08_Assessment of urinary system
advertisement

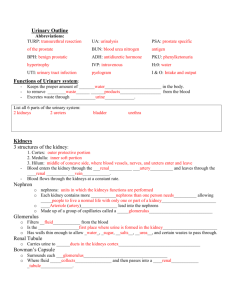
Assessment of the Renal/Urinary System Lectures Petrenko N., MD, PhD Elsevier items and derived items © 2006 by Elsevier Inc. Anatomy and Physiology Review • Kidneys • Ureters • Urinary bladder • Urethra Location and External Anatomy of Kidneys • Located retroperitoneally • Lateral to T12–L3 vertebrae • Average kidney – 11-13 cm tall, 5-7 cm wide, 3 cm thick – Bean-shaped, brownish-red structures, – right lower than left • Renal capsule surrounds the kidney • Hilus – On concave surface – Vessels and nerves enter and exit Urinary anatomy and function • http://www.youtube.com/watch?v=qxb2_d9il Ew&NR=1&feature=fvwp A. Regions 1. Renal parenchyma a. Cortex • Glomeruli, proximal and distal convoluted tubules, cortical collecting ducts, and adjacent peritubular capillaries. b. Medulla • Pyramids (8- 18 pyramids/ kidney) 2. 2. Renal Pelvis - it is the concave portion of the kidney through which the renal artery enters and the renal vein exits - composed of afferent arteriole and efferent arteriole B. Nephrons - Functional units of kidney: a) Glomerulus b) Bowman’s capsule c) Proximal tubule d) Distal tubule e) Loop of Henle f) Collecting ducts Urinary anatomy and function • http://www.youtube.com/watch?v=aQZaNXNr oVY&feature=related C. D. Calyx • Minor calyx- 4-13 minor calices • Major calyx- 2-3 major calices Glomerulus 3 filtering layers: 1. Capillary endothelium 2. Basement membrane 3. Epithelium General Specific Function: Function: • Urine formation • Excretion of waste products • Regulation of electrolyte excretion • Regulation of acid excretion • Regulatory • Regulation of water excretion • Auto regulation of blood pressure • Secretory • Regulation of red blood cell production • Renal clearance • Vitamin D synthesis • Secretions of prostaglandins • Urine storage • Bladder emptying • Excretory Ureters • Fibromuscular tube that connect each kidney to the bladder • Narrow, muscular tubes, 24-30 cm long – 3 narrowed areas: • Ureteropelvic junction • Ureteral segment • Ureterovesical junction - prevents reflux of urine Urinary Bladder • Muscular, hollow- sac located just behind the pubic bone • 300- 600 ml of urine 4 layers of the urinary bladder: 1. Adventitia- outermost layer 2. Detrusor- beneath the adventitia 3. Lamina Propria- interface between detrusor and urethelium. 1. Urothelium- innermost layer Urethra • Small tube leading from the floor of urinary bladder • 1.5 inch in length in females & 8 inch in male • Function: passageway for urine & semen Renal/Urinary System Changes Associated with Aging • Reduced renal blood flow causing kidney loss of cortical tissue by 80 years of age • Thickened glomerular and tubular basement membranes, reducing filtrating ability • Decreased tubule length • Decreased glomerular filtration rate • Nocturnal polyuria and risk for dehydration • Tubular changes are shown by a decreased ability to concentrate urine, resulting in nocturia (increased need to urinate at night). • The excretion and regulation of sodium, acids, and bicarbonate remain effective but are less efficient because homeostasis is slower. • Hormonal changes include a decrease in renin secretion, aldosterone levels, and activation of vitamin D. Renal/Urinary System Changes Associated with Aging • Urinary Changes • Changes in the elasticity of the detrusor muscle may cause decreased bladder capacity and a decreased ability to retain urine. • The sensation of the urge to void may cause immediate bladder emptying because the urinary sphincters lose muscle tone and often become weaker with age. • In women, weakening muscles shorten the urethra, which contributes to incontinence. • In men, an enlarged prostate gland causes difficulty in starting the urine stream and may cause urinary retention. Assessment Techniques • Family history and genetic risk assessment • Demographic data and personal history • Diet history • Socioeconomic status • Current health problems COMMONLY USED RENAL AND URINARY TERMS • anuria Total urine output of less than 100 mL In 24 hours • azotemia Increased blood urea nitrogen and serum creatinine levels suggestive of renal impairment but without outward symptoms of renal failure • dysuria Discomfort or pain associated with micturition • frequency Feeling the need to void often, usually voiding small amounts of urine each time; may void every hour or even more frequently than hourly • hesitancy Difficulty in initiating the flow of urine, even when the bladder has sufficient urine to initiate a void and the sensation of the need to void is present COMMONLY USED RENAL AND URINARY TERMS • micturition The act of voiding • nocturia Awakening prematurely from sleep because of the need to empty the bladde • roliguria Decreased urine output; total urine output between 100 and 400 mL in 24 hours • polyuria Increased urine output; total urine output usually greater than 2000 mL in 24 hours • uremia Full-blown signs and symptoms of renal failure; sometimes referred to as the