = hydrolase →removes phosphate groups •Present in bile canaliculi, bone and placenta •↑ sensitivity for hepatobiliary disease •↓ specificity for hepatobiliary disease •Due to its numerous isoenzymes, its presence in nonhepatic tissues, and its sensitivity to drug induction Increases in liver ALP • Cholestasis, cholecystitis, cholangitis, cirrhosis, hepatitis, fatty liver, liver tumour, liver metastases, drug intoxication • Drugs e.g. verapamil, carbamazepine, phenytoin, erythromycin, allopurinol, ranitidine • ↑ → enhanced synthesis rather than hepatocytic leakage • ↓ ≠ clinically significant • If source ↑ ALP is not clear check other liver enzymes Gamma glutamyl transpeptidase (GGT) • GGT → hydrolysis of gamma-glutamyl peptide bonds • Biliary enzyme → obstruction of biliary tract + damage to biliary capillaries • Easily induced (alcohol, drugs) → disproportionately ↑ in alcoholic liver disease • Can be elevated in other diseases e.g. CHD, MI, COPD, pancreatitis, renal disease Patterns of enzyme alterations ALT Hepatocellular ≥ 2x upper limit of normal Cholestasis Normal (bile flow obstruction) Mixed disease ↑ ALP Normal ALT/ALP ratio ≥5 ≥ 2x ULN ≤2 ↑ 2-5 Ramachandran and Kakar J Clin Pathol 2009;62;481-492 Histological patterns in drug-induced liver disease ERCP = Endoscopic Retrograde Cholangiopancreatography From Beckett - Lecture Notes : Clinical Biochemistry 7th ed 2005 From Beckett - Lecture Notes : Clinical Biochemistry 7th ed 2005 Other tests • Haematology (anaemia, RBC parameters) • Clotting tests (PT) NOTE – these are vitamin K-dependent clotting factors • • • Lipid tests (total cholesterol, HDL, LDL, triglycerides) Biochemistry (albumin, glucose) Serology -Hepatitis virus -Antimitochondrial antibody (present in >90% of biliary cirrhosis cases) -Antinuclear factor- inflammatory marker -Antismooth muscle antibody-inflammatory marker -Alpha fetoprotein-hepatic carcinoma marker • Functional tests -Clearance tests (caffeine, bromosulphthalein), Elimination tests (galactose) • Imaging procedures -Abdominal radiographs -US, NMR, CT -Direct biliary visualisation → contrast studies • Liver Biopsy - Percutaneous -Surgical Drug Induced Liver Disease (DILD) • > 1000 drugs → DILD • ↑Hz drug withdrawal from the market Reference Hughes et al. Use of laboratory test data: a process guide and reference for health care professionals. 2nd Ed, PSA, 2009. Drug Induced Liver Disease (DILD) • Consider wherever altered liver function tests • However – Broad range of drugs – Wide variation in hepatic injury caused Drug Induced Liver Disease (DILD) • Types of hepatic injury – – – – – – Hepatitis Cholestasis Mixed Fibrosis Granulomatous lesions Neoplasms http://www.health-writings.com/img/mk/drug-induced-liver-disease/drugs_MIC062ML.jpg Drug induced hepatic failure http://www.path.cam.ac.uk/Normal/AR_Alimentary/LV_Liver/N_AR_LV_02.jpg http://mayoresearch.mayo.edu/mayo/research/nyberg_lab/images/histology.jpg Drug Induced Liver Disease (DILD) • • • • • Other changes (functional) Enzyme induction and inhibition Dietary /other deficiencies e.g. cysteine, Vit K Steatosis = fatty change Phospholipidosis Drug Induced Liver Disease (DILD) • Intrinsic – Dose related – Occurs within few days of use – Related to drug or toxic metabolite of drug – Known/reported/expected • Idiosyncratic – Unexpected – Variable latency – Not usually dose related Intrinsic - usually dose related: Drug Reason Paracetamol Hepatocellular necrosis Amiodarone Chronic steatosis- due to total dose over time Cyclosporine Cholestasis due to toxic serum levels Methotrexate Elevated aminotransferase and fibrosis after single large dose Niacin Vascular injury after prolonged administration Oral Contraceptives Hepatic tumour after prolonged administration Tetracycline Steatosis after large total dose and renal dysfunction Idiosyncratic - usually hypersensitivity Drug Reason Isoniazid, diclofenac, nefazodone, trazodone, venlafaxine etc Hepatocellular necrosis CPZ, oestrogen, macrolides Cholestasis Phenytoin, sulphamethoxazole Immune reaction Diltiazem, sulphonamides Granulomatous Hepatitis Didanosine, tetracycline, valproic acid Steatosis Methotrexate Fibrosis Amoxycillin/Clavulonic Acid Cholestatic injury Factors affecting DILD • • • • • • • • • Age Gender Genetic factors Nutritional status Renal function Dose and duration Alcohol Cigarette smoking Other conditions- Hep C, HIV, RA Paracetamol toxicity • Paracetamol = #1 drug → calls to poisons information centres in Australia and NZ. 1 • Paracetamol = #1 drug overdose → hospital presentation and admission. 