Tests for Cholestasis & Necrotic/Inflammatory Processes in the Liver
advertisement

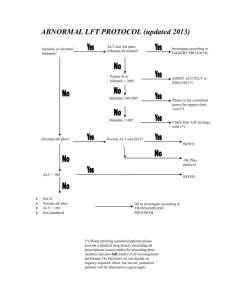
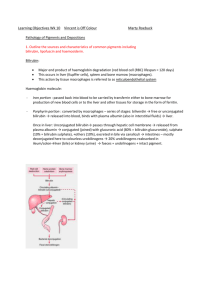
Tests for Cholestasis & Necrotic/Inflammatory Processes in the Liver Cholestasis Cholestasis is caused by obstruction within the liver (intrahepatic) or outside the liver (extrahepatic). The obstruction causes bile salts, the bile pigment bilirubin, and fats to accumulate in the blood stream instead of being eliminated naturally. (1) Necrosis/Inflammation Hepatitis is the Latin word for liver inflammation. It is characterised by the destruction of a number of liver cells and the presence of inflammatory cells in the liver tissue. (2) http://www.netdoctor.co.uk/diseases/facts/hepatitis.htm Diagnosis Intrahepatic cholestasis: A history of hepatitis or heavy drinking, recent use of certain drugs, and symptoms like ascites and splenomegaly. (1) Extrahepatic cholestasis: Pain or rigidity in the gallbladder or pancreas. (1) Blood tests and liver function tests: Reveal the pattern and extent of liver injury, indicate functional abnormalities, and establish the cause of the condition. (1) Inflammation of the hepatic cells results in elevation in the alanine aminotransferase (ALT), aspartate aminotransferase (AST) and possibly the bilirubin. Inflammation of the biliary tract cells results predominantly in an elevation of the alkaline phosphatase. (3) Elevated levels of: - Alanine Aminotransferase (ALT): ALT is the enzyme produced within the cells of the liver. The level of ALT is increased in conditions where cells of the liver have been inflamed or undergone cell death. As the cells are damaged, the ALT leaks into the bloodstream leading to a rise in the serum levels. Any form of hepatic cell damage can result in an elevation in the ALT. (3) http://www.gastromd.com/lft.html More than 3 times greater than normal may indicate cholestasis. (1) (Reference Range: 5-40 IU/L) (4) - Aspartate Aminotranferase (AST): Can indicate hepatocellular disease (viral hepatitis or cancer). (1) However, it is less specific and may be elevated in other conditions such as a MI. Although AST is not a specific for liver as the ALT, ratios between ALT and AST are useful to physicians in assessing the etiology of liver enzyme abnormalities. (1) (Reference Range: 10-40 IU/L) (4) - Alkaline Phosphatase (ALP): This enzyme is in the cells lining the biliary ducts of the liver. (4) ALP levels in plasma will rise with primary biliary cirrhosis, alcoholic hepatitis, large bile duct obstruction or intrahepatic cholestasis. (1) ALP is also present in bone and placental tissue, so it is higher in growing children and elderly patients with Paget's disease. (4) (Reference Range: 30-120 IU/L) (4) - Gamma Glutamic Transpeptidase (GGT): Although reasonably specific to the liver and a more sensitive marker for cholestatic damage than ALP, GGT may be elevated with even minor, sub-clinical levels of liver dysfunction. It is used to confirm that ALP is of hepatic etiology. (Reference Range: 0-51 IU/L) (4) o 5' nucleotidase is another test specific for cholestasis or damage to the intra or extrahepatic biliary system. In some laboratories, it is used as a substitute for GGT for ascertaining whether an elevated ALP is of biliary or extra-biliary origin. (4) - Bilirubin A. Total Bilirubin: Increased total bilirubin causes jaundice, and can signal a number of problems: (Reference Range 2-14 IU/L) (4) 1. Prehepatic: Increased bilirubin production. This can be due to a number of causes, including hemolytic anemias and internal hemorrhage. (4) 2. Hepatic: Problems with the liver, which are reflected as deficiencies in bilirubin metabolism (e.g. reduced hepatocyte uptake, impaired conjugation of bilirubin, and reduced hepatocyte secretion of bilirubin). Some examples would be cirrhosis and viral hepatitis. (4) 3. Posthepatic: Obstruction of the bile ducts, reflected as deficiencies in bilirubin excretion. (Obstruction can be located either within the liver or in the bile duct.) (4) B. Direct Bilirubin: Looking at the levels of direct bilirubin narrows the diagnosis down further. (Reference Range 0-4 IU/L) (4) If direct (i.e. conjugated) bilirubin is normal, then the problem is an excess of unconjugated bilirubin, and the location of the problem is upstream of bilirubin excretion. Hemolysis, viral hepatitis, or cirrhosis can be suspected. (4) If direct bilirubin is elevated, then the liver is conjugating bilirubin normally, but is not able to excrete it. Bile duct obstruction by gallstones or cancer should be suspected. (4) http://en.wikipedia.org/wiki/Liver_enzymes - Albumin: When the liver has been chronically damaged, the albumin may be low. This would indicate that the synthetic function of the liver has been markedly diminished. Such findings suggest a diagnosis of cirrhosis. (3) http://www.gastromd.com/lft.html Non-invasive procedures: Ultrasound, computed tomography scans (CT) and magnetic resonance imaging (MRI) can provide more detailed information about the source of the obstruction. (1) If these procedures do not provide the information needed to make a diagnosis of cholestasis, one of these procedures may be performed: Direct cholangiography: an x-ray map of the bile ducts, enhanced by the use of contrast dye. (1) Percutaneous transhepatic cholangiography: used to identify obstructions that impede the flow of bile from the liver to the GIT. Takes x-ray images of the bile ducts after a contrast dye has been injected by a needle passed directly into a hepatic duct. (1) Endoscopic retrograde cholangiopancreatography (ERCP): Uses a special dye to outline the pancreatic and common bile ducts and highlights the position of any obstruction; a special tube with a light transmitter is inserted into the duct and a series of x-ray images are taken. (1) http://medical-dictionary.thefreedictionary.com/Obstruction+of+bile+duct 1.http://www.healthatoz.com/healthatoz/Atoz/common/standard/transform.jsp?request URI=/healthatoz/Atoz/ency/cholestasis.jsp 2. http://www.netdoctor.co.uk/diseases/facts/hepatitis.htm 3. http://www.gastromd.com/lft.html 4. http://en.wikipedia.org/wiki/Liver_enzymes Plagiarism sources: 45.3%