uremic syndrome, especially if the cause of the renal failure is unknown • urgency A sudden onset of the feeling of the need to void immediately; may result in incontinence if the client is unable to locate or get to toileting facilities quickly Assessment Techniques Current health problems • The client is asked about • any changes in the appearance (color, odor, clarity) of the urine, • pattern of urination, • ability to initiate or control voiding, • and other unusual symptoms. • urine color (reddish, dark brown or black, greenish, or otherwise different from the usual yellowish, straw color) • a change in odor quality, or a decrease in urine clarity • changes in urination patterns, such as nocturia, frequency, or an increase or decrease in the amount of urine. • The normal urine output for adults is 1 mL/kg/hr, or approximately 1500 to 2000 mL/day. Assessment Techniques Current health problems • The client is asked about • difficulty initiating urine flow • a burning sensation or other discomfort is present on urination • the force of the urine stream is decreased (in men) • any loss of urinary continence. Situations that increase intraabdominal pressure (e.g., coughing and sneezing) may result in the involuntary passage of urine. • a persistent dribbling of urine. Assessment Techniques Current health problems • The client is asked about • pain in the flank, in the lower abdomen or pelvic region, or in the perineal are. (the onset, intensity, and duration of the pain, its location, and its association with any activity or event). • Pain associated with renal or ureteral irritation is often severe and spasmodic. • Pain that radiates into the perineal area, groin, scrotum, or labia is described as renal colic. Renal colic pain is usually associated with distention or spasm of the ureter, such as in an obstruction or the passing of a stone. Renal colic pain may be intermittent or continuous and may even be systemic with pallor, diaphoresis, and hypotension. These general symptoms occur because of the location of the nerve tracts associated with the kidneys and ureters. • Because the kidneys are close to the GI organs and the nerve pathways are similar, GI symptoms may be part of the client's presenting history. These renointestinal reflexes often complicate the detailed description of the renal problem. • Uremia results from the accumulation of nitrogenous waste products in the blood, a result of renal failure. Symptoms include anorexia, nausea and vomiting, muscle cramps, pruritus (itching), fatigue, and lethargy. Physical Assessment • assessment of general appearance, • a general review of body systems, • specific structure and functions of the renal/urinary systems Inspection Auscultation Palpation Percussion Assessment of the urethra Physical Assessment assessment of general appearance • the general appearance of the client and checks for a yellowish skin color and the presence of any rashes, bruising, or other discoloration. • edema, which with renal disorders may be detected in the pedal (foot), pretibial (shin), sacral tissues, and around the eyes. • The lungs are auscultated to determine whether fluid is present. • Weight and blood pressure measurements are obtained for comparison purposes. • general level of consciousness and level of alertness, noting deficits in concentration, thought processes, or memory. • Family members may report subtle changes. Such cognitive changes may be the result of an insufficient clearance of waste products when renal disease is present. Physical Assessment Inspection • The nurse inspects the abdomen and the flank regions with the client in both the supine and the sitting position. • The client is observed for asymmetry (e.g., swelling) or discoloration (e.g., bruising or redness) in the flank region, especially in the area of the costovertebral angle (CVA). The CVA is located between the lower portion of the twelfth rib and the vertebral column Physical Assessment Auscultation The nurse listens for a bruit over each renal artery on the midclavicular line. A bruit is an audible swishing sound produced when the volume of blood or the diameter of the blood vessel changes. A bruit is usually associated with blood flow through a narrowed vessel, as in renal artery stenosis Physical Assessment Palpation • Renal palpation identifies masses and areas of tenderness in or around the kidney. The abdomen is lightly palpated in all quadrants. The nurse asks about areas of tenderness or discomfort and examines nontender areas first. The outline of the bladder may be seen as high as the umbilicus in clients with severe bladder distention. Special training and practice under the guidance of a qualified practitioner are necessary; therefore appropriate education is essential before attempting the procedure. If tumor or aneurysm is suspected, palpation may harm the client. • Because the kidneys are deep, posterior structures, palpation is easier in thin clients who have little abdominal musculature. For palpation of the right kidney, the client