2,3 • Hepatic failure and death → uncommon outcomes • #1 cause of acute fulminant hepatic failure in Western countries.4 1. Buckley N, Eddleston M. Paracetamol (acetaminophen) poisoning. Clin Evid 2005; (14): 1738-1744. 2. Dart RC, Erdman AR, Olson KR, et al. Acetaminophen poisoning: an evidence-based consensus guideline for out-of-hospital management. Clin Toxicol (Phila) 2006; 44: 1-18. 3. Linden CH, Rumack BH. Acetaminophen overdose. Emerg Med Clin North Am 1984; 2: 103-119. 4. Ostapowicz G, Fontana RJ, Schiødt FV, et al. Results of a prospective study of acute liver failure at 17 tertiary care centers in the United States. Ann Intern Med 2002; 137: 947-954. Phases of paracetamol hepatotoxicity PHASE 1 (0-24 H) •Asymptomatic •Anorexia •Nausea or vomiting •Malaise •Subclinical rise in serum transaminases levels begins at about 12 hours postingestion PHASE 3 (72-96 H) •Centrilobular hepatic necrosis with continued abdominal pain •Jaundice •Coagulopathy •Hepatic encephalopathy •Nausea and vomiting •Renal failure •Fatality PHASE 2 (18-72 H) •Right upper quadrant abdominal pain, anorexia, nausea, vomiting •Continued rise in serum transaminases levels •Admitted to hospital PHASE 4 (4 D TO 3 WK) •Complete resolution of symptoms •Complete resolution of organ failure Paracetamol toxicity • Toxicity when GSH reserves overwhelmed by N-acetyl-pbenzoquinone imine (NAPQi) • ± gastric lavage and activated charcoal • Treatment → IV N-acetylcysteine http://drugdiscoveryopinion.com/images/paracetamol_metabolism.jpg Management plan- dose thresholds for NAC treatment ≠ serum readings <4 hours of poisoning Frank F S Daly, John S Fountain, Lindsay Murray, Andis Graudins and Nicholas ABuckley(2008).Guidelines for the management of paracetamol poisoning in Australia and New Zealand — explanation and elaboration. A consensus statement from clinical toxicologists consulting to the Australasian poisons information centres. MJA 2008; 188 (5): 296-302. Management Plan Source- Frank F S Daly, John S Fountain, Lindsay Murray, Andis Graudins and Nicholas ABuckley(2008).Guidelines for the management of paracetamol poisoning in Australia and New Zealand — explanation and elaboration. A consensus statement from clinical toxicologists consulting to the Australasian poisons information centres. MJA 2008; 188 (5): 296-302. Source: Frank F S Daly, John S Fountain, Lindsay Murray, Andis Graudins and Nicholas A Buckley(2008).Guidelines for the management of paracetamol poisoning in Australia and New Zealand — explanation and elaboration. A consensus statement from clinical toxicologists consulting to the Australasian poisons information centres. MJA 2008; 188 (5): 296-302. Source: Frank F S Daly, John S Fountain, Lindsay Murray, Andis Graudins and Nicholas A Buckley(2008).Guidelines for the management of paracetamol poisoning in Australia and New Zealand — explanation and elaboration. A consensus statement from clinical toxicologists consulting to the Australasian poisons information centres. MJA 2008; 188 (5): 296-302. Source- Frank F S Daly, John S Fountain, Lindsay Murray, Andis Graudins and Nicholas ABuckley(2008).Guidelines for the management of paracetamol poisoning in Australia and New Zealand — explanation and elaboration. A consensus statement from clinical toxicologists consulting to the Australasian poisons information centres. MJA 2008; 188 (5): 296-302. Management Plan cont… Management Plan cont… • Monitoring of liver function • Post –discharge patient education • Referral to Psychologist if needed Kava (Piper methysticum) • Kava = plant native to South Pacific Islands • Western society → herbal remedy anxiety • Kavalactones = active components -6 KL ~ 95% of the activity • Anxiolytic effect ~ benzodiazepines -few side effects -limited cognitive and motor impairment • Kava → hepatotoxicity e.g. hepatitis, cirrhosis, fulminant liver failure, death • Banned in many countries • Australia → voluntary recall 2002 Isolated Perfused Rat Liver (IPRL) PUMP Perfusate • Kavalactone • 95% O2/5% CO2 • Taurocholic acid • Krebs-Henseleit (KH) buffer Inferior Vena Cava Hepatic Portal Vein 37°C 10 µg/mL Kavain for 2 hours is hepatotoxic in IPRL studies Light Microscopy Scanning Electron Microscopy Control Liver Following Kavain Treatment Fu (2008) World J Gastroenterology 14: 541546 Membranes and electron dense structures Distorted cell nuclei Autophagosome Whirled ER surrounding mitochondrion Advice for case studies • Common things