CARTILAGE
advertisement
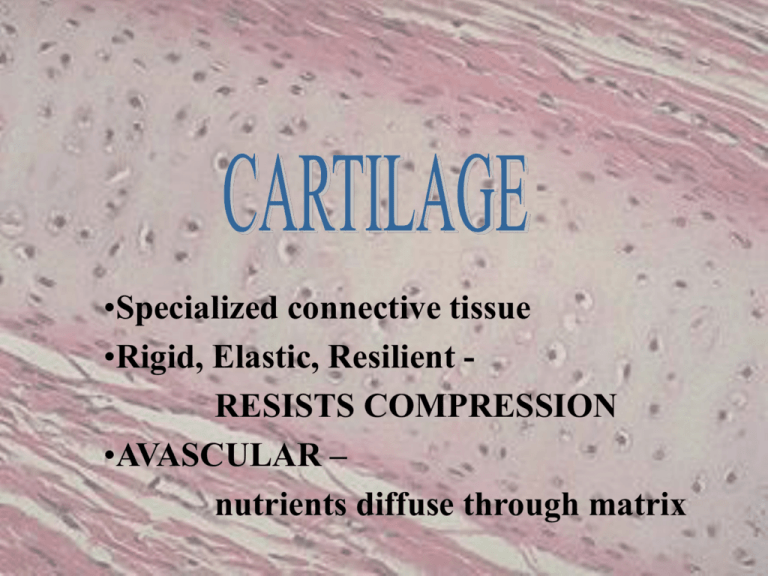
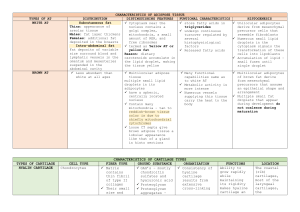
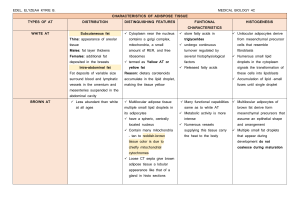
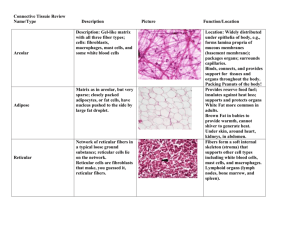
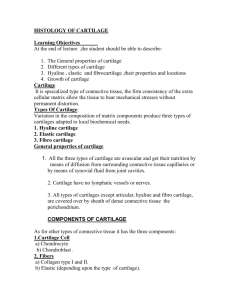
•Specialized connective tissue •Rigid, Elastic, Resilient RESISTS COMPRESSION •AVASCULAR – nutrients diffuse through matrix Hundreds of Eyes Staring Back at YOU! PERICHONDRIUM • Dense irregularly arranged connective tissue (type I collagen) • Ensheaths the cartilage • Houses the blood vessels that nourish chondrocytes CHONDROBLAST • Progenitor of chondrocytes • Lines border between perichondrium and matrix • Secretes type II collagen and other ECM components • Chondroblasts build CHONDROCYTE • Mature cartilage cell • Reside in a space called the lacuna • Clear areas = Golgi and lipid droplets • Chondrocytes completely fill their lacunae • RER and euchromatic nuclei • Synthetically active, secrete matrix N RER Cartilage matrix MATRIX • Provides the rigidity, elasticity, & resilience • FIBERS – Collagenous and elastic • GROUND SUBSTANCE – Glycosaminoglycans (chondroitin sulfates, keratin sulfate, hyaluronic acid) – Proteoglycans: GAGs + core protein – Water • Basophilic • Territorial matrix - high [ ] of sulfated proteoglycans CARTILAGE GROWTH • Appositional – Increasing in WIDTH; chondroblasts deposit matrix on surface of pre-existing cartilage • Interstitial – Increasing in LENGTH; chondrocytes divide and secrete matrix from w/in lacunae TYPES OF CARTILAGE • HYALINE • ELASTIC • FIBROUS HYALINE CARTILAGE • FUNCTION – Support tissue and organs – Model for bone development • MATRIX – Type II collagen (thin fibrils) – Chondroitin sulfate, keratin sulfate, hyaluronic acid – Water • LOCATION – Tracheal rings, nasal septum, larynx, articular surfaces of joints ELASTIC CARTILAGE • FUNCTION – Support with flexibility • MATRIX – Normal components of hyaline matrix plus ELASTIC fibers • LOCATION – External ear, external auditory canal, epiglottis • STAINS – Elastic fibers stain BLACK with Weigert stain perichondrium FIBROCARTILAGE Orcein van Giesen Elastic stain - fibrocartilage - reddish brown hyaline cartilage - yellow FIBROCARTILAGE • FUNCTION – Support with great tensile strength • MATRIX – Type I collagen Oriented parallel to stress plane • LOCATION – Intervertebral disks, pubic symphysis FIBROCARTILAGE • Chondrocytes align between collagen fibers • Collagen fibers lie parallel to lines of stress How many types of cartilage do you see? SYNOVIAL (DIARTHRODIAL) JOINTS JOINT DEFINITIONS • SYNOVIAL CAVITY – Fluid filled space b/t 2 bones • SYNOVIAL FLUID – Water and GAGs; provides nutrients for cartilage • SYNOVIAL MEMBRANE – Continuous with the perichondrium SYNOVIAL “MEMBRANE” Not a true membrane Why? • Specialized secretory CT • Loose (areolar) CT • Formed by layers of collagen and fibroblasts • Highly vascular • No perichondrium • Joint capsule composed of DIACT • Why does the cartilage at the joint stain so acidophilic (i.e. pink)? Question 1 A Panel C is a low magnification micrograph of the tissue shown in Panel B. Provide the letter or letters (A and/or B) (or none) of the panel to which the following apply. normally calcified vascularized collagen type II cells capable of division matrix contains proteoglycans lacunae present C B C A Questions 2 and 3: 2. The three tissues shown have all of the following properties in common EXCEPT: a. b. c. d. B They contain capillaries. They contain proteoglycans. They can increase in size by interstitial growth. They can increase in size by appositional growth. 3. Which tissue is the most highly specialized to resist compression? a. A b. B c. C Question 4 4. What cartilage nourishing tissue is missing at the interface shown? a. Synovial fluid b. Perichondrium c. Synovial membrane d. Chondroblasts