assumes a supine position while the nurse places one hand under the right flank and the other hand over the abdomen below the lower right part of the rib cage. The lower hand raises the flank, and the upper hand depresses the anterior abdomen as the client takes a deep breath. The left kidney is deeper and rarely palpable. A transplanted kidney is readily palpable in either the lower right or left abdominal quadrant. The kidney should feel smooth, firm, and nontender Physical Assessment Palpation • http://www.youtube.com/watch?v=jXmwrvi07 ME • http://www.youtube.com/watch?v=5BzbMc5w CZo&feature=related Physical Assessment Percussion –A distended bladder sounds dull when percussed. After gently palpating to determine the general outline of the distended bladder, the nurse begins percussion on the skin of the lower abdomen and continues in the direction of the umbilicus until dull sounds are no longer produced. –If the client identifies flank pain or tenderness, the nontender flank is percussed first. The client assumes a sitting, side-lying, or supine position, and the nurse forms one hand into a clenched fist. The heel of the other hand and the little finger form a flat area with which a firm thump to the CVA area can be quickly administered. Costovertebral tenderness is highly suggestive of kidney infection or inflammation. Clients with inflammation or infection in the kidney or adjacent structures may describe their pain as severe or as a constant, dull ache. Physical Assessment Assessment of the urethra Using a good light source and wearing gloves, the nurse inspects the urethra by examining the meatus and surrounding tissues. Any unusual discharge such as blood, mucus, and purulent drainage is noted. The skin and mucous membranes of surrounding tissues are inspected, and the presence of lesions, rashes, or other abnormalities of the penis or scrotum or of the labia or vaginal orifice is documented. Urethral irritation is suspected when the client reports discomfort with urination. LAB TESTS Blood Tests • Serum creatinine is a measurement of the end product of muscle and protein metabolism. Creatinine is filtered by the kidneys and excreted in the urine. Because muscle mass and metabolism are usually constant, the serum creatinine level is an excellent indicator of kidney function • ↑ indicates renal impairment. • ↓ may be caused by a decreased muscle mass • Males; 0.6-1.2 mg/dL (80-115 mmol/L) • Females: 0.5-1.1 mg/dL (44-97 mmol/L) • Older Adults: may be decreased LAB TESTS Blood Tests • Blood urea nitrogen (BUN) measures the renal excretion of urea nitrogen, a by-product of protein metabolism in the liver. Urea nitrogen is produced primarily from food sources of protein, which undergo metabolism by the liver. The kidneys filter urea nitrogen from the blood and excrete the nitrogenous waste in urine. BUN levels indicate the extent of renal clearance of this nitrogenous waste product. • ↑ may indicate hepatic or renal disease, dehydration or decreased renal perfusion, a high-protein diet, infection, stress, steroid use, Gl bleeding, or other situations in which there is blood in body tissues. • ↓ may indicate malnutrition, fluid volume excess, or severe hepatic damage • 10-20 mg/dL (2.1-7.1 mmol/L) • Older Adult: 60-90 yr; 8-23 mg/dL (2.9-8.2 mmol/L); • over 90 yr: 10-31 mg/dL (3.6-11.1 mmol/L) LAB TESTS Blood Tests • Ratio of blood urea nitrogen to serum creatinine determines whether factors such as dehydration or lack of renal perfusion are causing the elevated BUN level. When a blood volume deficit (dehydration) or hypoperfusion exists, the BUN level rises more rapidly than the serum creatinine level. As a result, the ratio of BUN to creatinine is increased. • When both the BUN and serum creatinine levels increase at the same rate, the BUN/creatinine ratio remains normal. However, the elevated serum creatinine and BUN levels suggest renal dysfunction that is not related to acute volume depletion or hypoperfusion. • Mass ratio: 12:1 to 20:1; • mole ratio: 48.5:1 to 80.8:1 • ↑ may indicate fluid volume deficit, obstructive uropathy, catabolic state, or a high-protein diet. • ↓ may indicate fluid volume excess or acute renal tubular acidosis. • No change in the ratio with increases in both the BUN and creatinine levels indicates renal impairment. LAB TESTS Urinalysis • • • • • • • Color - Pale yellow Dark amber indicates concentrated urine. Very pale yellow indicates dilute urine. Dark red or brown indicates blood in the urine; brown also may indicate increased urinary bilirubin level; red may also indicate the presence of myoglobin. Other color changes may result from diet or medications. • Odor - specific aromatic odor, similar to ammonia • Foul smell indicates possible infection, dehydration, or ingestion of certain foods or drugs. • turbidity Clear • Cloudy urine indicates infection or sediment or high levels of urinary protein LAB TESTS Urinalysis • Specific gravity measures the concentration or density of urine compared to water • Usually 1,010-1.025; (possible