occur commonly. • Uncommon things don’t. • When you have eliminated the impossible, whatever remains, however improbable, must be the truth. Sherlock Holmes - The Sign of the Four (1890) Case Study #1 – history and signalment • • • • • • 68 YO male retired labourer Lethargy but no pain BW ↓19kg in the last 3 months Eating normally up to last 3 weeks Dark urine and pale stools ‘Moderate’ drinker throughout lifetime Clinical findings • Jaundice • Weakness • Palpable, non-tender mass in upper RHS abdominal quadrant Serum chemistry • • • • Analyte Result Reference Range Units Albumin 32 36-47 g/L ALP 632 40-125 U/L ALT 55 10-40 U/L Total bilirubin 90 2-17 µmol/L GGT 200 10-55 U/L Bilirubin predominantly conjugated ↑↑ ALP and GGT Predominantly cholestasis Pancreatic tumour obstructing common bile duct Case Study #2 – history and signalment • • • • 21 YO female student Flu-like symptoms for 2 days Condition deteriorating – dark urine, vomiting Recently returned from long holiday in Asia Clinical findings • Jaundice • Temperature 38.6oC (36.5-37.5 oC) • Liver enlarged and tender Serum chemistry • • • • • Analyte Result Reference Range Units Albumin 40 36-47 g/L ALP 190 40-125 U/L ALT 560 10-40 U/L Total bilirubin 110 2-17 µmol/L GGT 60 10-55 U/L Bilirubin predominantly conjugated ↑↑ ALT Predominantly hepatocellular Any other tests? Serology - high Hepatitis A titre Case Study #3 – history and signalment • • • • 48 YO male gardener Fatigue BW ↓8 kg over last 4 months Denies any history of hepatitis, alcohol use, family history of liver disease, exposure to hepatotoxins Clinical findings • No abnormalities detected Serum chemistry • • • • Analyte Result Reference Range Units Albumin 20 36-47 g/L ALP 56 40-125 U/L ALT 16 10-40 U/L Total bilirubin 13 2-17 µmol/L GGT 24 10-55 U/L Any other tests? PT = 18 s (10-13 s) IM dose 10 mg Vitamin K returned PT to 12 s < 48 hours Serology and endoscopy → Coeliac disease → interfering with Vit K and protein absorption Case Study #4 – history and signalment • 13 YO male • Muscle pain and feeling hot for 2 days • Eaten little over this time Clinical findings • Jaundice • Temperature 38.3oC • No abdominal pain or swelling Serum chemistry • • • • • • • • • Analyte Result Reference Range Units Albumin 45 36-47 g/L ALP 180 40-125 U/L ALT 30 10-40 U/L Total bilirubin 60 2-17 µmol/L GGT 35 10-55 U/L Bilirubin 90% unconjugated Any other tests? Haematology – RBC and reticulocyte count normal Gilbert’s syndrome = most common hereditary hyperbilirubinaemia Familial autosomal dominant in 2-3% men ↓ activity of the glucuronyltransferase → ↓ bilirubin conjugation Exposed by caloric restriction while ill with cold ↑ ALP but GGT normal ?? Raised ALP from bone turnover with onset of puberty Case Study #5 – history and signalment • • • • • 36 YO female lawyer Very stressful job Working 12 hour days striving for promotion Feeling run down Annual blood test Clinical findings • No abnormalities detected Serum chemistry • • • • Analyte Result Reference Range Units Albumin 42 36-47 g/L ALP 130 40-125 U/L AST 180 8-42 IU/L ALT 70 10-40 U/L Total bilirubin 15 2-17 µmol/L GGT 380 10-55 U/L Any other tests? Haematology – leukopaenia (↓WBC), macrocytosis (↑MCV) Toxic effects on bone marrow? Finally admits drinking one bottle wine per day over lunch and after work • Quit job. Quit drinking • 3 months later – ALT 28 IU/L, GGT 50 IU/L, ALP 54 IU/L Case Study #6 – history and signalment • 26 YO male • Admitted to hospital with 5-day history of excruciating abdominal pain radiating up back • Patient reports persistent nausea and vomiting Clinical findings • Vital stable signs on admission • No fever • Extreme reaction to abdominal palpation Serum chemistry • • • • • • Analyte Result Reference Range Units Albumin 34 36-47 g/L ALP 110 40-125 U/L ALT 24 10-40 U/L Total bilirubin 16 2-17 µmol/L GGT 23 10-55 U/L Any other tests? Blood test normal Serum amylase normal US and CT normal Requested ongoing opiates for pain control Opiates withdrawn → patient checked out → continue search for opiates elsewhere Summary • • • • • • • • • Variable interspecies anatomy Histological structure open to interpretation Metabolic functions (glucose, protein, fat) Glandular function (produces bile) Jaundice = hyperbilirubinaemia Bilirubin is a product of heme catabolism Pre-hepatic (unconjugated) Hepatic (unconjugated + conjugated – glucuronic acid) Cholestatic/obstructive → intra/post-hepatic (conjugated) • Diagnosis – symptoms, laboratory, imaging, biopsy Any Questions?