range 1.000-1.030;) • after 12-hr fluid restriction > 1.025 • Older adult; Decreased because of decreased concentrating ability • ↑ with dehydration, decreased kidney perfusion, or the presence of antidiuretic hormone (ADH). In each of these situations the expected kidney response is to reabsorb water and decrease urine output. As a result, the urine produced is more concentrated. • ↓ in specific gravity occurs with increased fluid intake, diuretic administration, and diabetes insidious. In each of these situations, the normal kidney response is to excrete more water; thus urine output is increased. • ↓ in kidney disease (chronic renal insufficiency, diabetes insipidus, malignant hypertension, diuretic administration, and lithium toxicity), the specific gravity decreases because there is less solute, and it does not vary with changes in plasma osmolality LAB TESTS Urinalysis • pH Average: 6; possible range: 4.6-8 • Changes are caused by diet, the administration of medications, infection, freshness of the specimen, acid-base imbalance, and altered renal function. • Glucose is filtered at the glomerulus and is reabsorbed in the proximal tubule of the nephron. When the blood glucose level rises above 220 mg/dL, the renal threshold for reabsorption is usually exceeded, and glucose is excreted in the urine • <0.5 g/day (<2.78 mmol/L) • Presence reflects hyperglycemia or a decrease in the renal threshold for glucose. • Ketone bodies absent • Presence reflects incomplete metabolism of fatty acids, as in diabetic ketoacidosis, prolonged fasting, anorexia nervosa LAB TESTS Urinalysis • Protein is not normally present 8-18 mg/dL (10-140 mg/L) • ↑ may indicate stress, infection, recent strenuous exercise, or glomerular disorders • The glomerular membrane is semipermeable to small molecules; protein molecules are too large to pass through this semipermeable membrane. When permeability of the glomerular membrane is increased, protein molecules pass through and are excreted in the urine. Increased glomerular membrane permeability may be caused by infection, inflammation, or immunologic problems. • Certain systemic processes result in the production of abnormal proteins, such as globulin. These proteins are not detected with routine urinalysis procedures; urine protein electrophoresis or other tests are necessary to detect these unusual proteins. • Microalbuminuria is the presence of albumin in the urine that is not measurable by a urine dipstick or conventional urinalysis procedures. Specialized immunoassay tests can quickly analyze a freshly voided urine specimen for microscopic levels of albumin. • The normal microalbumin levels in a freshly voided random specimen should range between 2.0 to 20 mg/mmol for men and 2.8 to 28 mg/mmol for women. • Higher levels indicate microalbuminuria and could mean the presence of very early kidney disease, especially in clients with diabetes mellitus. • For 24-hour urine specimens, levels of 30 to 300 mg/24 hr, or 20 to 200 xg/min, indicate microalbuminuria. LAB TESTS Urinalysis • • • • • Bilirubin (urobilinogen) None Presence suggests hepatic or biliary disease or obstruction. Cells Types of cells abnormally present in the urine may include: tubular cells (from the tubule of the nephron), epithelial cells (from the lining of the urinary tract), red blood cells (RBCs), 0-2 per high-power field ↑ are normal with indwelling or intermittent catheterization or menses but may reflect tumor, stones, trauma, glomerular disorders, cystitis, or bleeding disorders. white blood cells (WBCs) Males: 0-3 per high-power field, Females: 0-5 per high-power field ↑ amounts may indicate an infectious or inflammatory process anywhere in the renal/urinary tract, renal transplant rejection, fever, or exercise. Casts are described by the type of element in the structure (e.g., RBC cast, WBC cast, tubular epithelial cast) or the stage of degeneration. The degeneration of casts refers to the stage of breakdown of the internal element. Casts are described as "granular" (coarse or fine) and "waxy.“ ↑ indicate the presence of bacteria or protein, which is seen in severe renal disease and could also indicate urinary calculi LAB TESTS Urinalysis • crystals in the urine come from various salts. These particles may be a result of diet, drags, or disease. The salts may be composed of calcium, oxalate, urea, phosphate, magnesium, or other substances. Certain drugs, such as the sulfates, can also produce crystals. None • Presence of normal or abnormal crystals may indicate that the specimen has been allowed to stand • Bacteria in a urine sample multiply quickly, so the specimen must be analyzed promptly. • Normally urine is sterile or <1000 colonies/mL, but it can be contaminated easily by perineal bacteria or airborne pathogens during collection • Increased amounts indicate the need for urine culture to determine the presence of urinary tract infection. • Presence of Trichomonas vaginalis indicates infection, usually of the urethra, prostate, or vagina Other Urine Tests • Urine for culture and sensitivity - determination of the number and types of pathogens. When bacterial colonies are present, they are placed in a medium containing different antibiotic drugs to determine which drugs are effective in killing or stopping the growth of the bacteria (sensitivity) • Composite urine collections quantitative and qualitative analysis of one or more substances (urinary creatinine or urea nitrogen, sodium, chloride, calcium, catecholamines, or other components) Other Urine Tests • • • • • • • • • • • Creatinine clearance is a calculation of glomerular filtration rate. It is the best indication of overall kidney function. The amount of creatinine cleared from the blood (e.g., filtered into the urine) is measured in the total volume of urine excreted in a defined period. A urine specimen for a creatinine clearance test is usually collected for 24 hours, but it can be collected for shorter periods (e.g., 8 or 12 hours). The calculation requires a comparison with the blood creatinine level, and therefore a blood specimen for creatinine must also be collected. The laboratory or the physician calculates the creatinine clearance. Because the client's age, gender, height, weight, diet, and activity level influence the expected amount of creatinine to be excreted, these variables are considered in the interpretation of creatinine clearance test results. The following formula is used to calculate creatinine clearance: Creatinine clearance = U x V/P x T where U is creatinine in urine (mg/dL), V is volume of urine (mL/24 hr), P is creatinine in plasma or blood (mg/dL), and T is time (minutes). The rate of creatinine clearance is expressed as milliliters per minute per 1.73 m2 of body surface area. The range for normal creatinine clearance is 90 to 139 mL/min for adult males and 80 to 125 mL/min for females. Creatinine clearance measurements are necessary to determine the client's current kidney function. Decreases in the creatinine clearance rate may require modification of drug dosing and often signifies the need for further investigation of the cause of kidney deterioration Urine electrolytes Osmolarity, blood/plasma osmolarity, urine osmolarity Osmolality is a measure of the concentration of particles in solution, in this case the concentration of solutes in urine. These solutes include electrolytes and solutes such as glucose, urea, and creatinine Radiological examination • Kidney, ureter, and bladder x-rays – to screen for the presence of two kidneys, to measure the kidneys' size, shape, relaionship to other parts of the urinary tract, to detect gross obstruction • Computed tomography - measuring the size of the kidneys, evaluating contour to assess for masses or obstruction • Intravenous urography (Excretory urography) - to measure the kidneys' size, to detect obstruction, to assess parenchymal mass • Bowel preparation, allergy information Intravenous urography • Intravenous urography demonstrating crossed renal ectopy. The "left" kidney is located below the right kidney. Cystography and Cystourethrography • Instilling dye into bladder via urethral catheter • Voiding cystourethrogram • Monitoring for infection • Encouraging fluid intake • Monitoring for changes in urine output and for development of infection from catheter placement Renal Arteriography (Angiography) • Possible bowel preparation • Light meal evening before, then nothing by mouth • Injection of radiopaque dye into renal arteries • Assessment for bleeding • Monitoring of vital signs • Absolute bedrest for 4 to 6 hours • Serum creatinine measured for several days to assess effects of test Renal Biopsy • Percutaneous kidney biopsy • Clotting studies • Preprocedure care • Follow-up care – Assessment for bleeding for 24 hours – Strict bedrest – Monitoring for hematuria – Comfort measures Renography • Small amount of radioactive material, a radionuclide, used • Procedure via intravenous infection • Follow-up care: – Small amount of radioactive material may be excreted. – Maintain standard precautions. – Client should avoid changing posture rapidly and avoid falling. Ultrasonography • Bedside sonography/bladder scanners checking postvoid residual volumes and determine the need for intermittent catheterization based on the amount of urine in the bladder. Cystoscopy and cystourethroscopy Procedure is invasive. – Consent is required. – Postprocedure care includes monitoring for airway patency, vital signs, and urine output. – Monitor for bleeding and infection. – Encourage client to take oral fluids. Cystoscopy • http://www.youtube.com/watch?v=iLeqYPJy G_A Retrograde Procedures • Retrograde procedures go against the normal flow of urine. • Procedure identifies obstruction or structural abnormalities with the instillation of dye into lower urinary tract. • Monitor for infection. • Follow-up care is the same as for a cystoscopic examination. Urodynamic Studies • Studies that examine the process of voiding include: – Cystometrography – Urethral pressure profile – Electromyography – Urine stream test